Abstract
Rev Bras Ter Intensiva. 2014;26(1):28-35
DOI 10.5935/0103-507X.20140005
To define the characteristics and measure the reaction time of a health care team monitoring alarms in the intensive care unit.
A quantitative, observational, and descriptive study developed at the coronary care unit of a cardiology public hospital in Rio de Janeiro state (RJ). Data were obtained from the information collected on the patients, the monitoring used, and the measurement of the team's reaction time to the alarms of multi-parameter monitors during a non-participatory field observation.
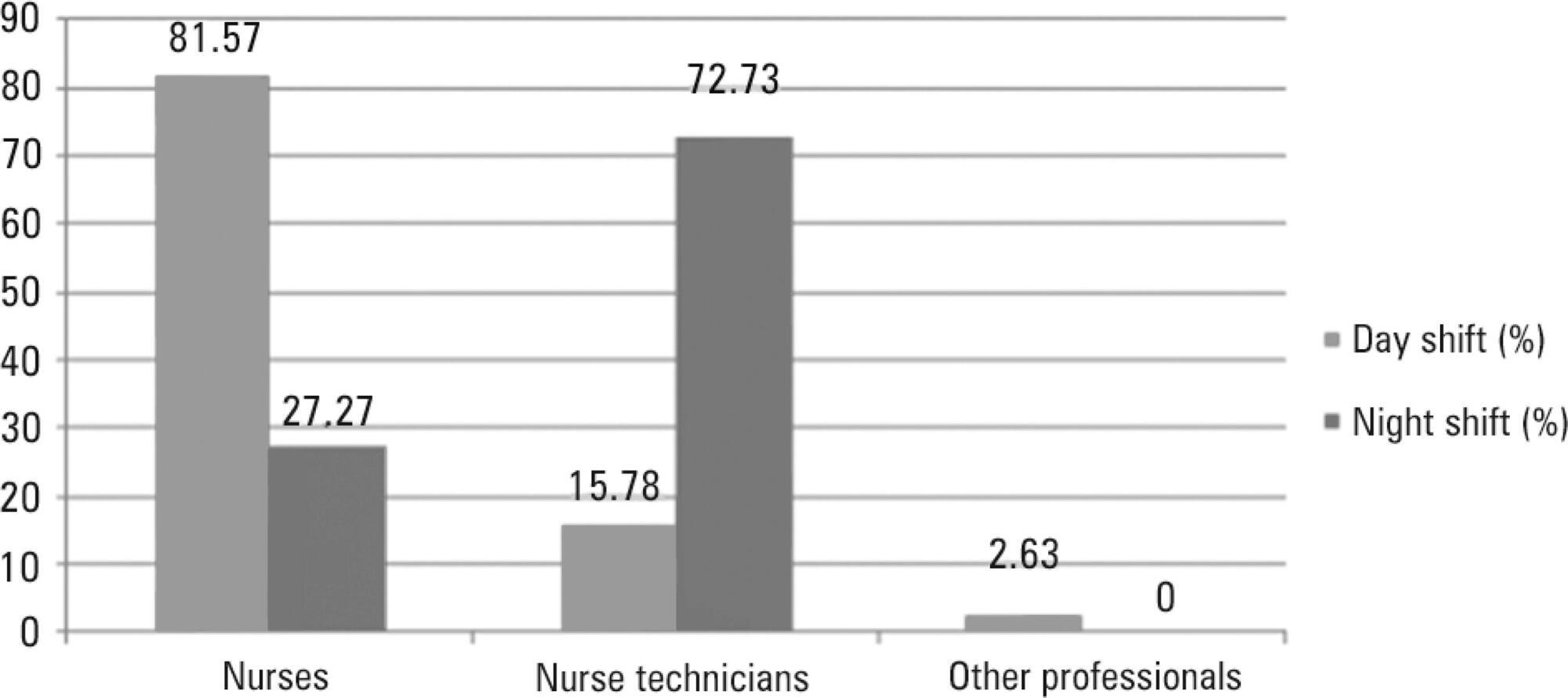
Eighty-eight patients were followed (49 during the day shift and 39 during the night shift). During the 40 hours of observation (20 hours during the day shift and 20 hours during the night shift), the total number of monitoring alarms was 227, with 106 alarms during the day shift and 121 during the night shift, an average of 5.7 alarms/hour. In total, 145 alarms unanswered by the team were observed, with 68 occurring during the day shift (64.15%) and 77 during the night shift (63.64%). This study demonstrated that the reaction time was longer than 10 minutes in more than 60% of the alarms, which were considered as unanswered alarms. The median reaction time of the answered alarms was 4 minutes and 54 seconds during the day shift and 4 minutes and 55 seconds during the night shift. The respiration monitoring was activated in only nine patients (23.07%) during the night shift. Regarding the alarm quality of these variables, the arrhythmia alarm was qualified in only 10 (20.40%) of the day-shift patients and the respiration alarm in four night-shift patients (44.44%).
The programming and configuration of the physiological variables monitored and the parameters of alarms in the intensive care unit were inadequate; there was a delay and lack of response to the alarms, suggesting that relevant alarms may have been ignored by the health care team, thus compromising the patient safety.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):99-105
DOI 10.5935/0103-507X.20130020
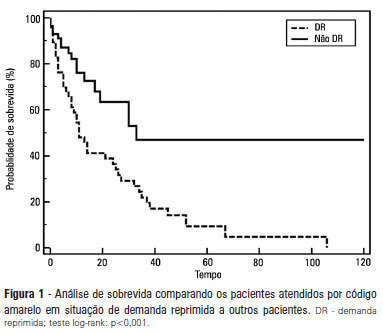
OBJECTIVE: To describe the epidemiological data of the clinical instability events in patients attended to by the rapid response team and to identify prognostic factors. METHODS: This was a longitudinal study, performed from January to July 2010, with an adult inpatient population in a hospital environment. The data collected regarding the code yellow service included the criteria of the clinical instability, the drug and non-drug therapies administered and the activities and procedures performed. The outcomes evaluated were the need for intensive care unit admission and the hospital mortality rates. A level of p=0.05 was considered to be significant. RESULTS: A total of 150 code yellow events that occurred in 104 patients were evaluated. The most common causes were related to acute respiratory insufficiency with hypoxia or a change in the respiratory rate and a concern of the team about the patient's clinical condition. It was necessary to request a transfer to the intensive care unit in 80 of the 150 cases (53.3%). It was necessary to perform 42 procedures. The most frequent procedures were orotracheal intubation and the insertion of a central venous catheter. The patients who were in critical condition and had to wait for an intensive care unit bed had a higher risk of death compared to the other patients (hazard ratio: 3.12; 95% CI: 1.80-5.40; p<0.001). CONCLUSIONS: There are patients in critical condition that require expert intensive care in the regular ward unit hospital beds. The events that most frequently led to the code yellow activation were related to hemodynamic and respiratory support. The interventions performed indicate the need for a physician on the team. The situation of pent-up demand is associated with a higher mortality rate.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):188-196
DOI 10.5935/0103-507X.20130034
Deep sedation in critically ill patients is associated with a longer duration of mechanical ventilation and a prolonged length of stay in the intensive care unit. Several protocols have been used to improve these outcomes. We implement and evaluate an analgesia-based, goal-directed, nurse-driven sedation protocol used to treat critically ill patients who receive mechanical ventilation.
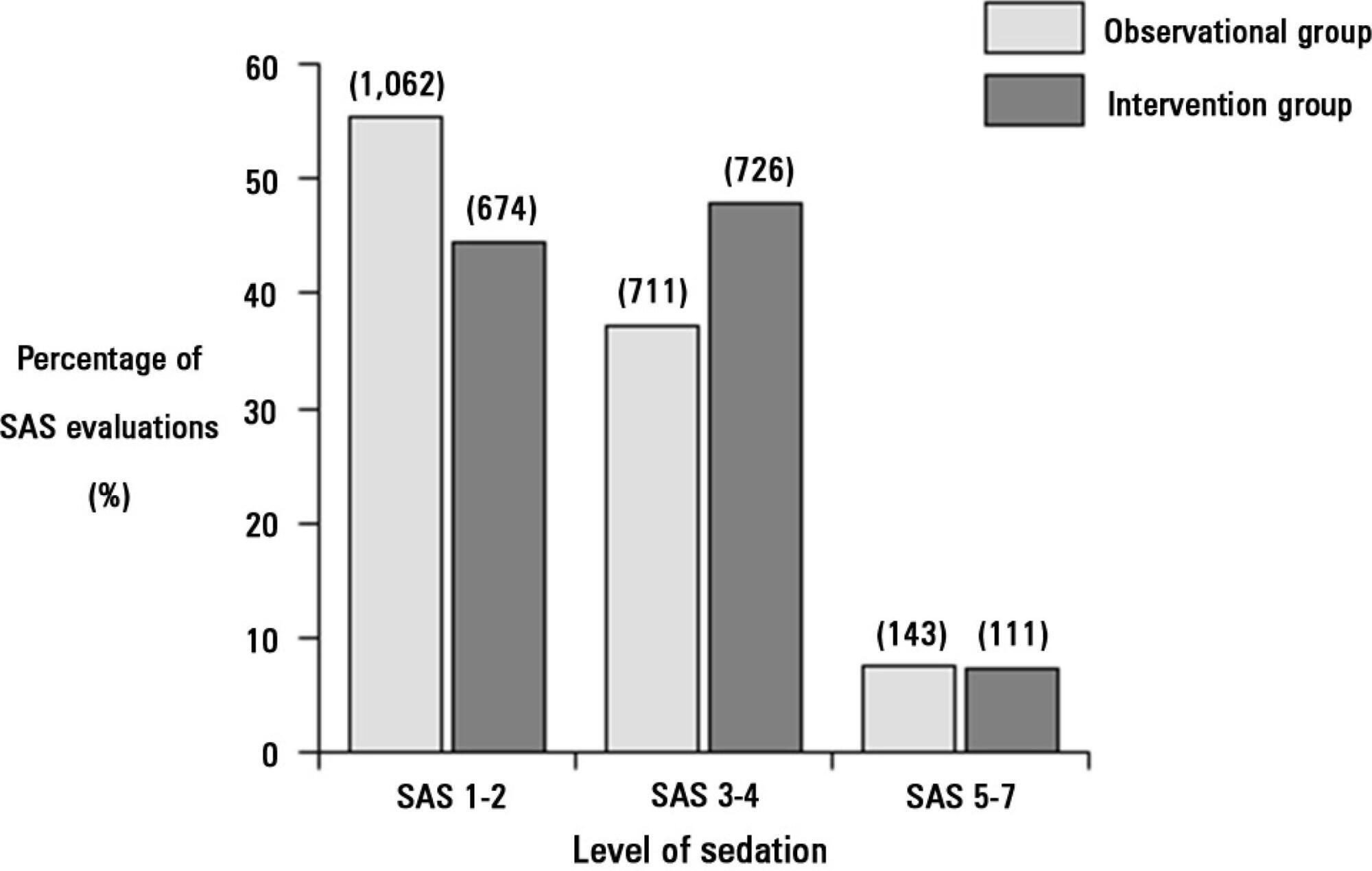
We performed a prospective, two-phase (before-after), non-randomized multicenter study that involved 13 intensive care units in Chile. After an observational phase (observational group, n=155), we designed, implemented and evaluated an analgesia-based, goal-directed, nurse-driven sedation protocol (intervention group, n=132) to treat patients who required mechanical ventilation for more than 48 hours. The primary outcome was to achieve ventilator-free days by day 28.
The proportion of patients in deep sedation or in a coma decreased from 55.2% to 44.0% in the interventional group. Agitation did not change between the periods and remained approximately 7%. Ventilator-free days to day 28, length of stay in the intensive care unit and mortality were similar in both groups. At one year, post-traumatic stress disorder symptoms in survivors were similar in both groups.
We designed and implemented an analgesia-based, goal-directed, nurse-driven sedation protocol in Chile. Although there was no improvement in major outcomes, we observed that the present protocol was safe and feasible and that it resulted in decreased periods of deep sedation without increasing agitation.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):257-263
DOI 10.1590/S0103-507X2010000300007
OBJECTIVE: To describe the frequency medication error disclosure to the team and to the family in an oncology pediatric patients' intensive care unit. METHODS: This was a descriptive and exploratory study performed between March 1 and May 31, 2008. A medication error report form was developed and implemented, to be completed by the professionals involved in the unit's medication process. RESULTS: The sample consisted of 71 forms collected over the 92 collection days. After medication error detection, the event was not reported to the pediatric intensive care unit's team in 34 (47.9%) cases. In the 37 reported to the team cases, for most of them (48.7%) the physician was the professional communicated. The event was not disclosed to the patient/family in 95.8% of medication error reports. CONCLUSIONS: Although the literature recommends disclosing the errors, this is not done in the studied pediatric intensive care unit.