Abstract
Rev Bras Ter Intensiva. 2008;20(2):115-123
DOI 10.1590/S0103-507X2008000200001
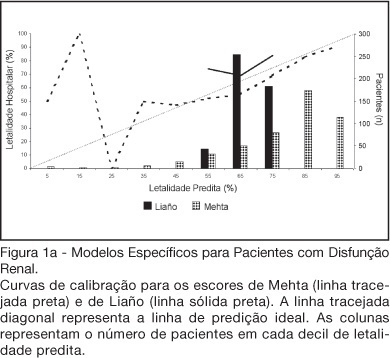
BACKGROUND AND OBJECTIVES: There is no consensus about prognostic scores for use in patients with acute kidney injury (AKI). The aim of this study was to evaluate the performance of six prognostic scores in predicting hospital mortality in patients with AKI and need for renal replacement therapy (RRT). METHODS: Prospective cohort of patients admitted to the intensive care units (ICU) of three tertiary care hospitals that required RRT for AKI over a 32-month period. Patients with end-stage renal disease and those with ICU stay < 24h were excluded. Data from the first 24h of ICU admission were used to calculate SAPS II and APACHE II scores, and data from the first 24h of RRT were used in the calculation of LOD, ODIN, Liaño and Mehta scores. Discrimination was evaluated using the area under ROC curve (AUROC) and calibration using the Hosmer-Lemeshow goodness-of-fit test. The hospital mortality was the end-point of interest. RESULTS: 467 patients were evaluated. Hospital mortality rate was 75%. Mean SAPS II and APACHE II scores were 48.5 ±11.2 and 27.4 ± 6.3 points, and median LOD score was 7 (5-8) points. Except for Mehta score (p = 0.001), calibration was appropriate in all models. However, discrimination was uniformly unsatisfactory; AUROC ranged from 0.60 for ODIN to 0.72 for SAPS II and Mehta scores. In addition, except for Mehta, all models tended to underestimate hospital mortality. CONCLUSIONS: Organ dysfunction, general and renal-specific severity-of-illness scores were inaccurate in predicting outcome in ICU patients in need for RRT.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):124-127
DOI 10.1590/S0103-507X2008000200002
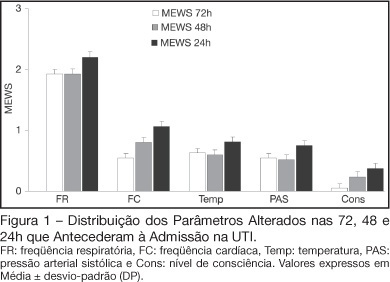
BACKGROUND AND OBJECTIVES: Prognosis of patients in the intensive care unit (ICU) has a relation with their severity just before admission. The Modified Early Warning Score (MEWS) was used to evaluate the severe condition of patients 12, 24 and 72 hours before admission in the ICU, assess the most prevalent parameters and correlate the MEWS before ICU with the outcome (survival versus death). METHODS: Retrospective analyses of 65 patients consecutively admitted to the ICU from July to October, 2006 evaluating the physiological parameters 72 hours prior to admission. RESULTS: APACHE II mean was 22.2 ± 7.9 points, mortality was 54.6% and standardized mortality ratio means was 1.24. MEWS means were 3.7 ± 0.2; 4.0 ± 0.2 and 5.1 ± 0.2 points, calculated 72, 48 and 24 hours previous to ICU admission, respectively. An increasing percentage of patients with MEWS > 3 points within 72, 48 and 24 hours before admission - 43.8%, 59.4% and 73.4%, respectively was recorded. Among the included physiological parameters respiratory rate contributed the most to the MEWS. Highest mortality was found in patients with MEWS > 3 points already found 72 hours before admission. Patients who died presented with a significant increase in the MEWS 24 hours prior to admission to the ICU (in relation to the MEWS recorded 72 hours before) but the situation was not identified in survivors. CONCLUSIONS: MEWS closely identified the severity of patients admitted to the ICU, suggesting that it can be a reliable score, useful in the situations preceding the ICU.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):128-134
DOI 10.1590/S0103-507X2008000200003
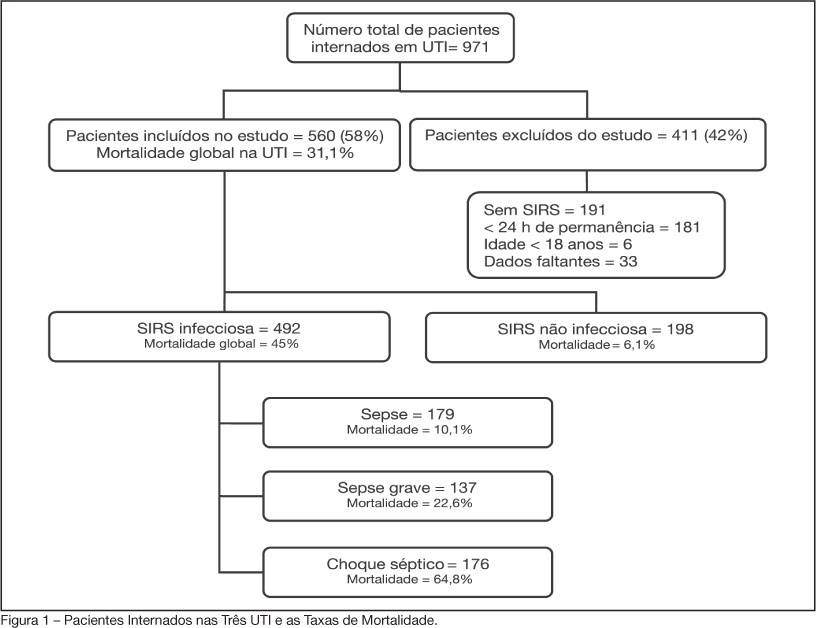
BACKGROUND AND OBJECTIVES: Sepsis is the main cause of death in patients treated in intensive care units (ICU). The aim of this study was to evaluate etiology, prognostic factors and mortality of septic patients treated in ICU of Passo Fundo, Brazil. METHODS: Out of 971 consecutive patients prospectively evaluated from August 2005 to February 2006, 560 were selected due to presence of systemic inflammatory response syndrome (SIRS) and followed for 28 days or until discharge or death. Patients were categorized according with the etiology of SIRS and further classified as having SIRS, sepsis, severe sepsis and septic shock. Prognosis was assessed by means of Apache II and SOFA. Mortality was compared in different etiologies of sepsis, APACHE II and SOFA scores, parameters. RESULTS: Of the 971 patients admitted to the ICU, 560 developed SIRS (58%). The most frequent cause of internation was neurological disease (28.9%), the most frequent site of infection was the respiratory tract (71.6%), and the most prevalent pathogens were gram-negative bacilli (53.2%). Mean APACHE II score was 18 ± 9, and mean SOFA score was 5 ± 4. Median ICU stay was 6 (3-11) days and overall mortality rate was 31.1%: 6.1% for non-infectious SIRS, 10.1% for sepsis, 22.6% for severe sepsis, and 64.8% for septic shock. CONCLUSIONS: Sepsis is an important health problem that leads to an extremely high mortality rate in the ICU of Passo Fundo, Brazil.
Abstract
Rev Bras Ter Intensiva. 2008;20(2):135-143
DOI 10.1590/S0103-507X2008000200004
BACKGROUND AND OBJECTIVES: To face the high mortality of sepsis, interventions grouped as "Surviving Sepsis Campaign" have been suggested. The aim of the study was to describe the application of glycemic control, corticoid use in septic shock, inotropics and drotrecogin-alpha in sepsis. METHODS: We studied 110 patients with sepsis from Recife/Brazil, who received drotrecogin-alpha between 2003/2006. Data on management of sepsis considering Surviving Sepsis Campaign, drotrecogin-alpha, mortality at 28 days and severe bleeding were recorded. RESULTS: Mean APACHE II was 25.6 and mean SOFA was 9.2. Around 95% of the patients presented two or more organ dysfunctions and 98% presented septic shock. The majority (56%) were under 65 years. Abdominal (48%) and respiratory (28%) focus of infection were the most prevalent. Hydrocortisone was used in 61% of the patients, and 29 (48.3%) died. Of the 38 patients with prolonged shock that did not receive it, 28 (73.7%) died. Of the 97 patients who presented uncontrolled glycemia only 65% achieved strict glycemic control and the mortality was 51.6%. Fluid gain ranged from 600 ml to 9,400 ml in the first 24h. In only 30 patients was myocardial dysfunction detected. The infusion of drotrecogin alpha started within 24h in 45%, between 24 and 48h in 35% and after 48h in 20%. Death occurred in 57% and severe bleeding in 9%. CONCLUSIONS: Discrepancy between the recommendations of Surviving Sepsis Campaign and clinical practice was observed. Death rate was 57%, similar to that found in the literature for septic shock irrespective of the use of drotrecogin-alpha.