Abstract
Rev Bras Ter Intensiva. 2018;30(1):80-85
DOI 10.5935/0103-507X.20180014
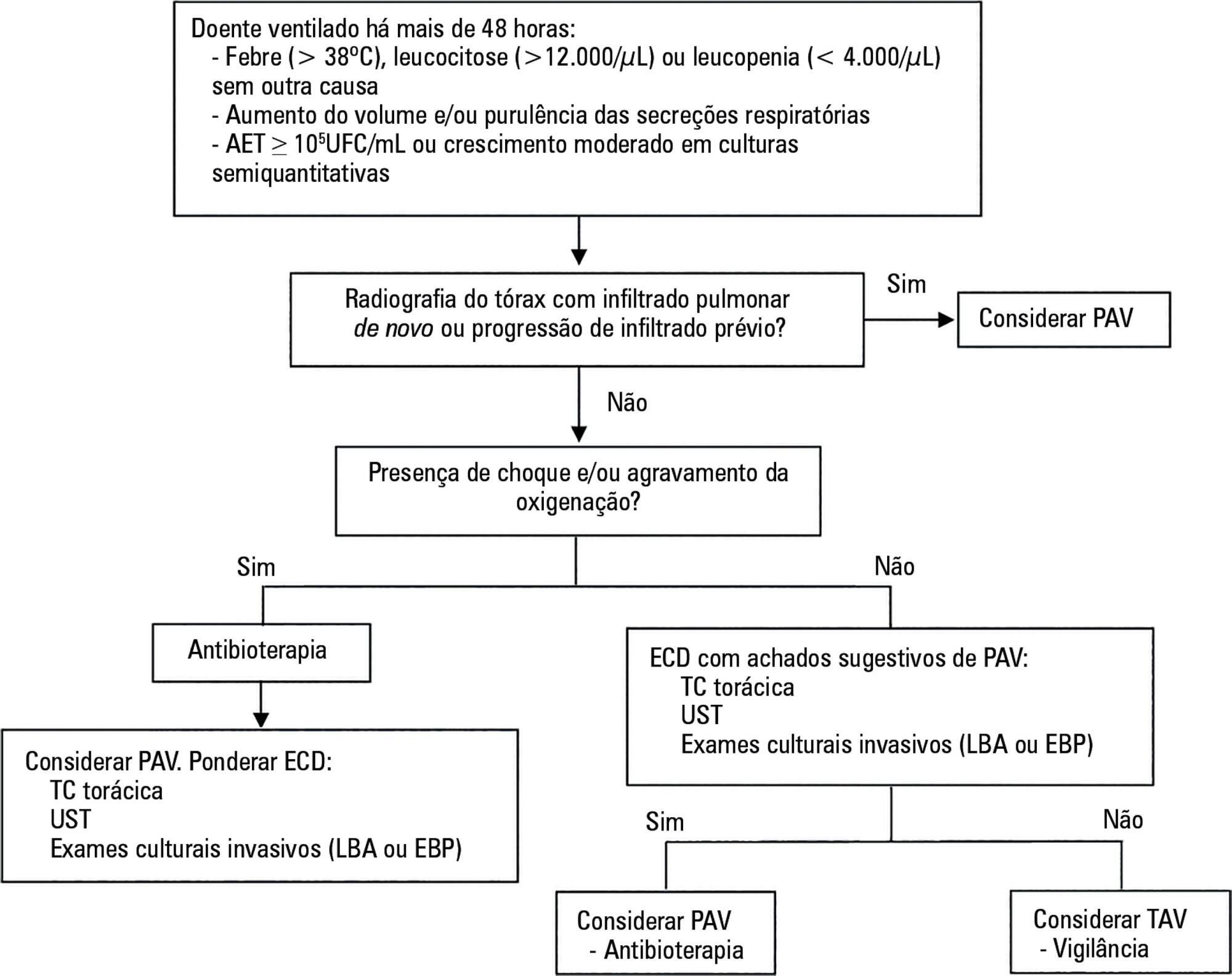
The concept of ventilator-associated tracheobronchitis is controversial; its definition is not unanimously accepted and often overlaps with ventilator-associated pneumonia. Ventilator-associated tracheobronchitis has an incidence similar to that of ventilator-associated pneumonia, with a high prevalence of isolated multiresistant agents, resulting in an increase in the time of mechanical ventilation and hospitalization but without an impact on mortality. The performance of quantitative cultures may allow better diagnostic definition of tracheobronchitis associated with mechanical ventilation, possibly avoiding the overdiagnosis of this condition. One of the major difficulties in differentiating between ventilator-associated tracheobronchitis and ventilator-associated pneumonia is the exclusion of a pulmonary infiltrate by chest radiography; thoracic computed tomography, thoracic ultrasonography, or invasive specimen collection may also be required. The institution of systemic antibiotic therapy does not improve the clinical impact of ventilator-associated tracheobronchitis, particularly in reducing time of mechanical ventilation, hospitalization or mortality, despite the possible reduced progression to ventilator-associated pneumonia. However, there are doubts regarding the methodology used. Thus, considering the high prevalence of tracheobronchitis associated with mechanical ventilation, routine treatment of this condition would result in high antibiotic usage without clear benefits. However, we suggest the institution of antibiotic therapy in patients with tracheobronchitis associated with mechanical ventilation and septic shock and/or worsening of oxygenation, and other auxiliary diagnostic tests should be simultaneously performed to exclude ventilator-associated pneumonia. This review provides a better understanding of the differentiation between tracheobronchitis associated with mechanical ventilation and pneumonia associated with mechanical ventilation, which can significantly decrease the use of antibiotics in critically ventilated patients.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):44-50
DOI 10.5935/0103-507X.20150008
To assess the adherence to Infectious Disease Society of America/American Thoracic Society guidelines and the causes of lack of adherence during empirical antibiotic prescription in severe pneumonia in Latin America.
A clinical questionnaire was submitted to 36 physicians from Latin America; they were asked to indicate the empirical treatment in two fictitious cases of severe respiratory infection: community-acquired pneumonia and nosocomial pneumonia.
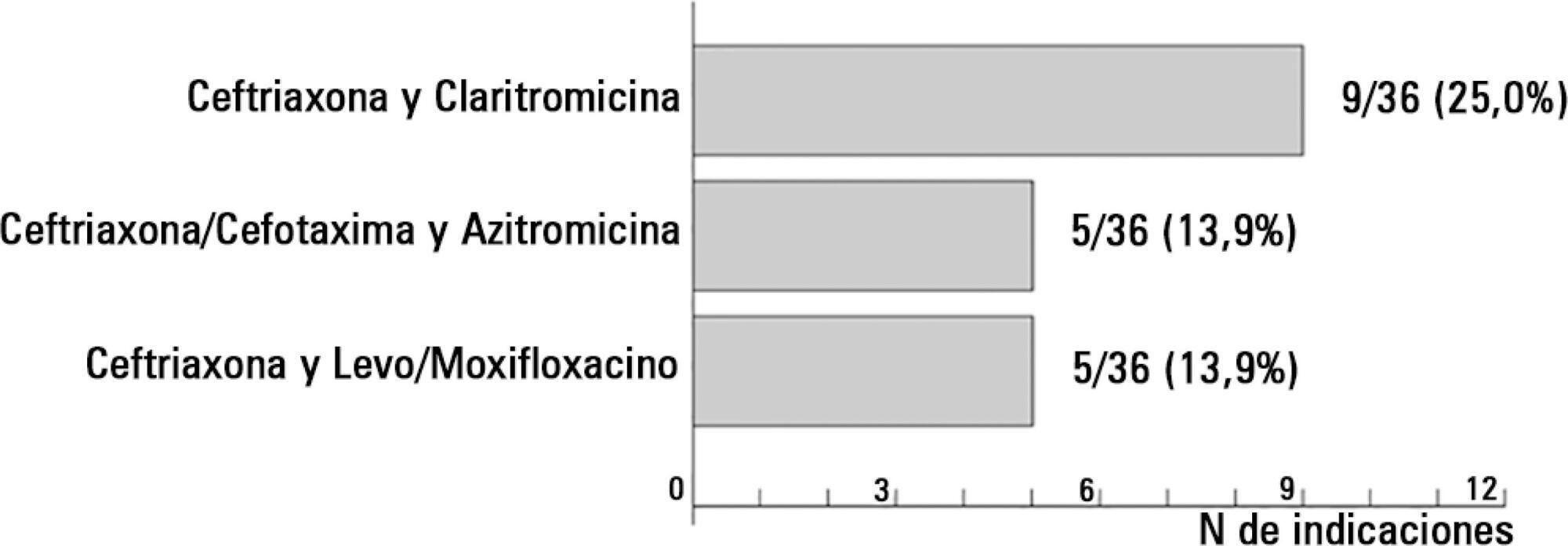
In the case of communityacquired pneumonia, 11 prescriptions of 36 (30.6%) were compliant with international guidelines. The causes for non-compliant treatment were monotherapy (16.0%), the unnecessary prescription of broad-spectrum antibiotics (40.0%) and the use of non-recommended antibiotics (44.0%).
The compliance rate with the Infectious Disease Society of America/American Thoracic Society guidelines in the community-acquired pneumonia scenario was 30.6%; the most frequent cause of lack of compliance was the indication of monotherapy. In the case of nosocomial pneumonia, the compliance rate with the guidelines was 2.8%, and the most important cause of non-adherence was lack of combined antipseudomonal therapy. If the use of monotherapy with an antipseudomonal antibiotic was considered the correct option, the treatment would be adequate in 100% of the prescriptions.