Abstract
Rev Bras Ter Intensiva. 2008;20(1):57-62
DOI 10.1590/S0103-507X2008000100009
BACKGROUND AND OBJECTIVES: It is important to know the risk factors for extubation failure (EF) in children submitted to cardiac surgery in order to avoid inherent events due to reintubation (airways injury, usage of medications, cardiovascular changes) and because of prolonged ventilatory support (pneumonias, reduction of the ventilatory muscles strength). The objective of this study is to evaluate mechanical ventilation (MV) parameters, ventilatory mechanics [rapid shallow breathing index (RSBI), ventilatory muscles force [the maximum inspiratory pressure (MIP), the maximum expiratory pressure (MEP) and the load/force balance (LFB)] and blood gases before and after extubation in pediatric patients undergoing cardiac surgery. METHODS: Prospective (March 2004 to March 2006) observational cross sectional study, enrolling children submitted to cardiac surgery admitted to an university PICU hospital and considered able to be extubated. With the tracheal tube in situ and maintaining the children spontaneously breathing we evaluate: expiratory minute volume (V E), MIP and MEP. We calculated the RSBI [(RR/VT)/Weight)], LFB [15x [(3xMAP)/MIP] + 0.03 x RSBI-5], the mean airway pressure (MAP) [MAP={(PIP-PEEP)x[Ti/(Te+Ti)]}+PEEP] and the oxygenation index (OI) [OI=(FiO2 x MAP/PaO2)x100]. Arterial blood gas was collected one hour before extubation. If after 48 hours there was no need to reintubate the patient the extubation was considered successful (SE). RESULTS: 59 children were included. EF was observed in 19% (11/59). Median (QI25%-75%) for age, weight, MAP, OI, duration of MV after cardiac surgery (DMV) were respectively, 36 (12-82) months, 12 (8-20) kg, 8 (6-9), 2 (2-5), 1 (1-3) days. Median (QI25-75%) of EF in relation to SE for OI, LFB and DMV were respectively 5(3-8) versus 2(2-4), p = 0.005; [8(6-11) versus 5(4-6), p =0.002 and 3(2-5) versus 1(1-2) days, p = 0.026. Mean ± SD of EF in relation to SE for V E, PaO2 and MIP were respectively 1.7 ± 0.82 versus 3 ± 2.7 mL/kg/min, p = 0.003); 64 ± 34 versus 111 ± 50 mmHg, p = 0.002 and 53 ± 18 versus 78 ± 28 cmH2O; p=0.002. Concerning the risk factors for EF: OI > 2 (area under the ROC 0.74, p = 0.017) and LFB > 4 (area under the ROC 0.80, p = 0.002), achieved a sensibility of 100% and specificity of 80%; MIP < -35 cmH2O (area under the ROC 0.23; p= 0.004) achieved a sensibility of 80% and specificity of 60%. CONCLUSIONS: EF in children submitted to cardiac surgery is related to OI > 2, LFB > 4, DMV > 3 days; V E < 1.7 mL/kg/min, PaO2 < 64 mmHg and MIP < - 53 cmH2O. The kind of cardiac defect, MAP, RSBI and arterial blood gas were not related to EF.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):24-30
DOI 10.1590/S0103-507X2008000100004
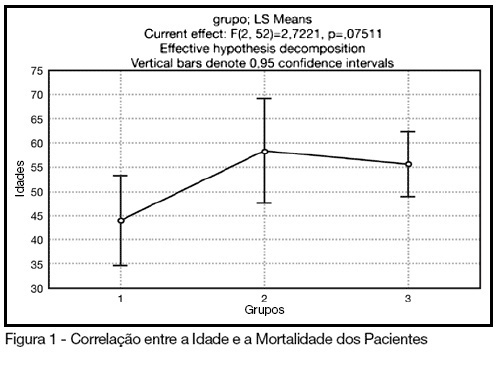
BACKGROUND AND OBJECTIVES: The control of patient discomfort in the intensive care unit (ICU) has become an integral part of critical care practice. The sedoanalgesic drugs could influence critically ill patient's morbimortality. Alpha²-adrenoceptor agonists might have an interesting future in ICU. The objective of this study is to evaluate the clonidine use for sedoanalgesia in ICU patients under prolonged mechanical ventilation. METHODS: Historical cohort study. Admitted patient files, January-December 2006, which stayed under mechanical ventilation, analgesia and sedation > 7days were analyzed. Demographic, clinical features and therapeutic data concerning analgesia and sedation were remarked. The data allowed classify the patients in three different groups: G1 = patients that used clonidine and other drugs; G2 = patients that used three or more drugs, without clonidine and G3 = patients that used fentanyl and midazolam. The mean daily doses of infused clonidine were registered, and the values of heat rate (HR), blood arterial pressure (BAP) before starting use of clonidine, after six hours and 24 hours were also registered. Statistical analyzes were performed using Variance Analysis (ANOVA), t tests and x² (significance p < 0.05). RESULTS: Were selected 55 patients. Fifteen (27.2%) belonged to G1, 11 (20%) belonged to G2 and 29 (52.7%) belonged to G3. The mean age of patients was 44 (G1), 50 (G2) and 56 (G3) (p = NS). The mean score APACHE II was 18 (G1), 20.4 (G2) and 20.7 (G3) (p = NS). G1 and G2 patients presented higher ICU length-of-stay (p < 0.05). The mean dose of clonidine used was 1.21 ± 0.54 mg/kg/min. G1 patients had HR and BAP decreased, however these effects were not considered clinically relevant. The mortality was lower in the patients from G1 (20%) when compared to G2 (54.5%) and G3 (62%) (p < 0.05). CONCLUSIONS: The clonidine use to analyzed patients did not result in clinical relevant side effects. The lower mortality index in patients that used clonidine was statistical significant.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):82-87
DOI 10.1590/S0103-507X2008000100013
BACKGROUND AND OBJECTIVES: Until the end of the previous century it remained controversial to admit cancer patients to the ICU for advanced-life-supporting therapy. However, over the past few years several centres over the world have shown that it is possible to achieve a meaningful survival in these patients. The aim of this review is to focus on the improvement in outcome that has been achieved over the past two decades in critically ill cancer patients. CONTENTS: We performed a MEDLINE search (period of 1980 to November 2007) to identify full-text English language publications on critically ill patients with solid tumors or hematological malignancies with particular interest for the outcome and treatment. Major MESH search terms included; cancer, solid tumor, hematologic or hematological malignancies, immunosupression, ICU, ventilation, organ failure, sepsis and infection. Additional studies were identified through a manual search of citations from retrieved articles. CONCLUSIONS: In this review, we first focus on the grim prognosis in the past, subsequently we discuss the improvements in outcome over the past few years across subgroups of cancer patients with increasing degree of severity of illness, and finally, we focus on the value of non-invasive ventilation since it is considered the initial ventilatory strategy in these patients.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):407-411
DOI 10.1590/S0103-507X2006000400015
BACKGROUND AND OBJECTIVE: The objective of this study was to review the literature on inhaled nitric oxide to children with acute respiratory distress syndrome. CONTENTS: A review of literature and selection of the most important publications on inhaled nitric oxide, using the MedLine and Cochrane Systematic Review Databases. This review was organized as follows: introduction; metabolism and biological effects; clinical applications; dosage, gas administration and weaning process; warnings and side-effects. Inhaled nitric oxide use was described in acute respiratory distress syndrome. CONCLUSIONS: Inhaled nitric oxide as the first vasodilator to produce selective pulmonary vasodilation has beneficial effects on gas exchange and ventilation, improving outcome in children with severe hypoxia. It is safe when administered in intensive care units under strict surveillance and monitoring. Further studies should be concentrated on early treatment, when acute respiratory distress syndrome is potentially reversible.
Abstract
Rev Bras Ter Intensiva. 2006;18(4):351-359
DOI 10.1590/S0103-507X2006000400006
BACKGROUND AND OBJECTIVES: The weaning of patients under mechanical ventilation (MV) is one of the critical stages of respiratory assistance in intensive care. There are several criteria for taking patients out of respiratory prothesis. The aim of this work was to assess if there is a group of parameter which can predict the patients who will succeed in weaning from mechanical ventilation. METHODS: Sixty patients were studied in a prospective way within 24 months. All of them had been in MV for, time > 48 hours. The specific mechanical parameters were monitored for the weaning, clinical data, gasometrical values and laboratory results. The patients were divided into both succeeding and unsucceeding groups for comparable analysis. By the ROC curve, it was observed the best cut point for the numerical variables evaluated for the success of the weaning. RESULTS: In analysis of logistic regression performed to evaluate the simultaneous influence of all the factors: MV < 8 days, APACHE II (Acute Physiologic and Chronic Health Evaluation II) < 16 and Pimax (maximum respiratory pression) > (-) 20 cmH2O were statistically significant to predict the success to weaning, in this order of explainable capacity. CONCLUSIONS: We could conclude that the indexes evaluated were suitable for the determination of the success in the weaning of those patients in mechanical ventilation. APACHE II because of admition constitutes severity indicator and allows awareness from the patient. MV timing, optimizing the treatment in order to accelerate the process of weaning is conducts that aim not only for the weaning success but also interfere both in the evolution and period of hospital admition.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):444-449
DOI 10.1590/S0103-507X2007000400007
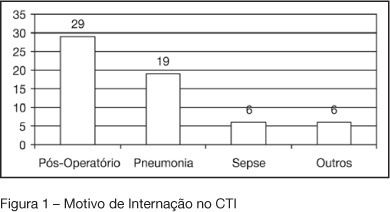
BACKGROUND AND OBJECTIVES: To assess the incidence of tracheostomy in patients submitted to mechanic ventilation (MV); to compare the length of stay (LOS), duration of MV, APACHE II and mortality among patients submitted to tracheostomy, according to the moment of its application (early or late). METHODS: A retrospective observation study type cohort was done from April thru October 2005 including 190 patients at the adult intensive care unit (ICU) of Hospital Estadual do Grajaú. RESULTS: Among the 190 patients, 32 (16.84%) were submitted to tracheostomy with a longer LOS (30.16 days) as compared to those that were not (p < 0.001). The mean time of the tracheostomy procedure was 13.5 days from the starting of the MV. It is known that there still is no guidance for defining an ideal period for the operation. On this study, the prevalence of early tracheostomy (<13 days) was 46.87% (n = 15) and the late tracheostomy (> 13 days) was 53.13% (n = 17). In a meaningful way, the patients with early tracheostomy obtained APACHE II superior to those with late tracheostomy (18.2 versus 13.47), however there was no difference regarding the mortality rate. There was no difference regarding the time of ICU LOS (28.9 versus 31.28 days) and the MV time (29.73 versus 32.23 days) for both groups. CONCLUSIONS: The incidence of tracheostomy was high, being associated to a smaller ICU mortality but with a longer LOS and more complications. There was no significant difference regarding the destination of the patients when submitted to early or late tracheostomy.
Abstract
Rev Bras Ter Intensiva. 2007;19(4):469-474
DOI 10.1590/S0103-507X2007000400011
BACKGROUND AND OBJECTIVES: Mechanical ventilation is considered a basic element of life support in the intensive care unit and is essential for patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS). Experimental studies have demonstrated that mechanical ventilation with high volumes and/or high pressures can exacerbate (VALI) or induce lung injury (VILI) with histological aspect similar to ALI/ARDS. CONTENTS: This systematic review included the literature on MedLine and SciElo database published in the last 20 years. In this review, we will highlight the most recent data on the mechanisms of VILI. The main mechanisms of VILI are: volutrauma caused by overinflation and uneven expansion of the lungs due to high ventilation pressures or volumes; aletectrauma induced by shear forces generated during cyclic closure and reopening of terminal airways; and biotrauma where the injury resulted from the release inflammatory mediators due to physical stresses associated with mechanical ventilation. CONCLUSIONS: It is fundamental to understand the mechanisms related to volutrauma, atelectrauma, and biotrauma to avoid ventilator-associated lung injury.
Abstract
Rev Bras Ter Intensiva. 2007;19(3):399-407
DOI 10.1590/S0103-507X2007000300023
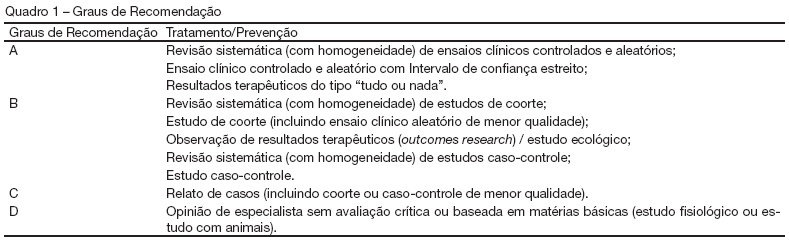
BACKGROUND AND OBJECTIVES: The II Brazilian Consensus Conference on Mechanical Ventilation was published in 2000. Knowledge on the field of mechanical ventilation evolved rapidly since then, with the publication of numerous clinical studies with potential impact on the ventilatory management of critically ill patients. Moreover, the evolving concept of evidence - based medicine determined the grading of clinical recommendations according to the methodological value of the studies on which they are based. This explicit approach has broadened the understanding and adoption of clinical recommendations. For these reasons, AMIB - Associação de Medicina Intensiva Brasileira and SBPT - Sociedade Brasileira de Pneumologia e Tisiologia - decided to update the recommendations of the II Brazilian Consensus. Physical therapy during mechanical ventilation has been one of the updated topics. This objective was described the most important topics on the physical therapy during mechanical ventilation. METHODS: Systematic review of the published literature and gradation of the studies in levels of evidence, using the key words: mechanical ventilation and physical therapy. RESULTS: Recommendations on the most important techniques applied during mechanical ventilation. CONCLUSIONS: Physical therapy has a central role at the Intensive Care environment, mainly in patients submitted to a mechanical ventilatory support invasive or non invasive.