Abstract
Rev Bras Ter Intensiva. 2011;23(2):199-206
DOI 10.1590/S0103-507X2011000200013
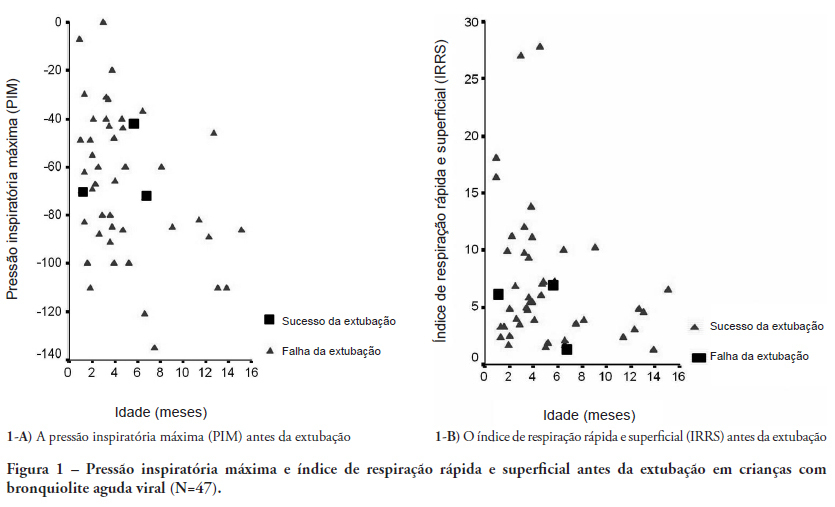
OBJECTIVES: Between 10% and 20% of children submitted to mechanical ventilation in the pediatric intensive care unit present extubation failure. Several ventilatory indexes have been proposed to predict extubation failure. The aim of this study was to analyze the accuracy of these indices in predicting successful extubation in children and to evaluate these variables according to the age of the patient and the specific disease. METHODS: A prospective observational study including all children submitted to mechanical ventilation in a Brazilian referral pediatric intensive care unit was conducted between August 2007 and August 2008. The tidal volume, maximal negative inspiratory pressure, rapid shallow breathing index and other ventilatory indexes were measured before extubation. These variables were analyzed according to the extubation outcome (success or failure) as well as age and specific disease (post cardiac surgery and acute viral bronchiolitis). RESULTS: A total of 100 patients were included (median age of 2.1 years old). Extubation failure was observed in 13% and was associated with lower weight (10.3+8.1 Kg vs. 5.5+2.4 Kg; p=0.01). We also evaluated the relationship between extubation failure and the main cause indicating mechanical ventilation: children who had received cardiac surgery (n=17) presented an extubation failure rate of 29.4% with a relative risk of 4.6 (1.2-17.2) when compared to children with acute viral bronchiolitis (n=47, extubation failure rate of 6.4%). The maximal inspiratory pressure was the only physiologic variable independently associated with the outcome. However, this variable showed a wide dispersion and lack of accuracy for predicting extubation success (sensitivity of 82% and specificity of 55% for a cut point of -37.5 cmH2O predicting successful extubation). The same wide dispersion was observed with other ventilatory indexes. CONCLUSION: The indexes for predicting extubation success in children submitted to mechanical ventilation are not accurate; they vary widely depending on age, main disease and other clinical aspects. New formulas including clinical variables should be developed for better prediction of extubation success in children submitted to mechanical ventilation
Abstract
Rev Bras Ter Intensiva. 2007;19(3):359-363
DOI 10.1590/S0103-507X2007000300017
BACKGROUND AND OBJECTIVES: To analyze and discuss the medical practices related to the end-of-life care provided to children admitted to pediatric intensive care unit (PICU) in Brazil and in some countries located in the northern hemisphere. CONTENTS: Selected articles on end-of-life care published during the last years searching the PubMed, MedLine and LILACS database, with special interest on studies of death conducted in pediatric intensive care units in Brazil, Latin America, Europe and North America, using the following key words: death, bioethics, PICU, cardiopulmonary resuscitation and life support limitation (LSL). CONCLUSIONS: In North America and North Europe, the incidence of LSL is greater (60%-80%) than in south Europe and Latin America (30%-40%). In Brazil the incidence of LSL depends on the region and in the last decade it is increasing from 6% to 40%; being the do-not-reanimated order the most frequent mode of LSL. The family participation in the decision making process is not stimulated and incipient. Based on the literature review and on their experience the authors present the measures that they consider most efficient and recommended for managing this situation in our region. Despite of LSL in children with terminal and irreversible disease be considered ethically, morally and legally; these measures are still adopted in a very few circumstances in our region. Urgent changes in this behavior are necessary, specially related to family participation in the decision-making process.