Abstract
Rev Bras Ter Intensiva. 2011;23(4):462-469
DOI 10.1590/S0103-507X2011000400011
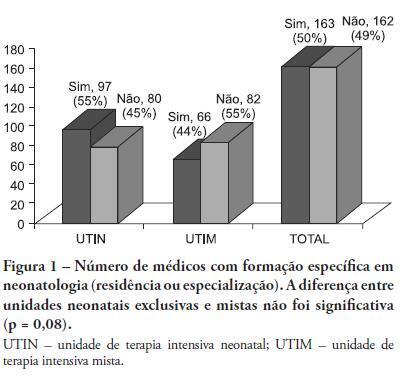
OBJECTIVE: This study described the sociodemographic profile and professional qualifications of pediatric intensive care physicians in the State of Rio de Janeiro (RJ), southeastern Brazil. METHODS: This investigation was an observational, cross-sectional and descriptive study that was conducted in neonatal, pediatric and mixed intensive care units in the State of Rio de Janeiro. Physicians working in the participating intensive care units voluntarily completed a semistructured and anonymous questionnaire. Questionnaires that were not returned within 30 days were considered lost, and questionnaires with less than 75% questions completed were excluded. The differences in neonatal and pediatric intensive care physicians' medical training were compared using the Chi-squared test with a 5% significance level. RESULTS: A total of 410 physicians were included in this study: 84% female, 48% between 30 and 39 years old and 45% with monthly incomes between US $1,700 to 2,700. Forty percent of these physicians worked exclusively in this specialty, and 72% worked in more than one intensive care unit. Only 50% of the participants had received specific training (either medical residency or specialization) in neonatology, and only 33% were board-certified specialists in this area. Only 27% of the physicians had received specific training in pediatric intensive care medicine, and only 17% were board-certified specialists (p < 0.0005 for both comparisons). Most (87%) physicians had participated in scientific events within the past 5 years, and 55% used the internet for continued medical education. However, only 25% had participated in any research. Most (63%) physicians were dissatisfied with their professional activity; 49% were dissatisfied due to working conditions, 23% due to low incomes and 18% due to training-related issues. CONCLUSION: These results suggested that the medical qualifications of neonatal and pediatric intensive care physicians in the State of Rio de Janeiro, Brazil are inadequate, especially in pediatric intensive care medicine. A high level of dissatisfaction was reported, which may jeopardize the quality of medical assistance that is provided by these professionals.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):434-441
DOI 10.1590/S0103-507X2011000400007
OBJECTIVE: Despite the decline in the incidence of tetanus, this disease is still neglected in the developing world and remains a major cause of morbidity and mortality. With improvements in intensive care, it is important to better understand the complications of this serious condition. We aim to evaluate 1) the lethality and osteomuscular and cardiovascular complications of patients with tetanus who are admitted to the intensive care unit (ICU) and 2) the risk factors associated with a poor prognosis. METHODS: This was a retrospective study that analyzed the medical records of all of the patients diagnosed with tetanus who were admitted to an infectious diseases ICU between January 2000 and December 2001. A standardized form that included demographic, clinical and laboratory data was completed. The clinical variables that were related to lethality and osteomuscular and cardiovascular complications were described. RESULTS: A total of 22 tetanus patients were admitted (81.8% male, mean age of 47.8 years).The tetanus infection was associated with professional activities in 54.5% of cases. The majority of patients (20 patients) presented with the generalized form of disease. Eighty-one percent of the patients had never received a tetanus vaccine or were unaware of their vaccine status. Following the injury, none had received appropriated passive prophylaxis, only two patients had received surgical debridement of wound and six patients received antibiotic therapy. Eleven patients (52.4%) experienced some cardiovascular complication. A pressure ulcer was the most frequent cardiovascular complication (38.1%), followed by arrhythmias (28.6%). Two of the patients developed bone fractures secondary to tetanus spasms, corresponding to 9.6% of sample. The tetanus lethality rate was 9.1%. Higher APACHE II severity scores and very severe status based on the Veronesi tetanus classification were significantly associated with the risk of death (p=0.04 and 0.03, respectively). The Veronesi classification was also associated with the risk of cardiovascular complications (p=0.013) and the length of the ICU stay (p=0.009). CONCLUSION: The present study demonstrates the failure of primary medical care in vaccination and post-traumatic tetanus prophylaxis. Despite improvements in intensive care support, cardiovascular complications are still frequent in these patients. Individuals exhibiting high APACHE II scores and severe clinical forms of tetanus should be monitored closely due to a risk of death and cardiovascular complications.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):442-447
DOI 10.1590/S0103-507X2011000400008
INTRODUCTION: The importance of autopsies is a common theme of discussions both in Brazil and around the world as it elucidates causes of death and has wide ranging social value. However this is a practice that is gradually being considered unnecessary and there have been a decline in the number of postmortems examinations. OBJECTIVES: To compare clinical and pathological diagnosis in critically ill patients with difficult premortem diagnosis. METHODS: All autopsy cases (total of 98) from any of the three general medical/surgical intensive care units (78 beds in total) affiliated to the medical school from January 2003 to December 2006 were analyzed. We analyzed the clinical and pathological diagnosis based on the Goldman criteria. RESULTS: In 49 (50%) cases, there were class I and II of Goldman. In contrast, only 30 (30.6%) had a complete agreement between premortem and postmortem diagnosis and were classified as class V. Infections had a significantly greater rate of concordant diagnosis than cardiovascular diseases. CONCLUSION: We found significant discrepancies between clinical and pathological findings, reinforcing the value of postmortem examination.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):448-454
DOI 10.1590/S0103-507X2011000400009
OBJECTIVES: This study aimed to assess family member acceptance of orthotanasia as related to symptom management, patient preference and the influence of the medical team's communication on therapy. METHODS: This was a descriptive one-year study conducted at the adult intensive care unit of the Hospital do Servidor Público Estadual. A structured questionnaire based on the Quality of Dying and Death (QODD 22) instrument and prior informal interviews were used. RESULTS: Sixty family members were assessed; the mean age was 51.7 + 12.1 years, and 81.7% were female. The patients were hospitalized for a mean of 31 + 26.9 days, and 17.0% of these days were spent in the intensive care unit. Most of the patients had neurological conditions. Most of the patients (53.3%) had discussed their end-of-life care wishes with family members; however, 76.7% of them had not discussed this issue with their doctors (p < 0.00). The family members reported being favorable to orthotanasia in 83.3% of the cases. Most (85.0%) desired the medical team to clearly approach the subject, and 65.0% wished to take part in the quality of end-of-life decision making process. The family members were generally satisfied with information they received from the doctors: 93.3% believed they had received appropriately frequent communications about the clinical conditions; 81.7% were able to clarify their doubts regarding the patient's clinical status; the communication was understood by 83.3% of the respondents; and 80.0% believed that clear and honest information had been provided. Only 43.3% of the respondents wished to be present at the time of their loved ones' deaths. A significant association between family member acceptance of orthotanasia and participation in end-of-life decisions (p = 0.042) was observed. CONCLUSIONS: Most of the respondents were favorable to orthotanasia and wished to participate in end-of-life discussions.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):455-461
DOI 10.1590/S0103-507X2011000400010
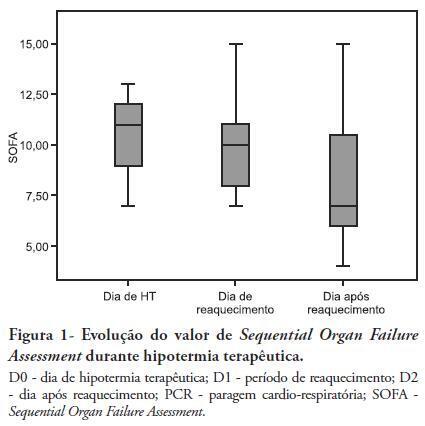
OBJECTIVES: Therapeutic hypothermia following cardiorespiratory arrest has been demonstrated to have cardio- and neuroprotective effects, resulting in improved survival and better neurological outcomes. The objective of this study was to assess the outcomes of patients undergoing therapeutic hypothermia following cardiorespiratory arrest. METHODS: A prospective, 10-month observational study of patients admitted to an intensive care unit and undergoing therapeutic hypothermia after cardiorespiratory arrest was undertaken. Therapeutic hypothermia was induced by cold fluid administration and body surface cooling in patients admitted no more than 12 hours after resuscitation from cardiorespiratory arrest. A target temperature of 33ºC was maintained for 24 hours. RESULTS: Overall, 12 patients were included (median age 64 years, 58% male). Half of the cardiorespiratory arrests were in-hospital. The median first-day Charlson Index, Sequential Organ Failure Assessment (SOFA) and Acute Physiology and Chronic Health Evaluation II scores were of 2.9, 11 and 24.5, respectively. The intensive care unit mortality rate was 42% (N=5). Five of the 7 surviving patients recovered their pre-cardiorespiratory arrest neurological status. Hypothermia was initiated 120 min (median) after recovery of spontaneous circulation. Most patients (75%) required vasopressor support. During the first 3 days after cardiorespiratory arrest and therapeutic hypothermia, a progressive SOFA score decrease (median 11 on day 0, 10 on day 1 and 7 on day 2) was observed. DISCUSSION: In this study, therapeutic hypothermia was applied to all post-cardiorespiratory arrest patients and demonstrated good neurological outcome in surviving patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):470-477
DOI 10.1590/S0103-507X2011000400012
OBJECTIVE: This study assessed the role of the nursing staff in pain management and verified the pain experiences of patients undergoing major surgery and receiving postoperative care in the intensive care unit. METHOD: This was a prospective, observational study of postoperative patients who were admitted to the intensive care unit and later discharged to one of the hospital's regular wards. Patients with impaired communication were excluded. All patients signed an informed consent form. Data were collected using a questionnaire of 13 pain-related questions. RESULTS: A total of 167 patients were included, and 69.5% were male. Patient age ranged from 50-59 years, and the intensive care unit stay was one to three days. The majority of the patients (85%) reported no difficulties in expressing their painful symptoms, and the nursing approach in 54.5% of patients was only to recognize the presence or absence of pain. No pain scale was used. The most painful conditions included the surgical wound and bed positioning. CONCLUSION: The nursing team was apparently more concerned with the presence of pain than with its quality, severity or possible painful stimuli. Pain scales were not used, which suggests the need for continued education of the nursing professionals on the manner of approaching their patients and assessing their patients' pain.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):478-483
DOI 10.1590/S0103-507X2011000400013
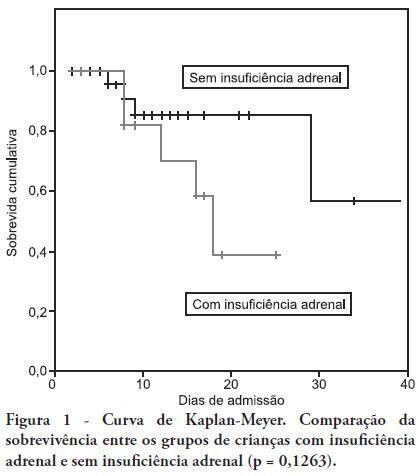
OBJECTIVE: To determine the frequency of adrenal insufficiency in children diagnosed with sepsis that were staying in pediatric intensive care units and to establish the association between adrenal function and the use of vasoactive drugs, mechanical ventilation time and mortality. METHODS: A cohort-designed study was conducted to assess the incidence of adrenal insufficiency in children aged 29 days to 12 years who were diagnosed with sepsis using the adrenocorticotropic hormone (ACTH) stimulation test. RESULTS: Thirty-nine children were included in the study. The frequency of adrenal insufficiency was 30.7% (12 patients). Children with adrenal insufficiency had an increased need for vasoactive drugs as well as longer mechanical ventilation times; however, the differences were not statistically significant. A Kaplan-Meier curve indicated lower survival rates among the adrenal insufficiency children, but the differences were not statistically significant (p = 0.1263). No differences were identified between the adrenal sufficiency and adrenal insufficiency groups in regards to mechanical ventilation time, use of vasoactive drugs, infection type and chronic disease. CONCLUSION: This study determined the frequency of adrenal insufficiency in children with sepsis and its relationship to increased mortality within the first 28 post-admission days. No statistically significant association was found between adrenal insufficiency and mechanical ventilation time or the use of vasoactive drugs.
Abstract
Rev Bras Ter Intensiva. 2011;23(3):291-296
DOI 10.1590/S0103-507X2011000300006
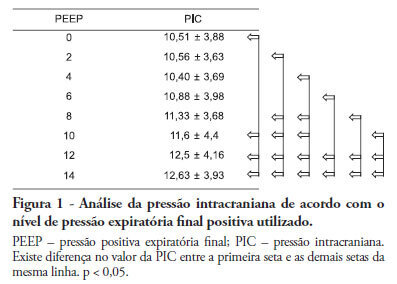
Positive intrathoracic pressure may cause hemodynamic changes, which can be transmitted to the cranial compartment, changing intracranial pressure and cerebral perfusion pressure. This can be increased when high positive end-expiratory pressure values are used. OBJECTIVE: To measure the impact of different positive end-expiratory pressure levels on intracranial pressure, cerebral perfusion pressure and mean blood pressure. METHOD: This study was conducted in a neurological intensive care unit and included 25 adult hemorrhagic stroke patients who were mechanically ventilated on airway pressure control mode. Patients were subjected to various positive end-expiratory values ranging between 0 and 14 cmH2O. The order of these values were randomized, and the variables were assessed five minutes after each new positive end-expiratory pressure level was initiated. RESULTS: Incremental positive end-expiratory pressures led to increased intracranial pressure (p < 0.001), however, no statistically significant changes were observed in mean blood pressure or cerebral perfusion pressure. CONCLUSION: In this population of patients with hemorrhagic stroke, positive end-expiratory pressure values up to 14 cmH2O did not alter cerebral perfusion pressure or mean blood pressure. Increased intracranial pressures were noted, although these elevations were not clinically significant