Abstract
Rev Bras Ter Intensiva. 2020;32(4):521-527
DOI 10.5935/0103-507X.20200089
To compare the performance of the Simplified Acute Physiology Score 3 (SAPS 3) in patients with and without solid cancer who were admitted to the intensive care unit of a comprehensive oncological hospital in Brazil.
We performed a retrospective cohort analysis of our administrative database of the first admission of adult patients to the intensive care unit from 2012 to 2016. The patients were categorized according to the presence of solid cancer. We evaluated discrimination using the area under the Receiver Operating Characteristic curve (AUROC) and calibration using the calibration belt approach.
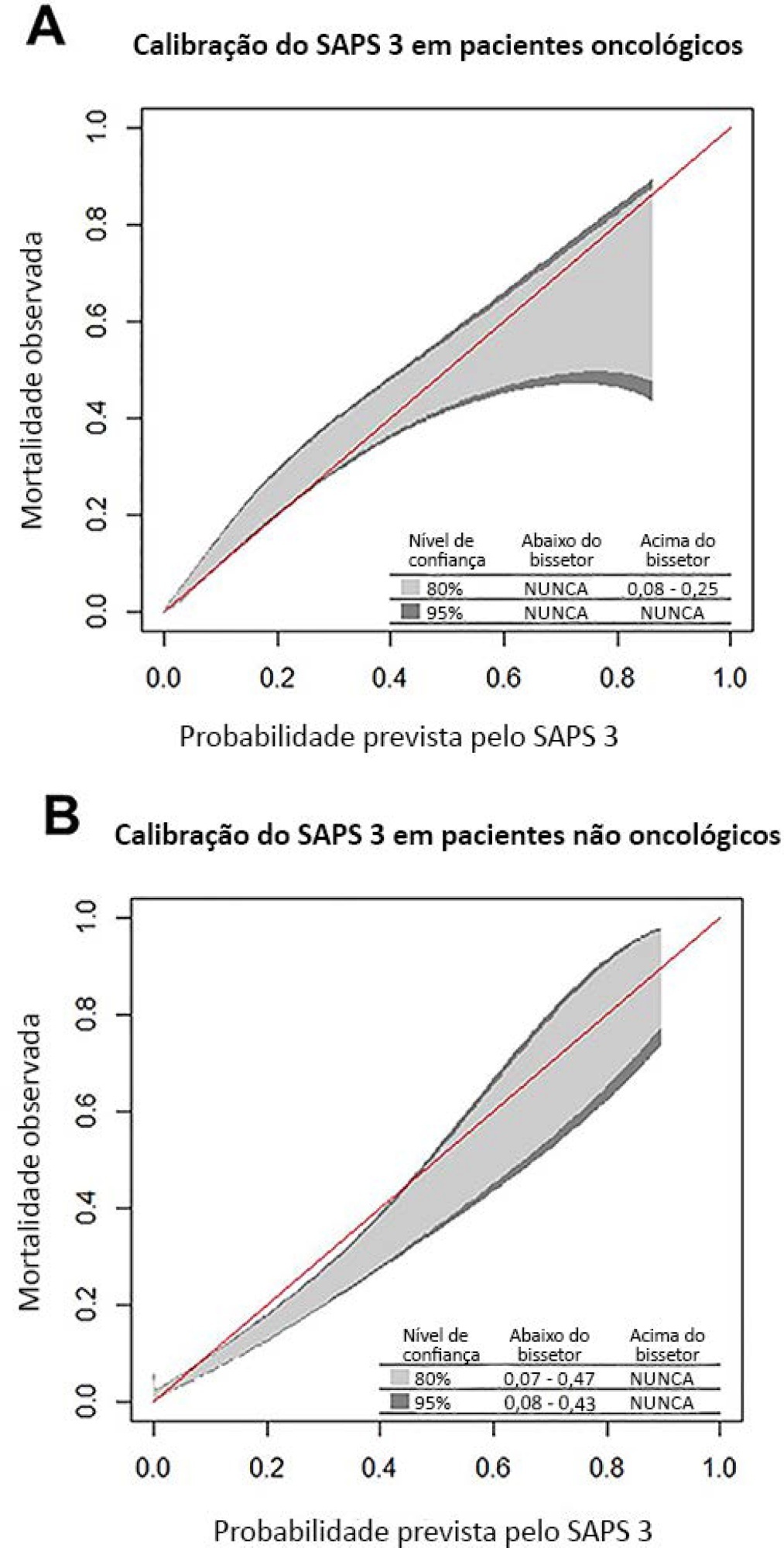
We included 7,254 patients (41.5% had cancer, and 12.1% died during hospitalization). Oncological patients had higher hospital mortality than nononcological patients (14.1% versus 10.6%, respectively; p < 0.001). SAPS 3 discrimination was better for oncological patients (AUROC = 0.85) than for nononcological patients (AUROC = 0.79) (p < 0.001). After we applied the calibration belt in oncological patients, the SAPS 3 matched the average observed rates with a confidence level of 95%. In nononcological patients, the SAPS 3 overestimated mortality in those with a low-middle risk. Calibration was affected by the time period only for nononcological patients.
SAPS 3 performed differently between oncological and nononcological patients in our single-center cohort, and variation over time (mainly calibration) was observed. This finding should be taken into account when evaluating severity-of-illness score performance.