You searched for:"Eduardo Juan Troster"
We found (4) results for your search.-
Letter to the Editor
Methemoglobinemia induced by dapsone in a pediatric patient: case report
Crit Care Sci. 2023;35(2):233-235
Abstract
Letter to the EditorMethemoglobinemia induced by dapsone in a pediatric patient: case report
Crit Care Sci. 2023;35(2):233-235
DOI 10.5935/2965-2774.20230018-pt
Views5INTRODUCTIONMethemoglobinemia is a rare condition and one of the differential diagnoses of cyanosis in the pediatric age group.() Clinical symptoms vary according to the levels of methemoglobin (MetHb) in the blood and may be nonspecific. The most common symptoms are central cyanosis, headache, fatigue, and respiratory depression.() Therefore, it is essential to recognize and treat […]See more -
Original Article
Prevalence and outcomes of sepsis in children admitted to public and private hospitals in Latin America: a multicenter observational study
Rev Bras Ter Intensiva. 2021;33(2):231-242
Abstract
Original ArticlePrevalence and outcomes of sepsis in children admitted to public and private hospitals in Latin America: a multicenter observational study
Rev Bras Ter Intensiva. 2021;33(2):231-242
DOI 10.5935/0103-507X.20210030
Views0ABSTRACT
Objective:
To report the prevalence and outcomes of sepsis in children admitted to public and private hospitals.
Methods:
Post hoc analysis of the Latin American Pediatric Sepsis Study (LAPSES) data, a cohort study that analyzed the prevalence and outcomes of sepsis in critically ill children with sepsis on admission at 21 pediatric intensive care units in five Latin American countries.
Results:
Of the 464 sepsis patients, 369 (79.5%) were admitted to public hospitals and 95 (20.5%) to private hospitals. Compared to those admitted to private hospitals, sepsis patients admitted to public hospitals did not differ in age, sex, immunization status, hospital length of stay or type of admission but had higher rates of septic shock, higher Pediatric Risk of Mortality (PRISM), Pediatric Index of Mortality 2 (PIM 2), and Pediatric Logistic Organ Dysfunction (PELOD) scores, and higher rates of underlying diseases and maternal illiteracy. The proportion of patients admitted from pediatric wards and sepsis-related mortality were higher in public hospitals. Multivariate analysis did not show any correlation between mortality and the type of hospital, but mortality was associated with greater severity on pediatric intensive care unit admission in patients from public hospitals.
Conclusion:
In this sample of critically ill children from five countries in Latin America, the prevalence of septic shock within the first 24 hours at admission and sepsis-related mortality were higher in public hospitals than in private hospitals. Higher sepsis-related mortality in children admitted to public pediatric intensive care units was associated with greater severity on pediatric intensive care unit admission but not with the type of hospital. New studies will be necessary to elucidate the causes of the higher prevalence and mortality of pediatric sepsis in public hospitals.
Keywords:ChildCritical illnessHospital, privateHospital, publicIntensive care unitsIntensive care units, pediatricLatin AmericaMortalityprevalenceSepsisSeptic shockSee more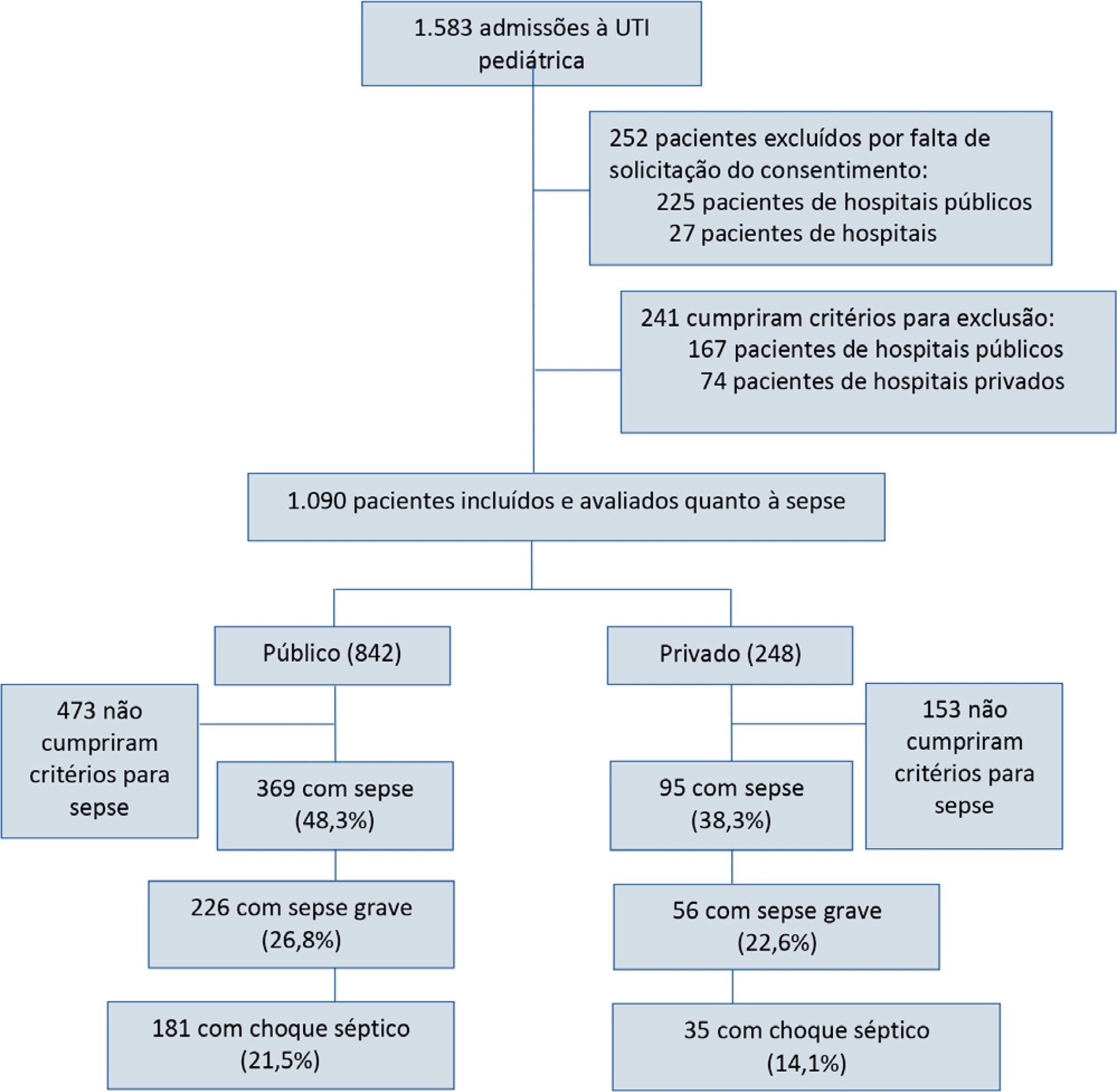
-
Letter to the Editor
To: Acute kidney injury and intra-abdominal hypertension in burn patients in intensive care
Rev Bras Ter Intensiva. 2019;31(2):271-272
Abstract
Letter to the EditorTo: Acute kidney injury and intra-abdominal hypertension in burn patients in intensive care
Rev Bras Ter Intensiva. 2019;31(2):271-272
DOI 10.5935/0103-507X.20190022
Views0To the Editor The difficulty of managing fluid in severely burned patients and the fact that monitoring intra-abdominal pressure (IAP) is not yet a routine intensive care therapy makes the article by Talizin et al.() mandatory reading, especially for professionals working with this group of patients.[…]See more
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




