Abstract
Rev Bras Ter Intensiva. 2011;23(3):321-326
DOI 10.1590/S0103-507X2011000300010
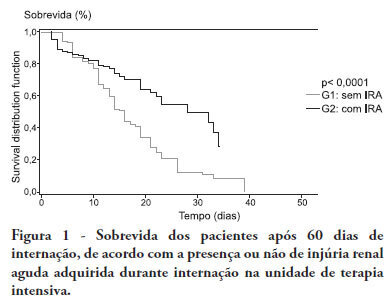
OBJECTIVE:To compare the clinical features and outcomes of patients with and without acute kidney injury in an intensive care unit of a tertiary university hospital and to identify acute kidney injury and mortality risk factors. METHODS: This was a prospective observational study of a cohort including 564 patients followed during their stay in the intensive care unit of Hospital das Clinicas da Faculdade de Medicina de Botucatu (Botucatu, São Paulo, Brazil) between May 2008 and May 2010. Patients were allocated to two different groups: with (G1) and without (G2) acute kidney injury. RESULTS: The incidence of acute kidney injury was 25.5%. The groups were different with respect to the reason for admission to the intensive care unit (sepsis, G1: 41.6% versus G2: 24.1%; P < 0.0001; neurosurgery, postoperative G1: 13.8% versus G2: 38.1%; P < 0.0001); age (G1: 56.8 ± 15.9 vs. G2: 49.8 ± 17.8 years; P < 0.0001); Acute Physiological Chronic Health Evaluation (APACHE) II score (G1: 21.9 ± 6.9 versus G2: 14.1 ± 4.6; P < 0.0001); use of mechanical ventilation (G1: 89.2% vs. G2: 69.1%; P < 0.0001) and use of vasoactive drugs (G1: 78.3% vs. G2: 56.1%; P < 0.0001). Higher rates of diabetes mellitus, congestive heart failure, chronic renal disease and use of non-steroidal anti-inflammatory drugs were more frequent in acute kidney injury patients (28.2% vs. 19.7%, P = 0.03; 23.6 vs. 11.6%, P = 0.0002; 21.5% vs. 11.5%, P < 0.0001 and 23.5% vs. 71.%, P < 0.0001, for G1 versus G2, respectively). Length of hospital stay and mortality were also higher for acute kidney injury patients (G1: 6.6 ± 2.7 days versus G2: 12.9 ±5.6 days, P < 0.0001 and G1: 62.5% versus G2: 16.4%, P < 0.0001). Multivariate analysis identified the following as risk factors for acute kidney injury: age above 55 years, APACHE II score above 16, baseline creatinine above 1.2 and use of non-steroidal anti-inflammatory drugs (odds ratio (OR) = 1.36, 95% confidence interval (95%CI): 1.22 - 1.85; OR = 1.2, 95%CI: 1.11 - 1.33; OR = 5.2, 95%CI: 2.3 - 11.6 and OR = 2.15, 95%CI: 1.1 - 4.2, respectively). Acute kidney injury was independently associated with longer hospital stay and increased mortality (OR = 1.18, 95%CI: 1.05 - 1.26 and OR = 1.24, 95%CI: 1.09 - 1.99, respectively). Analysis of the survival curve 30 days after admission showed 83.3% mortality for acute kidney injury patients and 45.2% for non-acute kidney injury patients (P < 0.0001). CONCLUSION: The incidence of acute kidney injury was high in this intensive care unit; the independent risk factors associated with acute kidney injury were age > 55 years, APACHE II > 16, baseline serum creatinine > 1.2 and use of non-steroidal anti-inflammatory drugs. Acute kidney injury is an independent risk factor for longer intensive care unit stay and mortality.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):327-334
DOI 10.1590/S0103-507X2011000300011
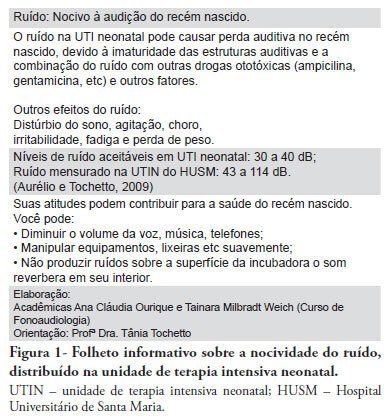
PURPOSE: To evaluate the effectiveness of a noise control program in the Neonatal Intensive Care Unit of the Hospital Universitário Santa Maria (NICU-HUSM) in Santa Maria, Rio Grande do Sul, Brazil. METHODS: NICU-HUSM professionals were initially contacted through informal interviews during the morning, afternoon and night shifts. Leaflets were delivered and posters were installed to raise awareness of the harmful effects of noise on neonates and professionals and to suggest behavioral changes to reduce noise levels. The suggestions included avoiding loud talking, careful handling of the incubator doors and keeping mobile phones on silent mode. One month later, questionnaires were used to assess behavioral changes since the first contact. RESULTS: Most of the professionals rated the NICU-HUSM noise level as moderate. Overall, 71.4% of the respondents acknowledged that their behaviors were noisy. The entire sample reported believing that the unit noise levels could be reduced by speaking lower, reacting more quickly to alarms and handling furniture more carefully. The NICU professionals reported adopting these behaviors. CONCLUSION: This noise control program was considered successful because the professionals became aware of the level of noise and adopted behavioral changes to avoid generating unnecessary noise.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):335-340
DOI 10.1590/S0103-507X2011000300012
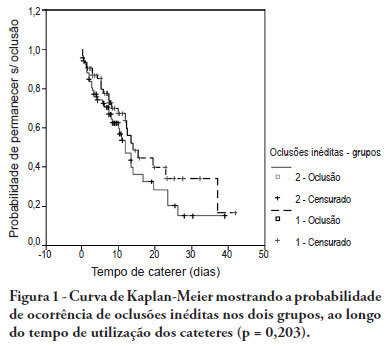
OBJECTIVE: To evaluate the effectiveness of intermittent 10 U/mL heparin flushes in reducing the occlusion of peripherally inserted central catheters in neonates. METHODS: In this randomized, open-label, prospective, controlled study, neonates were allocated either to receive 0.5 mL flushes of heparin (Group 1: n = 64) or saline (Group 2: n = 69) every 4 hours. Actions were taken to restore patency by using negative pressure (3-way stopcock method) in cases of occlusion. RESULTS: A total of 133 neonates were included. No significant intergroup difference was observed in the number of new occlusions (26 in Group 1, or 31/1,000 catheter-days; 36 in Group 2, or 36/1,000 catheter-days; P = 0.19). In Group 1, 5 catheters had 9 recurrent obstructions after successful clearance maneuvers. In Group 2, 19 catheters had 40 relapses (P < 0.0001), showing heparin's protective role against recurrence of obstruction (Relative Risk = 0.36). However, heparin failed to prevent catheter withdrawal due to permanent occlusion (3 catheters in Group 1 and 8 in Group 2; P = 0.24). CONCLUSION: Intermittent heparin is not effective for preventing the occlusion of peripherally inserted central catheters in neonates but reduces relapses when clearance maneuvers were successful
Abstract
Rev Bras Ter Intensiva. 2011;23(3):291-296
DOI 10.1590/S0103-507X2011000300006
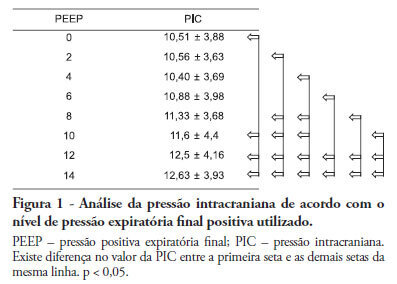
Positive intrathoracic pressure may cause hemodynamic changes, which can be transmitted to the cranial compartment, changing intracranial pressure and cerebral perfusion pressure. This can be increased when high positive end-expiratory pressure values are used. OBJECTIVE: To measure the impact of different positive end-expiratory pressure levels on intracranial pressure, cerebral perfusion pressure and mean blood pressure. METHOD: This study was conducted in a neurological intensive care unit and included 25 adult hemorrhagic stroke patients who were mechanically ventilated on airway pressure control mode. Patients were subjected to various positive end-expiratory values ranging between 0 and 14 cmH2O. The order of these values were randomized, and the variables were assessed five minutes after each new positive end-expiratory pressure level was initiated. RESULTS: Incremental positive end-expiratory pressures led to increased intracranial pressure (p < 0.001), however, no statistically significant changes were observed in mean blood pressure or cerebral perfusion pressure. CONCLUSION: In this population of patients with hemorrhagic stroke, positive end-expiratory pressure values up to 14 cmH2O did not alter cerebral perfusion pressure or mean blood pressure. Increased intracranial pressures were noted, although these elevations were not clinically significant
Abstract
Rev Bras Ter Intensiva. 2011;23(3):297-303
DOI 10.1590/S0103-507X2011000300007
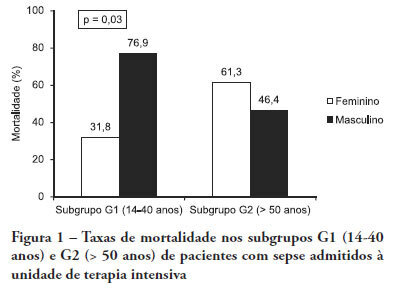
OBJECTIVE: Comparative assessment of the mortality rates of two septic patients' ages and/or gender subgroups, admitted to the intensive care unit of a university hospital. METHODS: From December 2005 to April 2008, from a total of 628 patients, 133 were admitted to the intensive care unit with sepsis and included into two age subgroups: (G1) 14 - 40 years old and (G2) more than 50 years old. Patients aged between 41 and 50 years old (n = 8) were excluded. Demographic data, prognostic indicators (APACHE II score, organ dysfunction and circulatory shock) and outcome (mortality) were analyzed. RESULTS: Of the G1 patients (n = 44), 27 were female (61.4%), and in G2 (n = 81), 40 were female (49.4%). For both groups, mean APACHE II scores, multi-organ dysfunction and progression to circulatory shock rates were not significantly different between female and male patients. For G1, overall mortality rate was lower in female than in male patients (P = 0.04), while for G2, the opposite trend was observed. CONCLUSIONS: In this sample, reproductive age female patients younger than 40 years old showed lower mortality rates compared with age-matched male patients; for patients older than 50 years old, male patients had lower mortality rates than female patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):304-311
DOI 10.1590/S0103-507X2011000300008
OBJECTIVES: Ascending aortic dissection has a poor prognosis if it is not promptly corrected surgically. Even with surgical correction, postoperative management is feared because of its complicated course. Our aim was to describe the incidence of postoperative complications and identify the 1 and 6-month mortality rate of our ascending aortic dissection surgical cohort. Secondarily, a comparison was made between ascending aortic dissection patients and paired-matched patients who received urgent coronary artery bypass graft surgery. METHODS: A retrospective analysis of a prospectively-collected database from February 2005 through June 2008 revealed 12 ascending aortic dissection and 10 elective ascending aortic aneurysm repair patients. These patients were analyzed for demographic and perioperative characteristics. Ascending aortic dissection patients were compared to paired-matched coronary artery bypass graft surgery patients according to age (± 3 years), gender, elective/urgent procedure and surgical team. The main outcome was in-hospital morbidity, defined by postoperative complications, intensive care unit admission and hospital length of stay. RESULTS: Twenty-two patients received operations to correct ascending aortic dissections and ascending aortic aneurysms, while 246 patients received coronary artery bypass graft surgeries. Ascending aortic dissection patients were notably similar to ascending aortic aneurysm brackets, except for longer mechanical ventilation times and lengths of stay in the hospital. After matching coronary artery bypass graft surgery patients to an ascending aortic dissection group, the following significantly worse results were found for the Aorta group: higher incidence of postoperative complications (91% vs. 45%, p=0.03), and longer hospital length of stay (19 [11-41] vs. 12.5 [8.5-13] days, p=0.05). No difference in mortality was found at the 1-month (8.3%) or 6-month (16.6%) postoperative care date. CONCLUSION: Ascending aortic dissection correction is associated with an increased incidence of postoperative complications and an increased hospital length of stay, but 1 and 6-month mortality is similar to that of paired-matched coronary artery bypass graft surgery patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)