Abstract
Rev Bras Ter Intensiva. 2017;29(2):163-170
DOI 10.5935/0103-507X.20170026
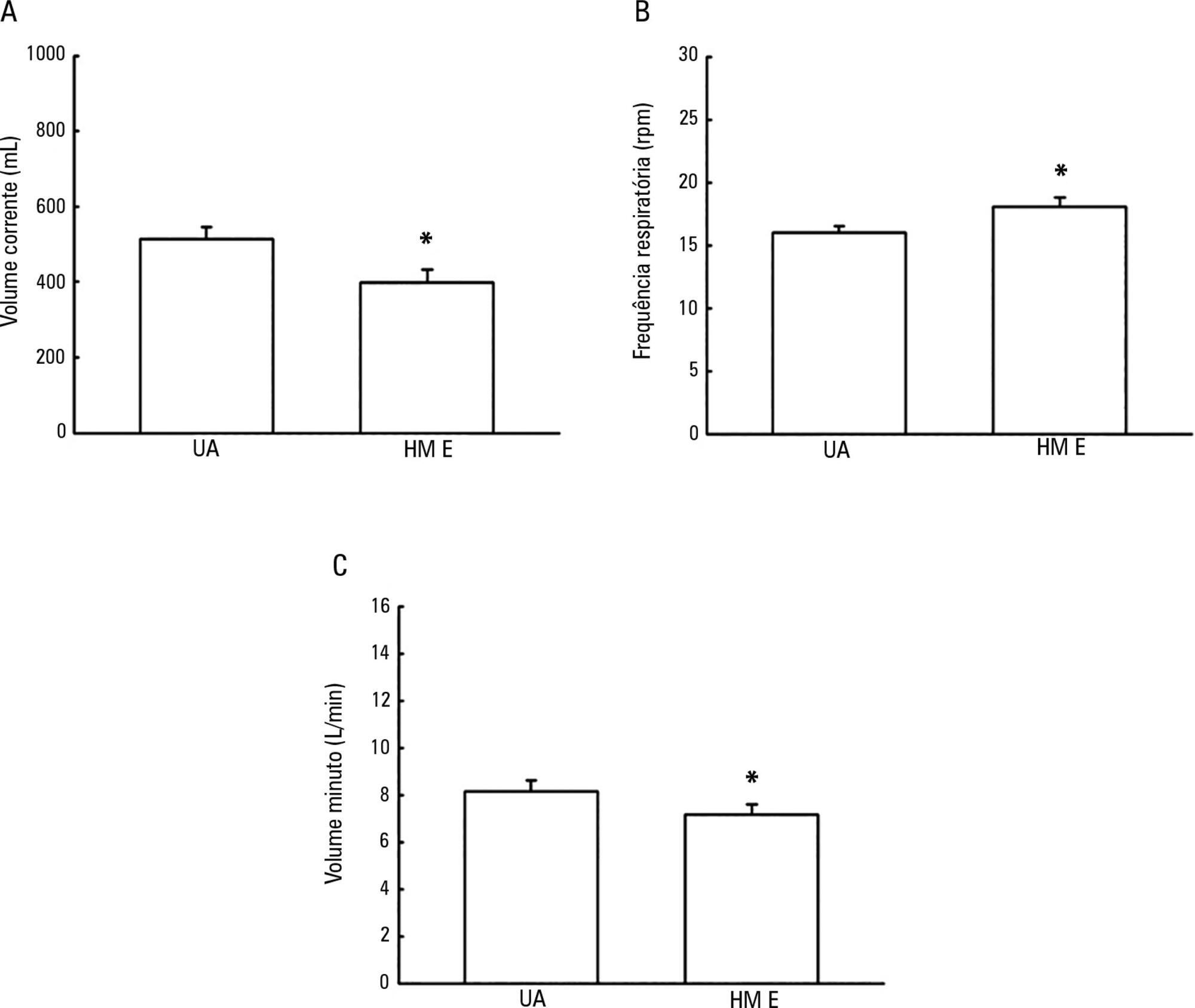
To evaluate the possible changes in tidal volume, minute volume and respiratory rate caused by the use of a heat and moisture exchanger in patients receiving pressure support mechanical ventilation and to quantify the variation in pressure support required to compensate for the effect caused by the heat and moisture exchanger.
Patients under invasive mechanical ventilation in pressure support mode were evaluated using heated humidifiers and heat and moisture exchangers. If the volume found using the heat and moisture exchangers was lower than that found with the heated humidifier, an increase in pressure support was initiated during the use of the heat and moisture exchanger until a pressure support value was obtained that enabled the patient to generate a value close to the initial tidal volume obtained with the heated humidifier. The analysis was performed by means of the paired t test, and incremental values were expressed as percentages of increase required.
A total of 26 patients were evaluated. The use of heat and moisture exchangers increased the respiratory rate and reduced the tidal and minute volumes compared with the use of the heated humidifier. Patients required a 38.13% increase in pressure support to maintain previous volumes when using the heat and moisture exchanger.
The heat and moisture exchanger changed the tidal and minute volumes and respiratory rate parameters. Pressure support was increased to compensate for these changes.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):213-221
DOI 10.5935/0103-507X.20170030
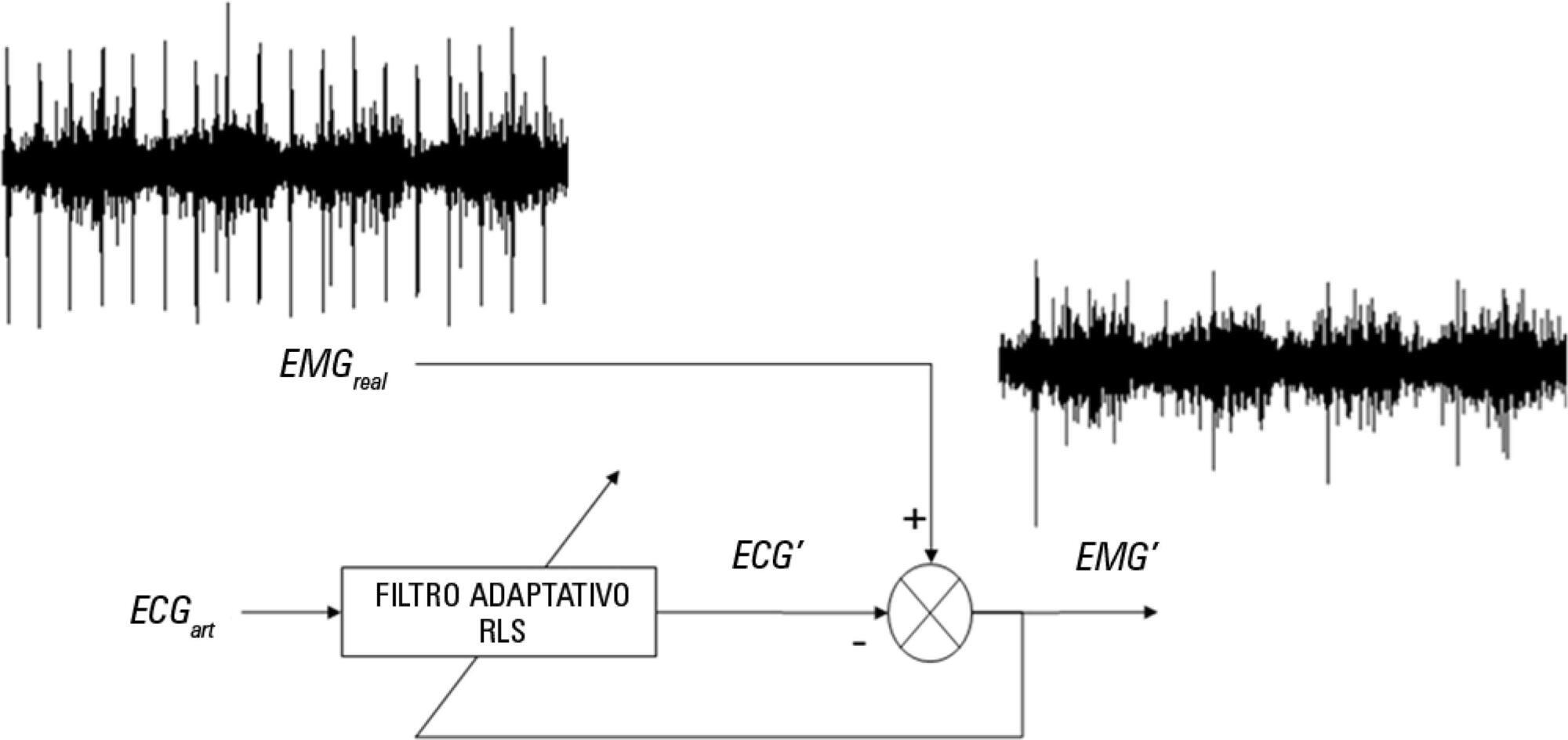
The aim of this pilot study was to evaluate the feasibility of surface electromyographic signal derived indexes for the prediction of weaning outcomes among mechanically ventilated subjects after cardiac surgery.
A sample of 10 postsurgical adult subjects who received cardiovascular surgery that did not meet the criteria for early extubation were included. Surface electromyographic signals from diaphragm and ventilatory variables were recorded during the weaning process, with the moment determined by the medical staff according to their expertise. Several indexes of respiratory muscle expenditure from surface electromyography using linear and non-linear processing techniques were evaluated. Two groups were compared: successfully and unsuccessfully weaned patients.
The obtained indexes allow estimation of the diaphragm activity of each subject, showing a correlation between high expenditure and weaning test failure.
Surface electromyography is becoming a promising procedure for assessing the state of mechanically ventilated patients, even in complex situations such as those that involve a patient after cardiovascular surgery.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):252-259
DOI 10.5935/0103-507X.20150046
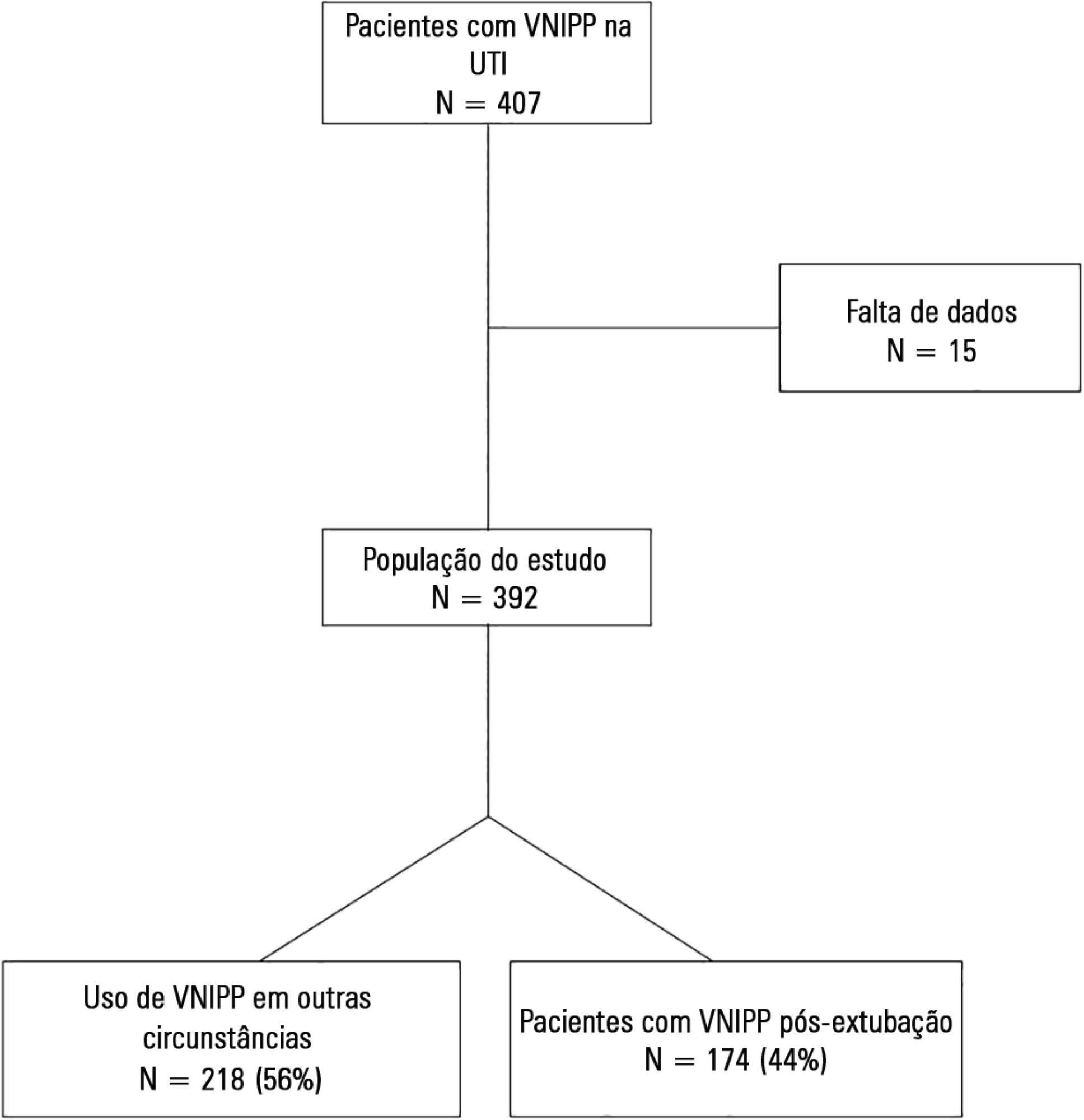
To describe postextubation noninvasive positive pressure ventilation use in intensive care unit clinical practice and to identify factors associated with noninvasive positive pressure ventilation failure.
This prospective cohort study included patients aged ≥ 18 years consecutively admitted to the intensive care unit who required noninvasive positive pressure ventilation within 48 hours of extubation. The primary outcome was noninvasive positive pressure ventilation failure.
We included 174 patients in the study. The overall noninvasive positive pressure ventilation use rate was 15%. Among the patients who used noninvasive positive pressure ventilation, 44% used it after extubation. The failure rate of noninvasive positive pressure ventilation was 34%. The overall mean ± SD age was 56 ± 18 years, and 55% of participants were male. Demographics; baseline pH, PaCO2 and HCO3; and type of equipment used were similar between groups. All of the noninvasive positive pressure ventilation final parameters were higher in the noninvasive positive pressure ventilation failure group [inspiratory positive airway pressure: 15.0 versus 13.7cmH2O (p = 0.015), expiratory positive airway pressure: 10.0 versus 8.9cmH2O (p = 0.027), and FiO2: 41 versus 33% (p = 0.014)]. The mean intensive care unit length of stay was longer (24 versus 13 days), p < 0.001, and the intensive care unit mortality rate was higher (55 versus 10%), p < 0.001 in the noninvasive positive pressure ventilation failure group. After fitting, the logistic regression model allowed us to state that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure compared with individuals with inspiratory positive airway pressure < 13.5 (OR = 3.02, 95%CI = 1.01 - 10.52, p value = 0.040).
The noninvasive positive pressure ventilation failure group had a longer intensive care unit length of stay and a higher mortality rate. Logistic regression analysis identified that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):119-124
DOI 10.5935/0103-507X.20150022
To evaluate the efficacy and safety of percutaneous tracheostomy by means of single-step dilation with fiber optic bronchoscopy assistance in critical care patients under mechanical ventilation.
Between the years 2004 and 2014, 512 patients with indication of tracheostomy according to clinical criteria, were prospectively and consecutively included in our study. One-third of them were high-risk patients. Demographic variables, APACHE II score, and days on mechanical ventilation prior to percutaneous tracheostomy were recorded. The efficacy of the procedure was evaluated according to an execution success rate and based on the necessity of switching to an open surgical technique. Safety was evaluated according to post-operative and operative complication rates.
The mean age of the group was 64 ± 18 years (203 women and 309 males). The mean APACHE II score was 21 ± 3. Patients remained an average of 11 ± 3 days on mechanical ventilation before percutaneous tracheostomy was performed. All procedures were successfully completed without the need to switch to an open surgical technique. Eighteen patients (3.5%) presented procedure complications. Five patients experienced transient desaturation, 4 presented low blood pressure related to sedation, and 9 presented minor bleeding, but none required a transfusion. No serious complications or deaths associated with the procedure were recorded. Eleven patients (2.1%) presented post-operative complications. Seven presented minor and transitory bleeding of the percutaneous tracheostomy stoma, 2 suffered displacement of the tracheostomy cannula, and 2 developed a superficial infection of the stoma.
Percutaneous tracheostomy using the single-step dilation technique with fiber optic bronchoscopy assistance seems to be effective and safe in critically ill patients under mechanical ventilation when performed by experienced intensive care specialists using a standardized procedure.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):167-172
DOI 10.1590/S0103-507X2012000200012
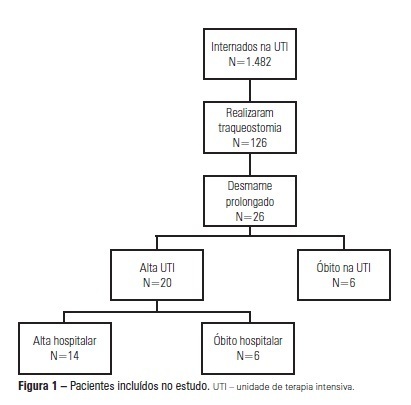
OBJECTIVE: We aimed to assess the use of noninvasive ventilation devices in patients with prolonged weaning following tracheotomy. METHODS: We performed a retrospective observational study using data collected from the clinical records of tracheotomized patients diagnosed with prolonged weaning. The participants were hospitalized in the adult intensive care unit of Moinhos de Vento Hospital, Porto Alegre (RS) between December 2007 and December 2008. RESULTS: In the data collection period, 1,482 patients were admitted to the intensive care unit. In total, 126 patients underwent tracheotomies, and 26 of these patients met the inclusion criteria for participating in the study. The average age of the patients in our sample was 73 ± 12 years. In our sample, 57.7% of the participants were female, and 80.8% were admitted as a result of acute hypoxemic respiratory failure. After the tracheotomy, the patients remained under mechanical ventilation for an average of 29.8 days. After the initiation of the experimental protocol, the tracheotomized patients remained under ventilation for an average of 53.5 days on a portable noninvasive device connected to the tracheotomy. There were three possible outcomes for the patients. They were discharged, were weaned from the noninvasive ventilation, or died in the intensive care unit or hospital ward. In total, 76.9% (20/26) of the patients were discharged from the intensive care unit, and 53.8% (14/26) of the patients were discharged from the hospital. CONCLUSION: The use of noninvasive portable ventilators connected to the tracheotomy may represent an alternative for discontinuing ventilationand discharging tracheotomized patients with prolonged ventilatory weaning from intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):199-206
DOI 10.1590/S0103-507X2011000200013
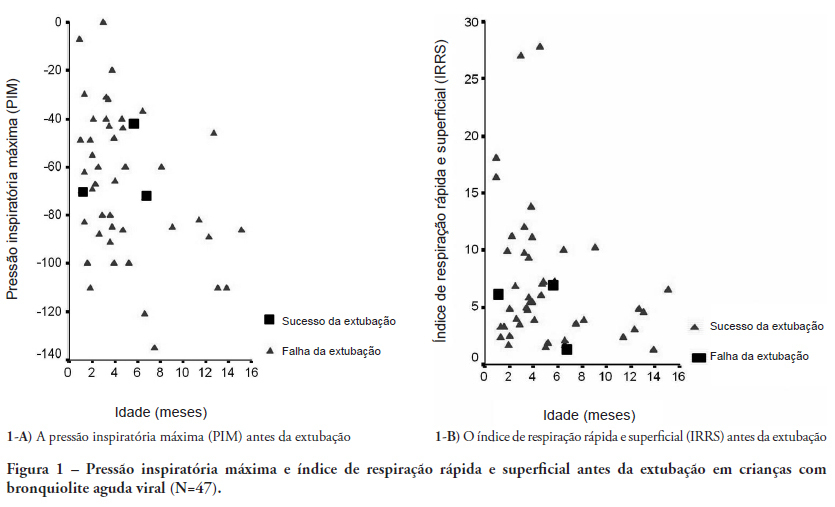
OBJECTIVES: Between 10% and 20% of children submitted to mechanical ventilation in the pediatric intensive care unit present extubation failure. Several ventilatory indexes have been proposed to predict extubation failure. The aim of this study was to analyze the accuracy of these indices in predicting successful extubation in children and to evaluate these variables according to the age of the patient and the specific disease. METHODS: A prospective observational study including all children submitted to mechanical ventilation in a Brazilian referral pediatric intensive care unit was conducted between August 2007 and August 2008. The tidal volume, maximal negative inspiratory pressure, rapid shallow breathing index and other ventilatory indexes were measured before extubation. These variables were analyzed according to the extubation outcome (success or failure) as well as age and specific disease (post cardiac surgery and acute viral bronchiolitis). RESULTS: A total of 100 patients were included (median age of 2.1 years old). Extubation failure was observed in 13% and was associated with lower weight (10.3+8.1 Kg vs. 5.5+2.4 Kg; p=0.01). We also evaluated the relationship between extubation failure and the main cause indicating mechanical ventilation: children who had received cardiac surgery (n=17) presented an extubation failure rate of 29.4% with a relative risk of 4.6 (1.2-17.2) when compared to children with acute viral bronchiolitis (n=47, extubation failure rate of 6.4%). The maximal inspiratory pressure was the only physiologic variable independently associated with the outcome. However, this variable showed a wide dispersion and lack of accuracy for predicting extubation success (sensitivity of 82% and specificity of 55% for a cut point of -37.5 cmH2O predicting successful extubation). The same wide dispersion was observed with other ventilatory indexes. CONCLUSION: The indexes for predicting extubation success in children submitted to mechanical ventilation are not accurate; they vary widely depending on age, main disease and other clinical aspects. New formulas including clinical variables should be developed for better prediction of extubation success in children submitted to mechanical ventilation
Abstract
Rev Bras Ter Intensiva. 2010;22(1):33-39
DOI 10.1590/S0103-507X2010000100007
OBJECTIVE: To verify if the maximal inspiratory pressure values with 40 seconds occlusion time are greater than with the 20 seconds occlusion time, and the impacts on the following patient's physiological variables: respiratory rate, pulse oxygen saturation, heart rate and blood pressure, before and after the measurements. METHODS: This was a transversal prospective randomized study. Fifty-one patients underwent maximal inspiratory pressure measurement, measured by one single investigator. The manometer was calibrated before each measurement, and then connected to the adapter and this to the unidirectional valve inspiratory branch for 20 or 40 seconds. RESULTS: The values with 40 seconds occlusion (57.6 ± 23.4 cmH2O) were significantly higher than the measurements taken with 20 seconds occlusion (40.5 ± 23.4 cmH2O; p=0.0001). The variables changes between the before and after measurement respiratory and hemodynamic parameters monitoring showed: heart rate variation for the 20 seconds occlusion 5.13 ± 8.56 beats per minute and after 40 seconds occlusion 7.94 ± 12.05 beats per minute (p = 0.053), versus baseline. The mean blood pressure change for 20 seconds occlusion was 9.29 ± 13.35 mmHg and for 40 seconds occlusion 15.52 ± 2.91 mmHg (p=0.021). The oxygen saturation change for 20 seconds occlusion was 1.66 ± 12.66%, and for 40 seconds 4.21 ± 5.53% (p=0.0001). The respiratory rate change for 20 seconds occlusion was 6.68 ± 12.66 movements per minute and for 40 seconds 6.94 ± 6.01 (p=0.883). CONCLUSION: The measurement of maximal inspiratory pressure using a longer occlusion (40 seconds) produced higher values, without triggering clinically significant stress according to the selected variables.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):47-52
DOI 10.1590/S0103-507X2010000100009
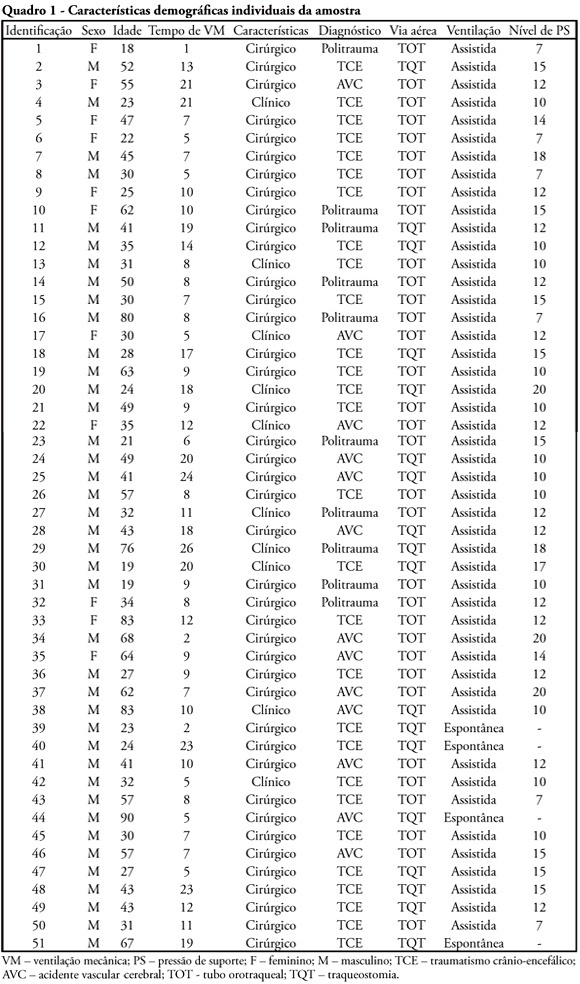
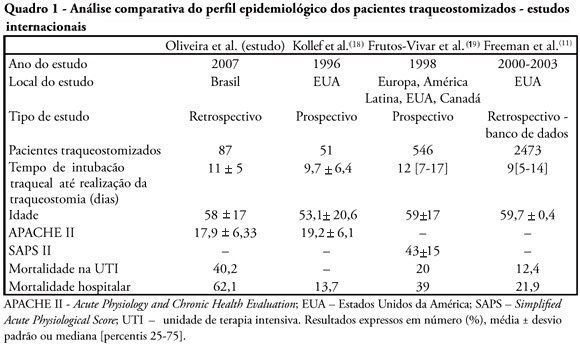
OBJECTIVES: Tracheostomy is a common procedure in intensive care unit to promote mechanical ventilation weaning. Despite tracheostomy is increasingly used there is no agreement of actual clinical practice of tracheostomy in different groups of patients in our environment. Objective of this study was to evaluate the epidemiological profile and outcomes of patients with tracheostomy at a clinical-surgical intensive care unit and compare this profile with the current literature. METHODS: Retrospective descriptive study through review of medical records and quality control database of "QuaTI" (Qualidade em Terapia Intensiva) of 87 patients with tracheostomy at Santa Casa de Belo Horizonte intensive care unit in 2007. We studied variables related to evolution aspects. RESULTS: The clinical and epidemiological analysis of the 87 patients showed: mean age 58 ± 17 years, mean Acute Physiology and Chronic Health Evaluation - APACHE II 18 ± 6, mean time of orotracheal intubation before tracheostomy of 11.17 ± 4.78 days. Intensive care unit mortality was 40.2% (35/87 patients), ward mortality was 36.5% (19/52) and overall hospital mortality 62.1% (54/87). Mean age of patients who died at intensive care unit (65 + 17 years) was greater than who were discharged to ward (53 ± 16 years) p = 0.003. Mean age of who died in hospital (intensive care unit and ward) (62 ± 17 years) was also higher than survivors (52 ± 16 years) p = 0.008. Old age (> 65 years) was related to intensive care unit mortality (OR 2.874, CI 1.165 a 7.088 p = 0.020) and also related to the overall hospital mortality (OR 3.202, CI 1.188 a 8.628 p = 0.019). There were not others variables related to mortality in this sample. CONCLUSIONS: The epidemiological profile of patients who underwent tracheotomy in the intensive care unit showed high mortality rate when compared to international series. Senility was related to worse outcome in these patients. Other issues were not related mortality in this group.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)