You searched for:"José Manuel Pereira"
We found (2) results for your search.-
Original Article
Prognostic value of hyperlactatemia in infected patients admitted to intensive care units: a multicenter study
Rev Bras Ter Intensiva. 2022;34(1):154-162
Abstract
Original ArticlePrognostic value of hyperlactatemia in infected patients admitted to intensive care units: a multicenter study
Rev Bras Ter Intensiva. 2022;34(1):154-162
DOI 10.5935/0103-507X.20220010-en
Views1See moreABSTRACT
Objective:
To evaluate the influence of patient characteristics on hyperlactatemia in an infected population admitted to intensive care units and the influence of hyperlactatemia severity on hospital mortality.
Methods:
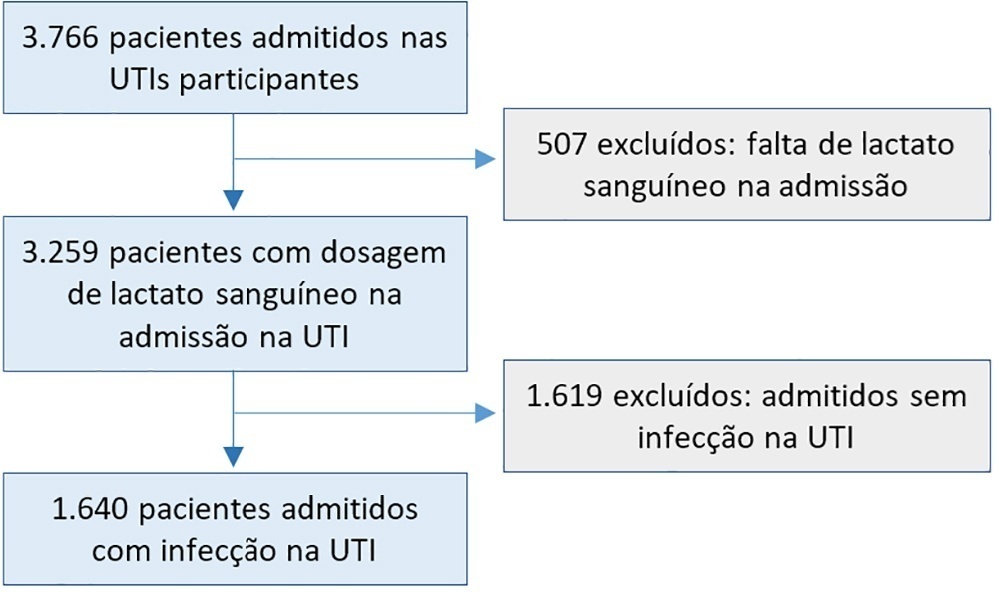
A post hoc analysis of hyperlactatemia in the INFAUCI study, a national prospective, observational, multicenter study, was conducted in 14 Portuguese intensive care units. Infected patients admitted to intensive care units with a lactate measurement in the first 12 hours of admission were selected. Sepsis was identified according to the Sepsis-2 definition accepted at the time of data collection. The severity of hyperlactatemia was classified as mild (2 – 3.9mmol/L), moderate (4.0 – 9.9mmol/L) or severe (> 10mmol/L).
Results:
In a total of 1,640 patients infected on admission, hyperlactatemia occurred in 934 patients (57%), classified as mild, moderate and severe in 57.0%, 34.4% and 8.7% of patients, respectively. The presence of hyperlactatemia and a higher degree of hyperlactatemia were both associated with a higher Simplified Acute Physiology Score II, a higher Charlson Comorbidity Index and the presence of septic shock. The lactate Receiver Operating Characteristic curve for hospital mortality had an area under the curve of 0.64 (95%CI 0.61 – 0.72), which increased to 0.71 (95%CI 0.68 – 0.74) when combined with Sequential Organ Failure Assessment score. In-hospital mortality with other covariates adjusted by Simplified Acute Physiology Score II was associated with moderate and severe hyperlactatemia, with odds ratio of 1.95 (95%CI 1.4 – 2.7; p < 0.001) and 4.54 (95%CI 2.4 - 8.5; p < 0.001), respectively.
Conclusion:
Blood lactate levels correlate independently with in-hospital mortality for moderate and severe degrees of hyperlactatemia.
-
Review Articles
Antibiotic therapy in ventilator-associated tracheobronchitis: a literature review
Rev Bras Ter Intensiva. 2018;30(1):80-85
Abstract
Review ArticlesAntibiotic therapy in ventilator-associated tracheobronchitis: a literature review
Rev Bras Ter Intensiva. 2018;30(1):80-85
DOI 10.5935/0103-507X.20180014
Views0ABSTRACT
The concept of ventilator-associated tracheobronchitis is controversial; its definition is not unanimously accepted and often overlaps with ventilator-associated pneumonia. Ventilator-associated tracheobronchitis has an incidence similar to that of ventilator-associated pneumonia, with a high prevalence of isolated multiresistant agents, resulting in an increase in the time of mechanical ventilation and hospitalization but without an impact on mortality. The performance of quantitative cultures may allow better diagnostic definition of tracheobronchitis associated with mechanical ventilation, possibly avoiding the overdiagnosis of this condition. One of the major difficulties in differentiating between ventilator-associated tracheobronchitis and ventilator-associated pneumonia is the exclusion of a pulmonary infiltrate by chest radiography; thoracic computed tomography, thoracic ultrasonography, or invasive specimen collection may also be required. The institution of systemic antibiotic therapy does not improve the clinical impact of ventilator-associated tracheobronchitis, particularly in reducing time of mechanical ventilation, hospitalization or mortality, despite the possible reduced progression to ventilator-associated pneumonia. However, there are doubts regarding the methodology used. Thus, considering the high prevalence of tracheobronchitis associated with mechanical ventilation, routine treatment of this condition would result in high antibiotic usage without clear benefits. However, we suggest the institution of antibiotic therapy in patients with tracheobronchitis associated with mechanical ventilation and septic shock and/or worsening of oxygenation, and other auxiliary diagnostic tests should be simultaneously performed to exclude ventilator-associated pneumonia. This review provides a better understanding of the differentiation between tracheobronchitis associated with mechanical ventilation and pneumonia associated with mechanical ventilation, which can significantly decrease the use of antibiotics in critically ventilated patients.
Keywords:Bronchitis/diagnosisBronchitis/drug therapyBronchitis/epidemiologyBronchitis/microbiologyPneumonia ventilator-associated/drug therapyTracheitis/diagnosisTracheitis/drug therapyTracheitis/epidemiologyTracheitis/microbiologySee more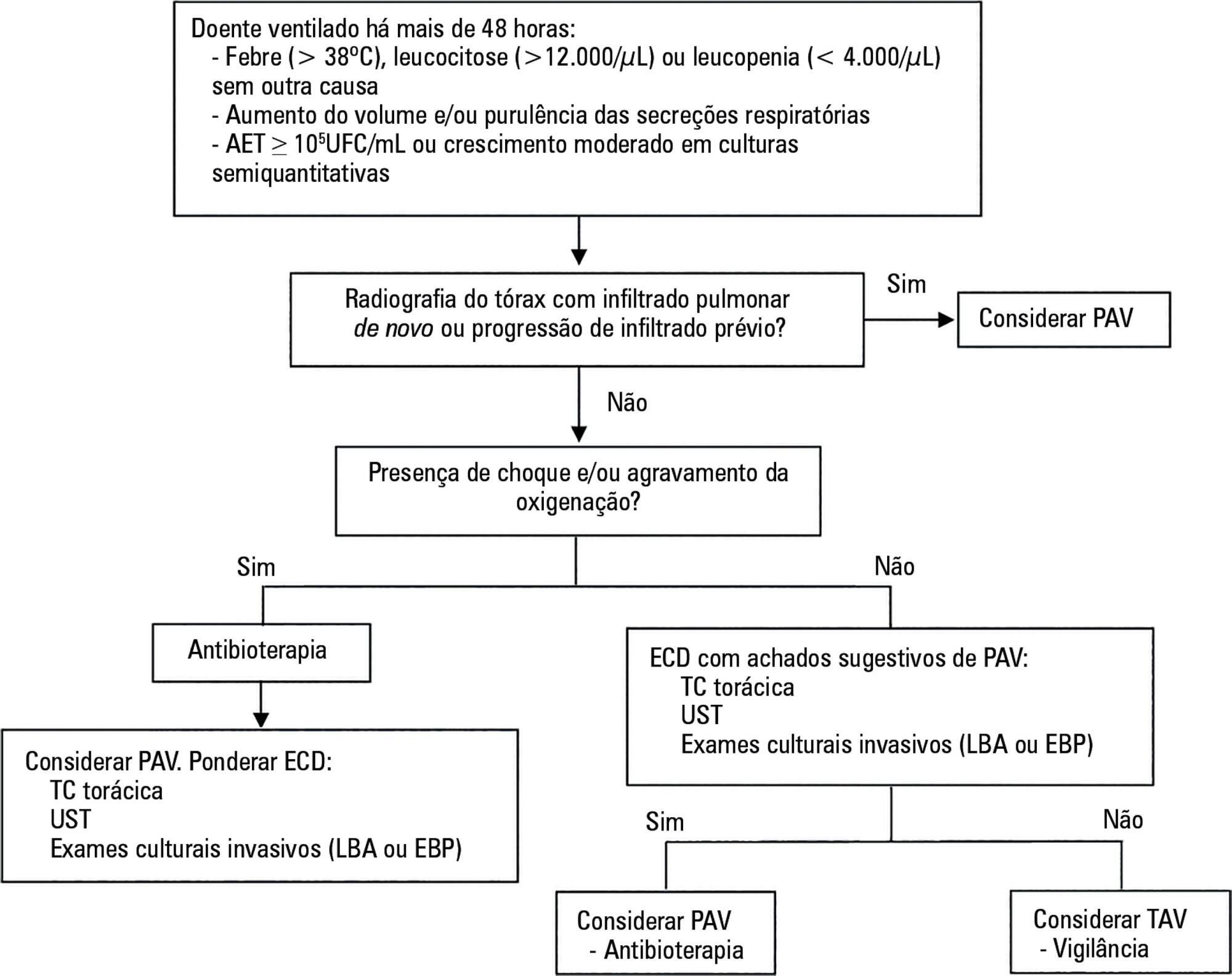
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




