Abstract
Rev Bras Ter Intensiva. 2019;31(4):504-510
DOI 10.5935/0103-507X.20190067
To evaluate the risk factors for protein-caloric inadequacy in critically ill patients.
Prospective cohort study of patients hospitalized in an adult intensive care unit between February and November 2017. Patients were followed for 7 days. The conditional probability of inadequacy was calculated using the Kaplan-Meier method and the 95% log-rank test. To assess the risk of inadequacy, crude and adjusted hazard ratios (HR) were calculated using Cox regression with a 95% confidence interval.
Of the 130 patients, 63.8% were male, 73.8% were <60 years of age, and 49.2% were diagnosed with trauma. The mean APACHE II score was 24 points, and 70.0% of the patients had a protein-caloric adequacy >80%. In the univariate analysis, the significant variables for inadequacy were use of vasoactive drugs, interruptions of diet and failure to initiate nutrition early. In the final model, patients who presented with vomiting/gastric residue (adjusted HR = 22.5; 95%CI 5.14 - 98.87) and fasting for extubation (adjusted HR = 14.75; 95%CI 3.59 - 60.63) and for examinations and interventions (adjusted HR = 12.46; 95%CI 4.52 - 34.36) had a higher risk of not achieving protein-caloric adequacy.
Achievement of nutritional goals > 80.0% occurred in 70.0% of patients. The risk factors for protein-caloric inadequacy were nutritional interruptions, especially due to vomiting/gastric residue and fasting for extubation, exams and surgical procedures.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):326-332
DOI 10.5935/0103-507X.20190041
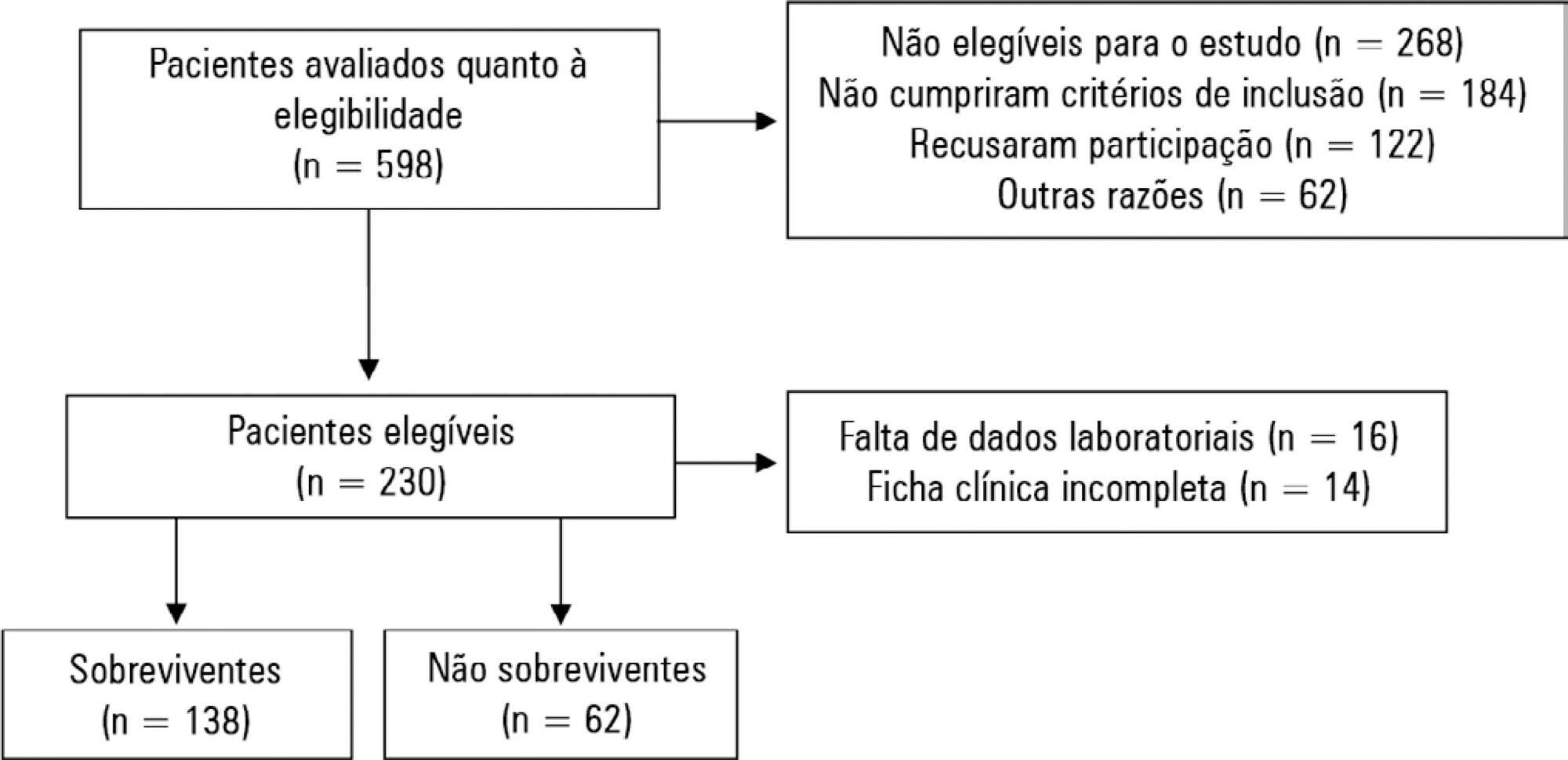
To evaluate possible associations between nutritional risk and the clinical outcomes of critical patients admitted to an intensive care unit.
A prospective study was carried out with a cohort comprising 200 patients admitted to a university hospital intensive care unit. Nutritional risk was assessed with the NRS-2002 and NUTRIC scores. Patients with scores ≥ 5 were considered at high nutritional risk. Clinical data and outcome measures were obtained from patients' medical records. Multiple logistic regression analysis was used to calculate odds ratios and their respective 95% confidence intervals (for clinical outcomes).
This sample of critical patients had a mean age of 59.4 ± 16.5 years and 53.5% were female. The proportions at high nutritional risk according to NRS-2002 and NUTRIC were 55% and 36.5%, respectively. Multiple logistic regression models adjusted for gender and type of admission indicated that high nutritional risk assessed by the NRS-2002 was positively associated with use of mechanical ventilation (OR = 2.34; 95%CI 1.31 - 4.19; p = 0.004); presence of infection (OR = 2.21; 95%CI 1.24 - 3.94; p = 0.007), and death (OR = 1.86; 95%CI 1.01 - 3.41; p = 0.045). When evaluated by NUTRIC, nutritional risk was associated with renal replacement therapy (OR = 2.10; 95%CI 1.02 - 4.15; p = 0.040) and death (OR = 3.48; 95%CI 1.88 - 6.44; p < 0.001).
In critically ill patients, high nutritional risk was positively associated with an increased risk of clinical outcomes including hospital death.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):15-20
DOI 10.5935/0103-507X.20190003
To describe the incidence of clinical and non-clinical events during intrahospital transport of critically ill patients and to analyze the associated risk factors.
Cohort study with retrospective data collected from October 2016 to October 2017. All cases of intrahospital transport for diagnostic and therapeutic purposes in a large hospital with six adult intensive care units were analyzed, and the adverse events and related risk factors were evaluated.
During the study period, 1,559 intrahospital transports were performed with 1,348 patients, with a mean age of 66 ± 17 years and a mean transport time of 43 ± 34 minutes. During transport, 19.8% of the patients were using vasoactive drugs; 13.7% were under sedation; and 10.6% were under mechanical ventilation. Clinical events occurred in 117 transports (7.5%), and non-clinical events occurred in 125 (8.0%) transports. Communication failures were prevalent; however, the multivariate analysis showed that the use of sedatives, noradrenaline and nitroprusside and a transport time greater than 36.5 minutes were associated with adverse clinical events. The use of dobutamine and a transport time greater than 36.5 minutes were associated with non-clinical events. At the end of transport, 98.1% of the patients presented unchanged clinical conditions compared with baseline.
Intrahospital transport is related to a high incidence of adverse events, and transport time and the use of sedatives and vasoactive drugs were related to these events.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):294-300
DOI 10.5935/0103-507X.20180046
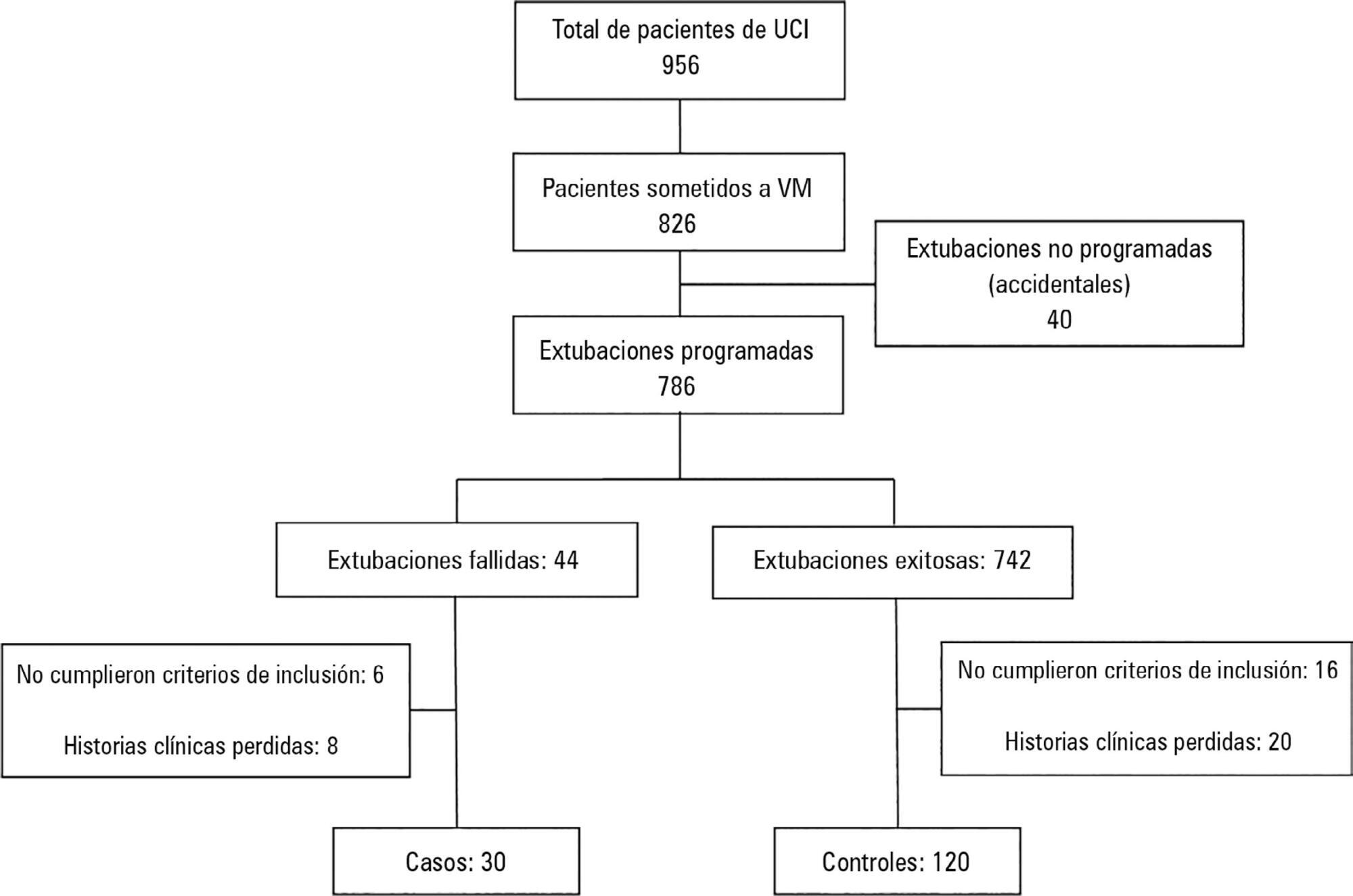
To determine the risk factors for extubation failure in the intensive care unit.
The present case-control study was conducted in an intensive care unit. Failed extubations were used as cases, while successful extubations were used as controls. Extubation failure was defined as reintubation being required within the first 48 hours of extubation.
Out of a total of 956 patients who were admitted to the intensive care unit, 826 were subjected to mechanical ventilation (86%). There were 30 failed extubations and 120 successful extubations. The proportion of failed extubations was 5.32%. The risk factors found for failed extubations were a prolonged length of mechanical ventilation of greater than 7 days (OR = 3.84, 95%CI = 1.01 - 14.56, p = 0.04), time in the intensive care unit (OR = 1.04, 95%CI = 1.00 - 1.09, p = 0.03) and the use of sedatives for longer than 5 days (OR = 4.81, 95%CI = 1.28 - 18.02; p = 0.02).
Pediatric patients on mechanical ventilation were at greater risk of failed extubation if they spent more time in the intensive care unit and if they were subjected to prolonged mechanical ventilation (longer than 7 days) or greater amounts of sedative use.
Abstract
Rev Bras Ter Intensiva. 2018;30(2):174-180
DOI 10.5935/0103-507X.20180023
To compare the neuropsychomotor development in the first year of life of premature infants with and without bronchopulmonary dysplasia.
A cross-sectional retrospective study was conducted between January 1, 2014, and December 30, 2015, with premature infants weighing < 1,500g at birth and diagnosed with bronchopulmonary dysplasia at the corrected ages of 6 and 9 months, assessed using the DENVER II Developmental Screening Test. Quantitative variables were described as the means, medians and standard deviations. Variables with normal distribution were tested using Student's t test; otherwise, the Mann-Whitney test was used, considering significance at p-value < 0.05. Qualitative variables were expressed as frequencies and percentages. Logistic regression was used with odds ratio analysis to evaluate the effects of other variables as risk factors for changes in neuropsychomotor development.
Infants with bronchopulmonary dysplasia showed greater developmental delay compared with those without bronchopulmonary dysplasia (p-value = 0.001). The factors associated with a higher incidence of changes in neuropsychomotor development, in addition to bronchopulmonary dysplasia, were antenatal steroid, gender, birth weight, 5-minute Apgar score, Score for Neonatal Acute Physiology-Perinatal Extension, duration of oxygen therapy, duration of mechanical ventilation and length of hospital stay. Other variables may also have influenced the result, such as drug use by mothers of infants with bronchopulmonary dysplasia.
Bronchopulmonary dysplasia associated with other pre- and postnatal factors may be considered a risk factor for delayed neuropsychomotor development in the first year of life in premature infants born weighing less than 1,500g.
Abstract
Rev Bras Ter Intensiva. 2017;29(2):195-205
DOI 10.5935/0103-507X.20170019
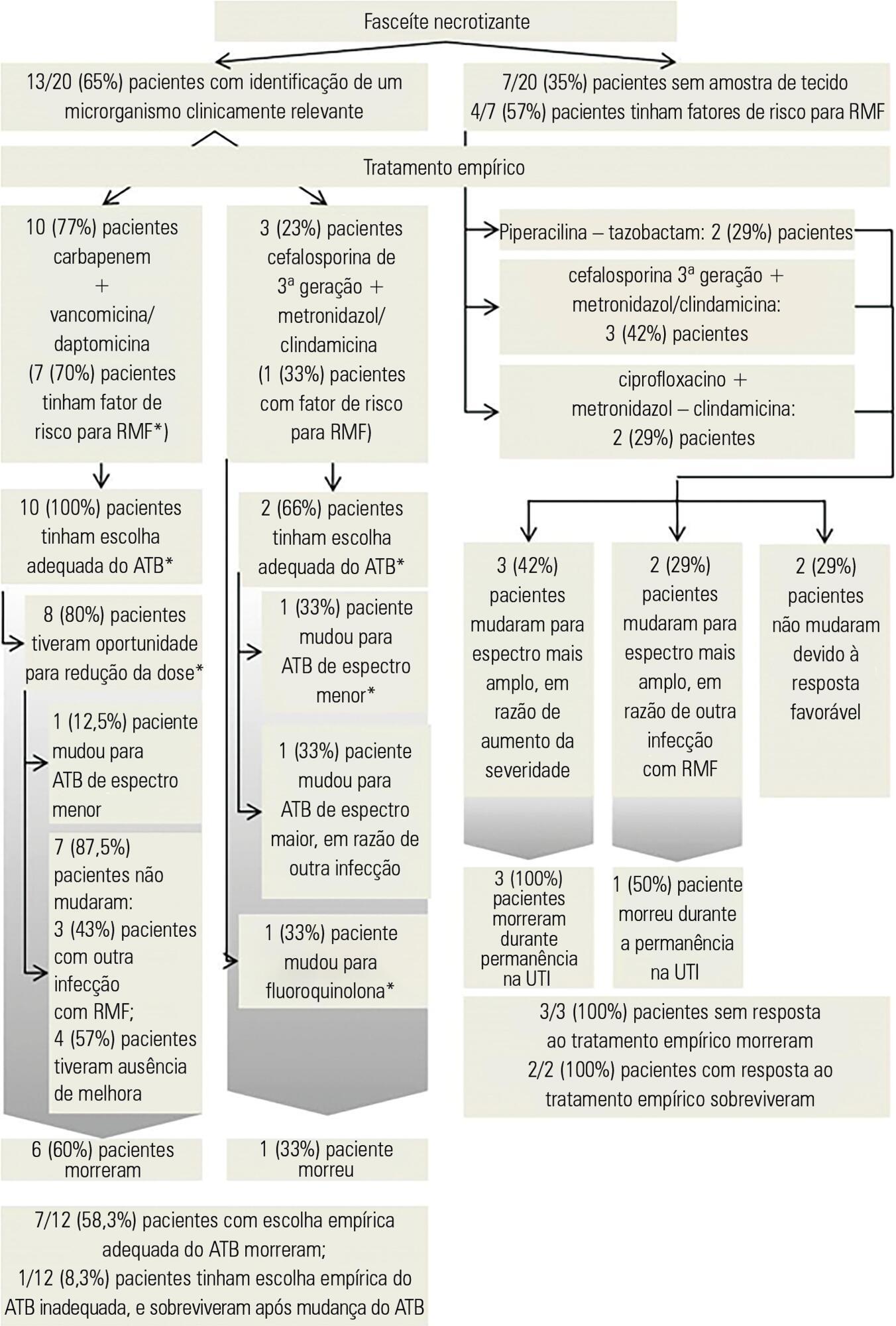
To identify factors that may influence outcomes in patients with severe skin and soft tissue infections in the intensive care unit.
A retrospective observational study was conducted in a cohort of 1,123 critically ill patients admitted to an intensive care unit with a primary or secondary diagnosis of severe skin and soft tissues infection between January 2006 and December 2014.
Thirty patients were included, 20 (66.7%) of whom were diagnosed with necrotizing fasciitis; in these patients, perineal area involvement was most commonly identified. Abscess was diagnosed in 8 (26.7%) patients, most commonly involving the cervical area. Risk factors such as immunosuppression and previous surgical trauma were commonly observed in this population. The most commonly isolated microorganism was Escherichia coli. Multidrug resistant microorganisms were commonly detected, even in the absence of traditional risk factors; among these patients, previous use of antibiotics was the most common risk factor for drug resistance. The rate of mortality was significantly higher in patients with necrotizing fasciitis (55%, p = 0.035) and associated with disease severity, presence of septic shock, cardiac arrest and leucocytosis.
Different risk factors and etiologies of severe skin and soft tissue infections were identified. Necrotizing fasciitis and drug-resistant bacteria were significant predictors of mortality, even in the absence of traditional risk factors. Obtaining a better understanding of trends in the risk factors and microorganisms associated with severe skin infections may help in the determination of prompt treatment and antibiotic choices.