You searched for:"José Artur Paiva"
We found (7) results for your search.-
Original Article
Neurocritical care management supported by multimodal brain monitoring after acute brain injury
Crit Care Sci. 2023;35(2):196-202
Abstract
Original ArticleNeurocritical care management supported by multimodal brain monitoring after acute brain injury
Crit Care Sci. 2023;35(2):196-202
DOI 10.5935/2965-2774.20230036-pt
Views10ABSTRACT
Objective:
To evaluate the association between different intensive care units and levels of brain monitoring with outcomes in acute brain injury.
Methods:
Patients with traumatic brain injury and subarachnoid hemorrhage admitted to intensive care units were included. Neurocritical care unit management was compared to general intensive care unit management. Patients managed with multimodal brain monitoring and optimal cerebral perfusion pressure were compared with general management patients. A good outcome was defined as a Glasgow outcome scale score of 4 or 5.
Results:
Among 389 patients, 237 were admitted to the neurocritical care unit, and 152 were admitted to the general intensive care unit. Neurocritical care unit management patients had a lower risk of poor outcome (OR = 0.228). A subgroup of 69 patients with multimodal brain monitoring (G1) was compared with the remaining patients (G2). In the G1 and G2 groups, 59% versus 23% of patients, respectively, had a good outcome at intensive care unit discharge; 64% versus 31% had a good outcome at 28 days; 76% versus 50% had a good outcome at 3 months (p < 0.001); and 77% versus 58% had a good outcome at 6 months (p = 0.005). When outcomes were adjusted by SAPS II severity score, using good outcome as the dependent variable, the results were as follows: for G1 compared to G2, the OR was 4.607 at intensive care unit discharge (p < 0.001), 4.22 at 28 days (p = 0.001), 3.250 at 3 months (p = 0.001) and 2.529 at 6 months (p = 0.006). Patients with optimal cerebral perfusion pressure management (n = 127) had a better outcome at all points of evaluation. Mortality for those patients was significantly lower at 28 days (p = 0.001), 3 months (p < 0.001) and 6 months (p = 0.001).
Conclusion:
Multimodal brain monitoring with autoregulation and neurocritical care unit management were associated with better outcomes and should be considered after severe acute brain injury.
Keywords:Acute brain injuryAutoregulationCritical care outcomeIntensive care unitsMultimodal brain monitoringOptimal cerebral perfusion pressurePrognosisSee more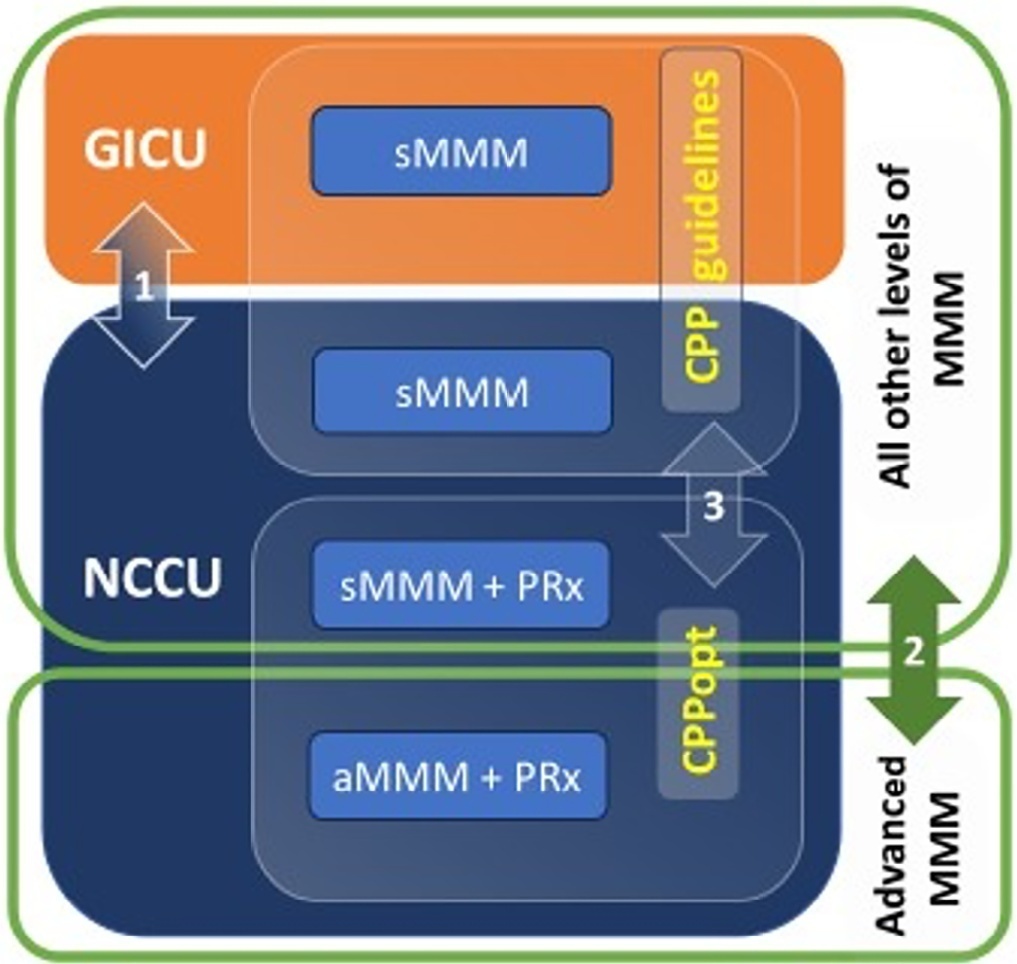
-
Original Article
Critical COVID-19 and neurological dysfunction – a direct comparative analysis between SARS-CoV-2 and other infectious pathogens
Rev Bras Ter Intensiva. 2022;34(3):342-350
Abstract
Original ArticleCritical COVID-19 and neurological dysfunction – a direct comparative analysis between SARS-CoV-2 and other infectious pathogens
Rev Bras Ter Intensiva. 2022;34(3):342-350
DOI 10.5935/0103-507X.20220229-en
Views8ABSTRACT
Objective:
To evaluate whether critical SARS-CoV-2 infection is more frequently associated with signs of corticospinal tract dysfunction and other neurological signs, symptoms, and syndromes, than other infectious pathogens.
Methods:
This was a prospective cohort study with consecutive inclusion of patients admitted to intensive care units due to primary infectious acute respiratory distress syndrome requiring invasive mechanical ventilation > 48 hours. Eligible patients were randomly assigned to three investigators for clinical evaluation, which encompassed the examination of signs of corticospinal tract dysfunction. Clinical data, including other neurological complications and possible predictors, were independently obtained from clinical records.
Results:
We consecutively included 54 patients with acute respiratory distress syndrome, 27 due to SARS-CoV-2 and 27 due to other infectious pathogens. The groups were comparable in most characteristics. COVID-19 patients presented a significantly higher risk of neurological complications (RR = 1.98; 95%CI 1.23 – 3.26). Signs of corticospinal tract dysfunction tended to be more prevalent in COVID-19 patients (RR = 1.62; 95%CI 0.72 – 3.44).
Conclusion:
Our study is the first comparative analysis between SARS-CoV-2 and other infectious pathogens, in an intensive care unit setting, assessing neurological dysfunction. We report a significantly higher risk of neurological dysfunction among COVID-19 patients. As such, we suggest systematic screening for neurological complications in severe COVID-19 patients.
Keywords:Coronavirus infectionsCOVID-19Intensive careNeurological manifestationsPyramidal tractRespiratory distress syndromeSARS-CoV-2See more -
Original Article
Prognostic value of hyperlactatemia in infected patients admitted to intensive care units: a multicenter study
Rev Bras Ter Intensiva. 2022;34(1):154-162
Abstract
Original ArticlePrognostic value of hyperlactatemia in infected patients admitted to intensive care units: a multicenter study
Rev Bras Ter Intensiva. 2022;34(1):154-162
DOI 10.5935/0103-507X.20220010-en
Views1See moreABSTRACT
Objective:
To evaluate the influence of patient characteristics on hyperlactatemia in an infected population admitted to intensive care units and the influence of hyperlactatemia severity on hospital mortality.
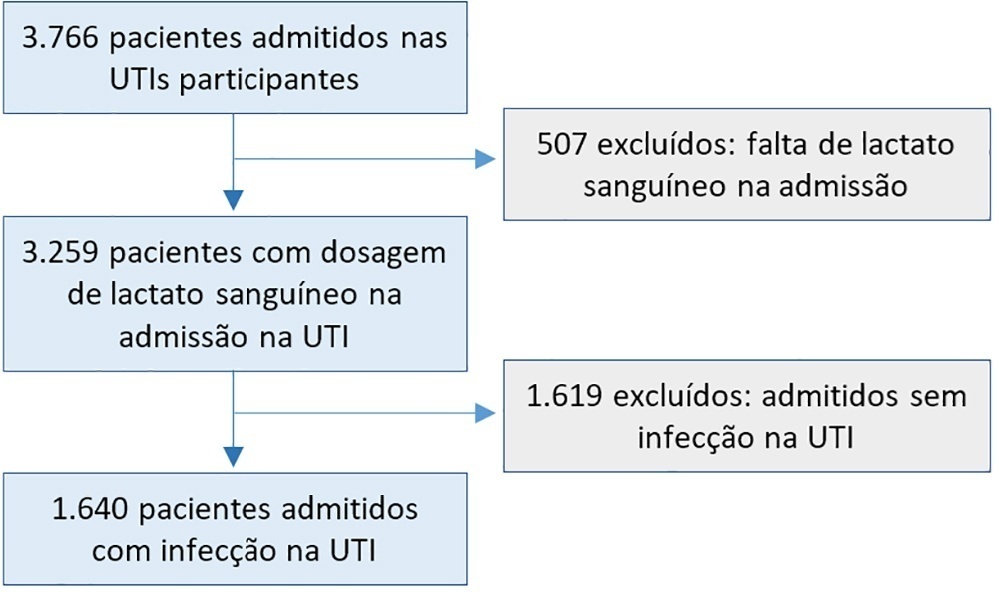
Methods:
A post hoc analysis of hyperlactatemia in the INFAUCI study, a national prospective, observational, multicenter study, was conducted in 14 Portuguese intensive care units. Infected patients admitted to intensive care units with a lactate measurement in the first 12 hours of admission were selected. Sepsis was identified according to the Sepsis-2 definition accepted at the time of data collection. The severity of hyperlactatemia was classified as mild (2 – 3.9mmol/L), moderate (4.0 – 9.9mmol/L) or severe (> 10mmol/L).
Results:
In a total of 1,640 patients infected on admission, hyperlactatemia occurred in 934 patients (57%), classified as mild, moderate and severe in 57.0%, 34.4% and 8.7% of patients, respectively. The presence of hyperlactatemia and a higher degree of hyperlactatemia were both associated with a higher Simplified Acute Physiology Score II, a higher Charlson Comorbidity Index and the presence of septic shock. The lactate Receiver Operating Characteristic curve for hospital mortality had an area under the curve of 0.64 (95%CI 0.61 – 0.72), which increased to 0.71 (95%CI 0.68 – 0.74) when combined with Sequential Organ Failure Assessment score. In-hospital mortality with other covariates adjusted by Simplified Acute Physiology Score II was associated with moderate and severe hyperlactatemia, with odds ratio of 1.95 (95%CI 1.4 – 2.7; p < 0.001) and 4.54 (95%CI 2.4 - 8.5; p < 0.001), respectively.
Conclusion:
Blood lactate levels correlate independently with in-hospital mortality for moderate and severe degrees of hyperlactatemia.
-
Special Article
Update of the recommendations of the Sociedade Portuguesa de Cuidados Intensivos and the Infection and Sepsis Group for the approach to COVID-19 in Intensive Care Medicine
Rev Bras Ter Intensiva. 2021;33(4):487-536
Abstract
Special ArticleUpdate of the recommendations of the Sociedade Portuguesa de Cuidados Intensivos and the Infection and Sepsis Group for the approach to COVID-19 in Intensive Care Medicine
Rev Bras Ter Intensiva. 2021;33(4):487-536
DOI 10.5935/0103-507X.0103-507X-rbti-20210080
Views0ABSTRACT
Introduction:
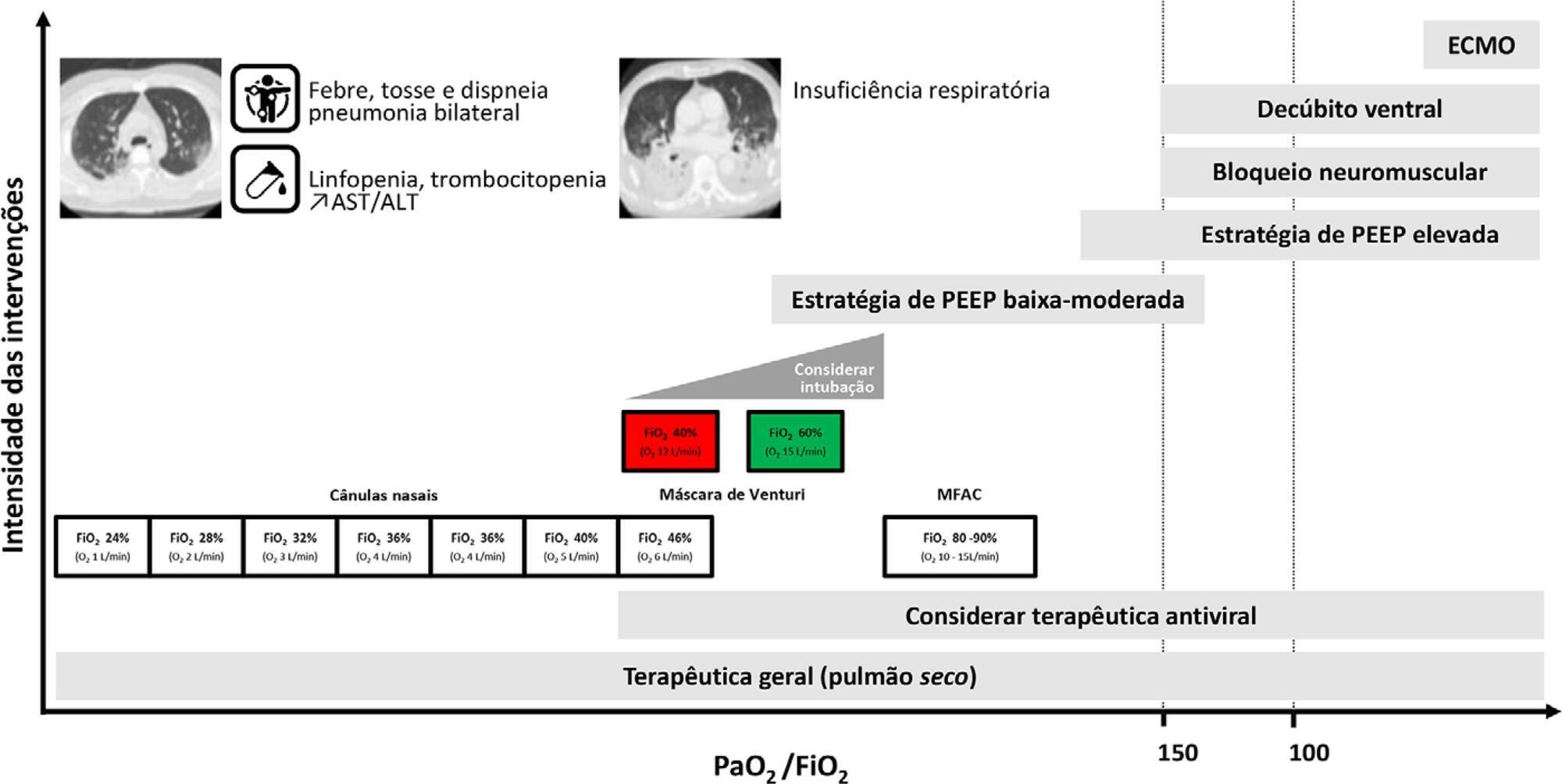
The Sociedade Portuguesa de Cuidados Intensivos and the Infection and Sepsis Group have previously issued health service and management recommendations for critically ill patients with COVID-19. Due to the evolution of knowledge, the panel of experts was again convened to review the current evidence and issue updated recommendations.
Methods:
A national panel of experts who declared that they had no conflicts of interest regarding the development of the recommendations was assembled. Operational questions were developed based on the PICO methodology, and a rapid systematic review was conducted by consulting different bibliographic sources. The panel determined the direction and strength of the recommendations using two Delphi rounds, conducted in accordance with the principles of the GRADE system. A strong recommendation received the wording “is recommended”, and a weak recommendation was written as “is suggested.”
Results:
A total of 48 recommendations and 30 suggestions were issued, covering the following topics: diagnosis of SARS-CoV-2 infection, coinfection and superinfection; criteria for admission, cure and suspension of isolation; organization of services; personal protective equipment; and respiratory support and other specific therapies (antivirals, immunomodulators and anticoagulation).
Conclusion:
These recommendations, specifically oriented to the Portuguese reality but that may also apply to Portuguese-speaking African countries and East Timor, aim to support health professionals in the management of critically ill patients with COVID-19. They will be continuously reviewed to reflect the progress of our understanding and the treatment of this pathology.
Keywords:Coronavirus infectionsCOVID-19/diagnosisCOVID-19/therapyPractice guidelines as topicSARS-CoV-2See more -
Special Article
Recommendations from the Sociedade Portuguesa de Cuidados Intensivos and Infection & Sepsis Group for intensive care approach to COVID-19
Rev Bras Ter Intensiva. 2020;32(1):2-10
Abstract
Special ArticleRecommendations from the Sociedade Portuguesa de Cuidados Intensivos and Infection & Sepsis Group for intensive care approach to COVID-19
Rev Bras Ter Intensiva. 2020;32(1):2-10
DOI 10.5935/0103-507X.20200002
Views0See moreABSTRACT
Current COVID-19 epidemics was declared on December 31, 2019 at the Wuhan city seafood market, rapidly spreading throughout China, and later reaching several countries (mainly South Korea, Japan, Italy and Iran) and, since March 1, reaching Portugal. Most of the infected patients present with mild symptoms, not requiring hospitalization. Among those admitted to the hospital, 6% to 10% require admission to the intensive care unit. These recommendations are aimed to support the organization of intensive care services to respond COVID-19, providing optimized care to the patient and protection for healthcare professionals.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis Septic shock




