Abstract
Rev Bras Ter Intensiva. 2022;34(4):499-506
DOI 10.5935/0103-507X.20220080-en
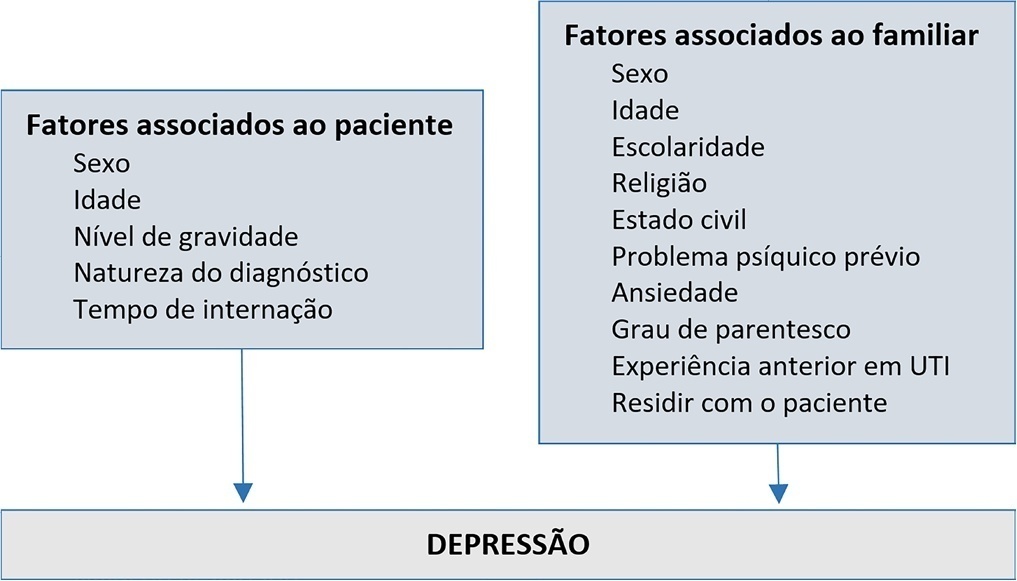
To evaluate the prevalence and factors associated with depression in family members of people hospitalized in intensive care units.
A cross-sectional study was conducted with 980 family members of patients admitted to the intensive care units of a large public hospital in the interior of Bahia. Depression was measured using the Patient Health Questionnaire-8. The multivariate model consisted of the following variables: sex and age of the patient, sex and age of the family member, education level, religion, living with the family member, previous mental illness and anxiety.
Depression had a prevalence of 43.5%. In the multivariate analysis, the model with the best representativeness indicated that factors associated with a higher prevalence of depression were being female (39%), age younger than 40 years (26%) and previous mental illness (38%). A higher education level was associated with a 19% lower prevalence of depression in family members.
The increase in the prevalence of depression was associated with female sex, age younger than 40 years and previous psychological problems. Such elements should be valued in actions aimed at family members of people hospitalized in intensive care.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):231-242
DOI 10.5935/0103-507X.20210030
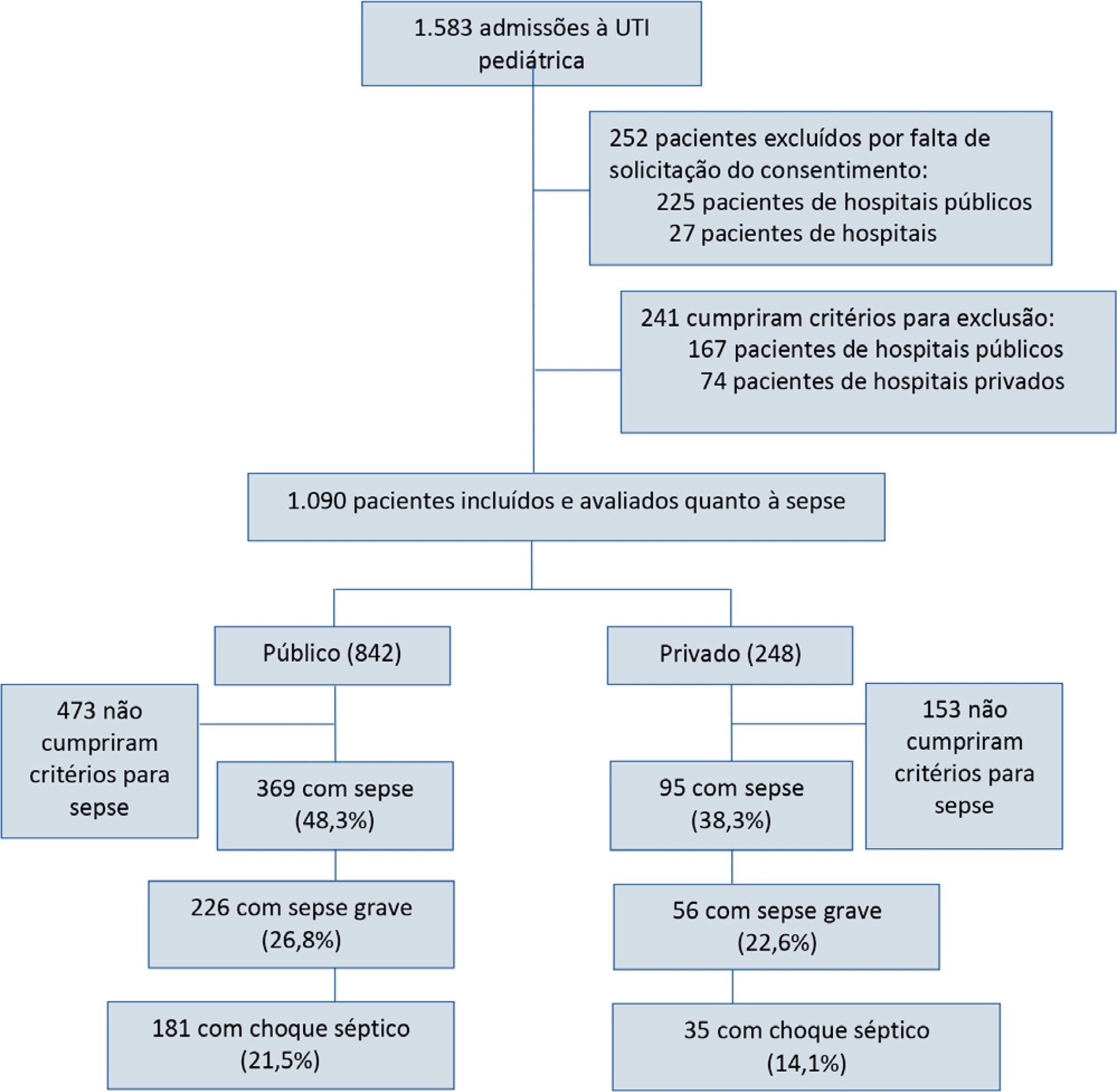
To report the prevalence and outcomes of sepsis in children admitted to public and private hospitals.
Post hoc analysis of the Latin American Pediatric Sepsis Study (LAPSES) data, a cohort study that analyzed the prevalence and outcomes of sepsis in critically ill children with sepsis on admission at 21 pediatric intensive care units in five Latin American countries.
Of the 464 sepsis patients, 369 (79.5%) were admitted to public hospitals and 95 (20.5%) to private hospitals. Compared to those admitted to private hospitals, sepsis patients admitted to public hospitals did not differ in age, sex, immunization status, hospital length of stay or type of admission but had higher rates of septic shock, higher Pediatric Risk of Mortality (PRISM), Pediatric Index of Mortality 2 (PIM 2), and Pediatric Logistic Organ Dysfunction (PELOD) scores, and higher rates of underlying diseases and maternal illiteracy. The proportion of patients admitted from pediatric wards and sepsis-related mortality were higher in public hospitals. Multivariate analysis did not show any correlation between mortality and the type of hospital, but mortality was associated with greater severity on pediatric intensive care unit admission in patients from public hospitals.
In this sample of critically ill children from five countries in Latin America, the prevalence of septic shock within the first 24 hours at admission and sepsis-related mortality were higher in public hospitals than in private hospitals. Higher sepsis-related mortality in children admitted to public pediatric intensive care units was associated with greater severity on pediatric intensive care unit admission but not with the type of hospital. New studies will be necessary to elucidate the causes of the higher prevalence and mortality of pediatric sepsis in public hospitals.
Abstract
Rev Bras Ter Intensiva. 2021;33(1):88-95
DOI 10.5935/0103-507X.20210009
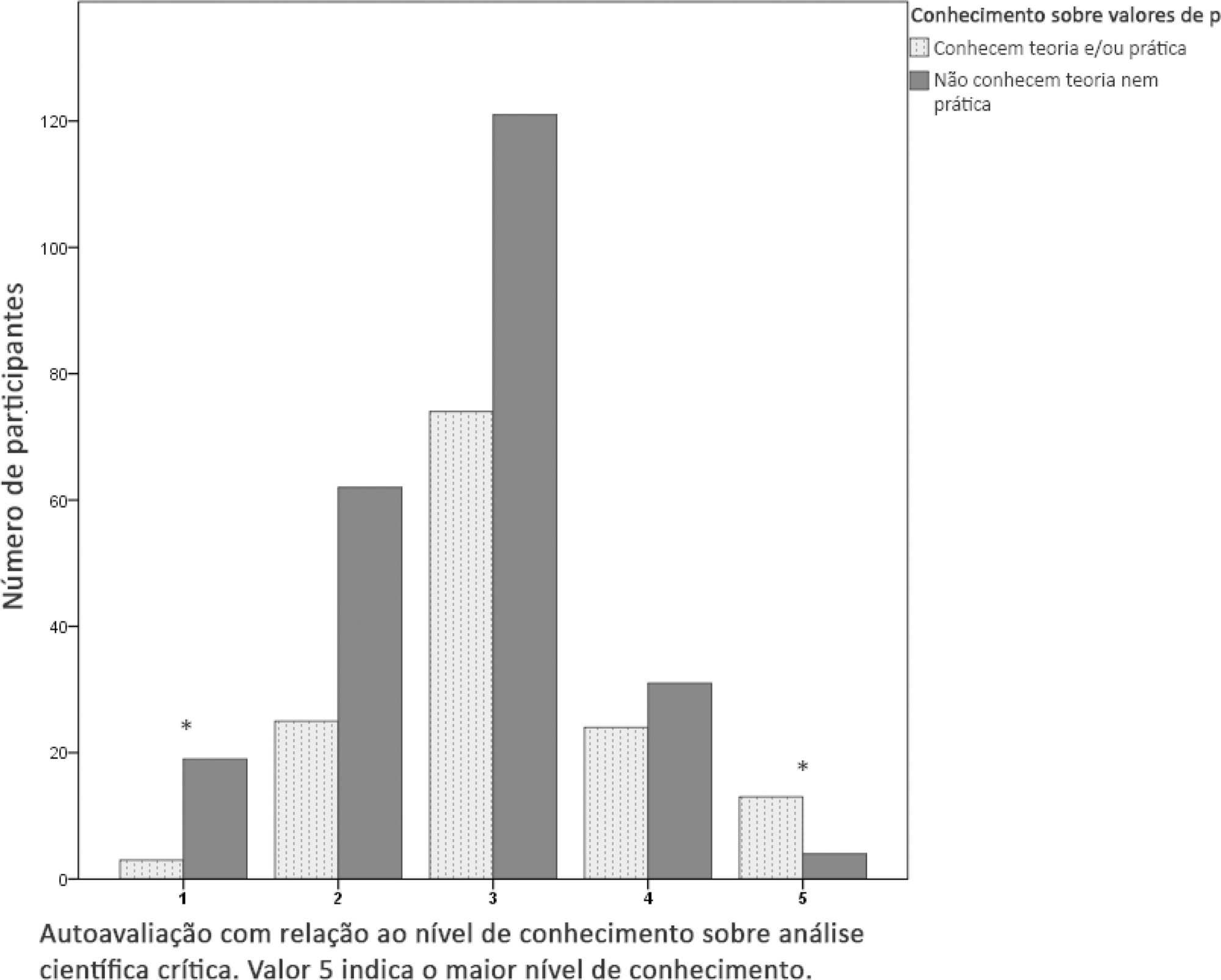
To determine the prevalence of and risk factors for insufficient knowledge related to p-values among critical care physicians and respiratory therapists in Argentina.
This cross-sectional online survey contained 25 questions about respondents’ characteristics, self-perception and p-value knowledge (theory and practice). Descriptive and multivariable logistic regression analyses were conducted.
Three hundred seventy-six respondents were analyzed. Two hundred thirty-seven respondents (63.1%) did not know about p-values. According to the multivariable logistic regression analysis, a lack of training on scientific research methodology (adjusted OR 2.50; 95%CI 1.37 - 4.53; p = 0.003) and the amount of reading (< 6 scientific articles per year; adjusted OR 3.27; 95%CI 1.67 - 6.40; p = 0.001) were found to be independently associated with the respondents’ lack of p-value knowledge.
The prevalence of insufficient knowledge regarding p-values among critical care physicians and respiratory therapists in Argentina was 63%. A lack of training on scientific research methodology and the amount of reading (< 6 scientific articles per year) were found to be independently associated with the respondents’ lack of p-value knowledge.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):458-467
DOI 10.5935/0103-507X.20200076
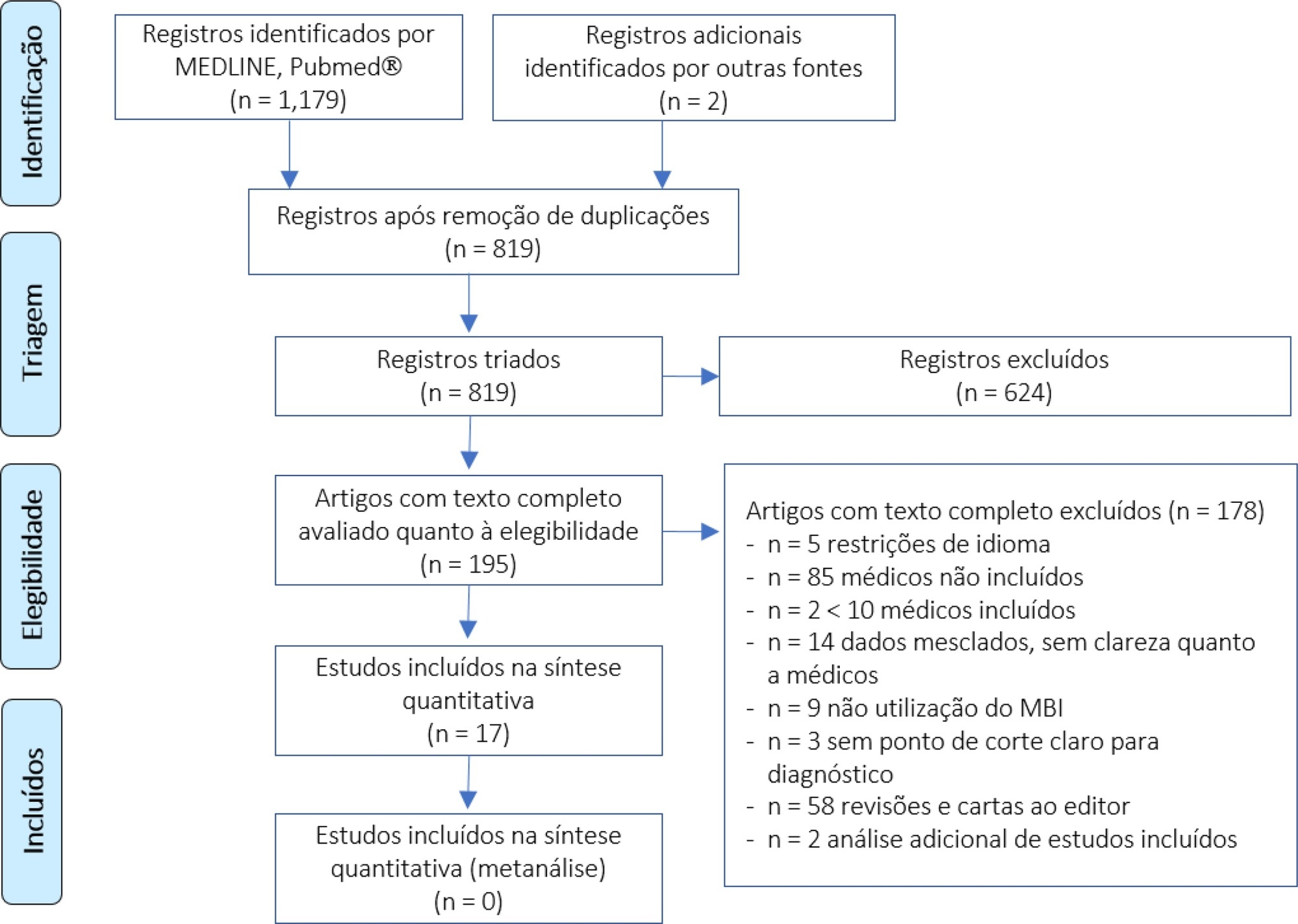
We performed a systematic review to summarize the knowledge regarding the prevalence of burnout among intensive care unit physicians.
We conducted a systematic review of the MEDLINE and PubMed® databases (last update 04.02.2019) with the goal of summarizing the evidence on burnout among intensive care unit physicians. We included all studies reporting burnout in intensive care unit personnel according to the Maslach Burnout Inventory questionnaire and then screened studies for data on burnout among intensive care unit physician specifically.
We found 31 studies describing burnout in intensive care unit staff and including different healthcare profiles. Among these, 5 studies focused on physicians only, and 12 others investigated burnout in mixed intensive care unit personnel but provided separate data on physicians. The prevalence of burnout varied greatly across studies (range 18% - 49%), but several methodological discrepancies, among them cut-off criteria for defining burnout and variability in the Likert scale, precluded a meaningful pooled analysis.
The prevalence of burnout syndrome among intensive care unit physicians is relatively high, but significant methodological heterogeneities warrant caution being used in interpreting our results. The lower reported levels of burnout seem higher than those found in studies investigating mixed intensive care unit personnel. There is an urgent need for consensus recommending a consistent use of the Maslach Burnout Inventory test to screen burnout, in order to provide precise figures on burnout in intensive care unit physicians.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):270-277
DOI 10.5935/0103-507X.20160053
To estimate the prevalence of burnout in intensivist doctors working in adult, pediatric and neonatal intensive care units in five Brazilian capitals.
Descriptive epidemiological study with a random sample stratified by conglomerate with 180 intensivist doctors from five capitals representing the Brazilian geographic regions: Porto Alegre (RS), Sao Paulo (SP), Salvador (BA), Goiania (GO) and Belem (PA). A self-administered questionnaire examining sociodemographic data and the level of burnout was evaluated through the Maslach Burnout Inventory.
A total of 180 doctors were evaluated, of which 54.4% were female. The average age was 39 ± 8.1 years, 63.4% had specialization as the highest degree, 55.7% had up to 10 years of work experience in an intensive care unit, and 46.1% had the title intensive care specialist. Most (50.3%) had weekly workloads between 49 and 72 hours, and the most frequent employee type was salaried. High levels of emotional exhaustion, depersonalization and inefficacy were found (50.6%, 26.1% and 15.0%, respectively). The prevalence of burnout was 61.7% when considering a high level in at least one dimension and 5% with a high level in three dimensions simultaneously.
A high prevalence of burnout syndrome among intensivist doctors was observed. Strategies for the promotion and protection of health in these workers must be discussed and implemented in hospitals.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):143-150
DOI 10.1590/S0103-507X2012000200008
OBJECTIVE: To determine the prevalence of infections in Brazilian intensive care units and the associated mortality by analyzing the data obtained in the Extended Prevalence of Infection in Intensive Care (EPIC II) study. METHODS: EPIC II was a multicenter, international, cross-sectional prospective study of infection prevalence. It described the demographic, physiological, bacteriological, and therapeutic characteristics, outcome up to the 60th day, prevalence of infection, and mortality of all the patients admitted to the participating ICUs between zero hour and midnight on May 8, 2007. A total of 14,414 patients were included in the original study. Of these 14,414 patients, 1,235 were Brazilian and were hospitalized in 90 Brazilian ICUs. They represent the focus of this study. RESULTS: Among these 1,235 Brazilian patients, 61,6% had an infection on the day of the trial, and the lungs were the main site of infection (71.2%). Half of the patients had positive cultures, predominantly gram-negative bacilli (72%). On the day of the study, the median SOFA score was 5 (3-8) and the median SAPS II score was 36 (26-47). The infected patients had SOFA scores significantly higher than those of the non-infected patients 6 (4-9) and 3 (2-6), respectively). The overall ICU mortality rate was 28.4%: 37.6% in the infected patients, and 13.2% in the non-infected patients (p<0.001). Similarly, the in-hospital mortality rate was 34.2%, with a higher rate in the infected than in the non-infected patients (44.2% vs. 17.7%) (p<0.001). In the multivariate analysis, the main factors associated with infection incidence were emergency surgery (OR 2.89, 95%CI [1.72-4.86], p<0.001), mechanical ventilation (OR 2.06, 95% CI [1.5-2.82], p<0.001), and the SAPS II score (OR 1.04, 95% CI [1.03-1.06], p<0.001). The main factors related to mortality were ICC functional class III/ IV (OR 3.0, 95% CI [1.51-5.98], p<0.01), diabetes mellitus (OR 0.48, 95% CI [0.25-0.95], p<0.03), cirrhosis (OR 4.62, 95% CI [1.47-14,5], p<0.01), male gender (OR 0.68, 95% CI [0.46-1.0], p<0.05), mechanical ventilation (OR 1.87, 95% CI [1.19-2.95], p<0.01), hemodialysis (OR 1.98, 95% CI [1.05-3.75], p<0.03), and the SAPS II score (OR 1.08, 95% CI [1.06-1.10], p<0.001). CONCLUSION: The present study revealed a higher prevalence of infections in Brazilian ICUs than has been previously reported. There was a clear association between infection and mortality.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):414-420
DOI 10.1590/S0103-507X2007000400002
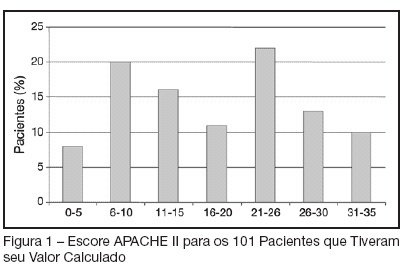
BACKGROUND AND OBJECTIVES: To determine the prevalence of intensive care unit (ICU)-acquired infections and the risk factors for these infections, identify the predominant infecting organisms, and evaluate the relationship between ICU-acquired infection and mortality. METHODS: A 1-day point prevalence study. Sixteen ICU of the State of Rio Grande do Sul-Brazil, excluding coronary care and pediatric units. All patients < 12 yrs occupying an ICU bed over a 24-hour period. The 16 ICU provided 174 case reports. Main outcomes: rates of ICU-acquired infection, resistance patterns of microbiological isolates, and potential risks factors for ICU-acquired infection and death. RESULTS: A total of 122 patients (71%) was infected and 51 (29%) had ICU-acquired infection. Pneumonia (58.2%), lower tract respiratory infection (22.9%), urinary tract infection (18%) were the most frequents types of ICU infection. Most frequently microorganisms reported were staphylococcus aureus (42% [64% resistant to oxacilin]) and pseudomonas aeruginosa (31%). Six risk factors for ICU acquired infection were identified: urinary catheterization, central vascular line, tracheal intubation for prolonged time (> 4 days), chronic disease and increased length of ICU stay (> 30 days). The risks factors associated with death were age, APACHE II, organ dysfunction, and tracheal intubation with or without mechanical ventilation. CONCLUSIONS: ICU-acquired infection is common and often associated with microbiological isolates of resistant organisms. This study may serve as an epidemiological reference to help the discussion of regional infection control policies.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)