You searched for:"Francisco Albano de Meneses"
We found (7) results for your search.-
Original Articles – Clinical Research
Gender and mortality in sepsis: do sex hormones impact the outcome?
Rev Bras Ter Intensiva. 2011;23(3):297-303
Abstract
Original Articles – Clinical ResearchGender and mortality in sepsis: do sex hormones impact the outcome?
Rev Bras Ter Intensiva. 2011;23(3):297-303
DOI 10.1590/S0103-507X2011000300007
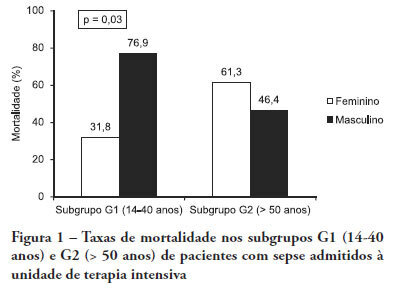
Views0See moreOBJECTIVE: Comparative assessment of the mortality rates of two septic patients’ ages and/or gender subgroups, admitted to the intensive care unit of a university hospital. METHODS: From December 2005 to April 2008, from a total of 628 patients, 133 were admitted to the intensive care unit with sepsis and included into two age subgroups: (G1) 14 – 40 years old and (G2) more than 50 years old. Patients aged between 41 and 50 years old (n = 8) were excluded. Demographic data, prognostic indicators (APACHE II score, organ dysfunction and circulatory shock) and outcome (mortality) were analyzed. RESULTS: Of the G1 patients (n = 44), 27 were female (61.4%), and in G2 (n = 81), 40 were female (49.4%). For both groups, mean APACHE II scores, multi-organ dysfunction and progression to circulatory shock rates were not significantly different between female and male patients. For G1, overall mortality rate was lower in female than in male patients (P = 0.04), while for G2, the opposite trend was observed. CONCLUSIONS: In this sample, reproductive age female patients younger than 40 years old showed lower mortality rates compared with age-matched male patients; for patients older than 50 years old, male patients had lower mortality rates than female patients.
-
Review Articles
End of life and palliative care in intensive care unit
Rev Bras Ter Intensiva. 2008;20(4):422-428
Abstract
Review ArticlesEnd of life and palliative care in intensive care unit
Rev Bras Ter Intensiva. 2008;20(4):422-428
DOI 10.1590/S0103-507X2008000400016
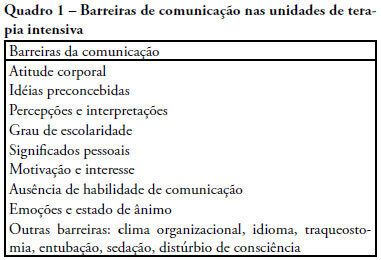
Views0See moreThe objective of this review was to evaluate current knowledge regarding terminal illness and palliative care in the intensive care unit, to identify the major challenges involved and propose a research agenda on these issues The Brazilian Critical Care Association organized a specific forum on terminally ill patients, to which were invited experienced and skilled professionals on critical care. These professionals were divided in three groups: communication in the intensive care unit, the decision making process when faced with a terminally ill patient and palliative actions and care in the intensive care unit. Data and bibliographic references were stored in a restricted website. During a twelve hour meeting and following a modified Delphi methodology, the groups prepared the final document. Consensual definition regarding terminality was reached. Good communication was considered the cornerstone to define the best treatment for a terminally ill patient. Accordingly some communication barriers were described that should be avoided as well as some approaches that should be pursued. Criteria for palliative care and palliative action in the intensive care unit were defined. Acceptance of death as a natural event as well as respect for the patient’s autonomy and the nonmaleficence principles were stressed. A recommendation was made to withdraw the futile treatment that prolongs the dying process and to elected analgesia and measures that alleviate suffering in terminally ill patients. To deliver palliative care to terminally ill patients and their relatives some principles and guides should be followed, respecting individual necessities and beliefs. The intensive care unit staff involved with the treatment of terminally ill patients is subject to stress and tension. Availability of a continuous education program on palliative care is desirable.
-
Original Articles
Characteristics of patients with systemic lupus erythematosus admitted to the intensive care unit in a brazilian teaching hospital
Rev Bras Ter Intensiva. 2008;20(3):249-253
Abstract
Original ArticlesCharacteristics of patients with systemic lupus erythematosus admitted to the intensive care unit in a brazilian teaching hospital
Rev Bras Ter Intensiva. 2008;20(3):249-253
DOI 10.1590/S0103-507X2008000300007
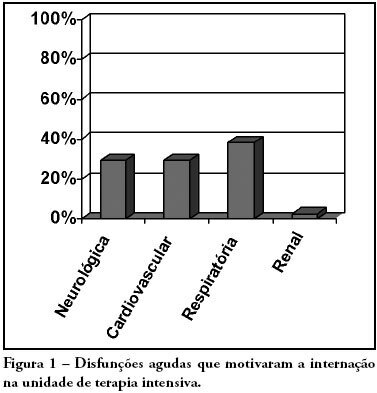
Views0See moreOBJECTIVES: Due to the high incidence in our service, we did object on this study describe the features and outcome of patients with systemic lupus erythematosus (SLE) admitted to the intensive care unit of Walter Cantídio University Hospital METHODS: Patients were restrospectively characterized according to demography parameters, time of diagnosis of SLE, organ dysfunction and laboratorial parameters at admission, supportive therapies during their stay, length of stay in the hospital before admission, length of stay in the unit, readmission to the unit and outcome. We also evaluated Systemic Lupus Erythematosus Disease Activity (SLEDAI) score, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, expected mortality and standardized mortality ratio. RESULTS: From November 2003 to October 2006, 1,052 patients were admitted to the intensive care unit. Fifty patients had SLE and were included in this retrospective study. Of the 50 patients with SLE admitted to the ICU, 88.2% were female. The mean age was 30.3 ± 12.8 years. The median time of diagnosis of SLE was 67 months. The most common organ dysfunctions were renal (70.6%), cardiovascular (61.8%), respiratory (55.9%) and neurological (55.9%). The main reasons for admission to the ICU were respiratory (38.2%), cardiologic (29.4%) and neurological (29.4%) dysfunctions. Among the intensive care therapies, 44.1% of the patients needed blood products, 41.2% vasopressor agents and 35.3% mechanical ventilation, 23.5% dialysis. The mean SLEDAI score was 15.0 ± 12.2. The mean APACHE II score was 19.3 ± 6.8, with a predicted mortality rate of 37.6%. The actual mortality rate in ICU was 29.4%, with 8.8% before 48 hours. The standardized mortality ratio was 0.78. Patients with APACHE II > 18, with more than 3 acute organ involvements, leukopenia (< 4000 cells/mm3) and gastrointestinal or metabolic involvement had higher mortality in the intensive care unit. CONCLUSION: Although the severity of patients at admission to the ICU, demonstrated by APACHE II and the acute dysfunctions, the outcomes of analysed patients sugest susceptibility to the therapy.
-
Original Articles
Validation of an early warning score in pre-intensive care unit
Rev Bras Ter Intensiva. 2008;20(2):124-127
Abstract
Original ArticlesValidation of an early warning score in pre-intensive care unit
Rev Bras Ter Intensiva. 2008;20(2):124-127
DOI 10.1590/S0103-507X2008000200002
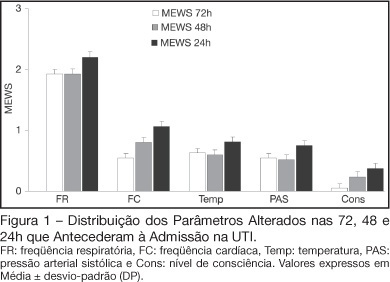
Views0See moreBACKGROUND AND OBJECTIVES: Prognosis of patients in the intensive care unit (ICU) has a relation with their severity just before admission. The Modified Early Warning Score (MEWS) was used to evaluate the severe condition of patients 12, 24 and 72 hours before admission in the ICU, assess the most prevalent parameters and correlate the MEWS before ICU with the outcome (survival versus death). METHODS: Retrospective analyses of 65 patients consecutively admitted to the ICU from July to October, 2006 evaluating the physiological parameters 72 hours prior to admission. RESULTS: APACHE II mean was 22.2 ± 7.9 points, mortality was 54.6% and standardized mortality ratio means was 1.24. MEWS means were 3.7 ± 0.2; 4.0 ± 0.2 and 5.1 ± 0.2 points, calculated 72, 48 and 24 hours previous to ICU admission, respectively. An increasing percentage of patients with MEWS > 3 points within 72, 48 and 24 hours before admission – 43.8%, 59.4% and 73.4%, respectively was recorded. Among the included physiological parameters respiratory rate contributed the most to the MEWS. Highest mortality was found in patients with MEWS > 3 points already found 72 hours before admission. Patients who died presented with a significant increase in the MEWS 24 hours prior to admission to the ICU (in relation to the MEWS recorded 72 hours before) but the situation was not identified in survivors. CONCLUSIONS: MEWS closely identified the severity of patients admitted to the ICU, suggesting that it can be a reliable score, useful in the situations preceding the ICU.
-
Artigo Original
Severity of patients admitted to a Brazilian teaching hospital Intensive Care Unit
Rev Bras Ter Intensiva. 2006;18(1):18-21
Abstract
Artigo OriginalSeverity of patients admitted to a Brazilian teaching hospital Intensive Care Unit
Rev Bras Ter Intensiva. 2006;18(1):18-21
DOI 10.1590/S0103-507X2006000100004
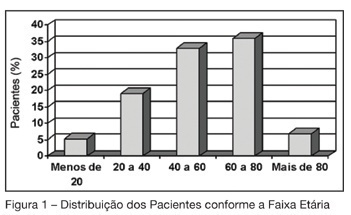
Views0See moreBACKGROUND AND OBJECTIVES: The aim of this study was to analyze the morbidity and the mortality of critically ill patients admitted to the intensive care unit in a teaching hospital, using the APACHE II score. METHODS: Descriptive and retrospective study, with analysis of 300 patients admitted to ICU from March 2004 to July 2005. RESULTS: Of the 300 patients admitted to ICU, 51.7% were men, average 54.2 ± 19.57 years and 78% from the wards of the teaching hospital itself. There was more prevalence of patients aged 60 years or older (43%). The main dysfunctions were from the respiratory and cardiocirculatory systems. Length of stay in ICU was 7.51 ± 8.21 days. The mean of APACHE II was 16.48 ± 7.67, with meaningful difference between survivors and deceased patients. The real mortality rate in ICU was 32.7%, without meaningful difference between patients that died before or after 48 hours. The standardized mortality ratio was 1.1. CONCLUSIONS: Despite the severity of the patients admitted to ICU, the standardized mortality ratio suggests a satisfactory quality in the service.
-
Morbidity and mortality of elderly patients admitted to an Intensive Care Unit of a University Hospital in Fortaleza
Rev Bras Ter Intensiva. 2006;18(3):263-267
Abstract
Morbidity and mortality of elderly patients admitted to an Intensive Care Unit of a University Hospital in Fortaleza
Rev Bras Ter Intensiva. 2006;18(3):263-267
DOI 10.1590/S0103-507X2006000300008
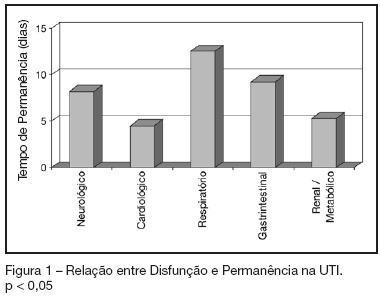
Views0See moreBACKGROUND AND OBJECTIVES: To identify the severity of elderly patients admitted to the intensive care unit (ICU) in a university hospital, relating it to the in-ICU mortality. METHODS: Retrospective study, with analysis of 130 patients admitted to ICU from March 2004 to July 2005. RESULTS: Of the 130 patients, there was a predominance of women, and mean 72.2 ± 7.3 years. There were more patients between 65 and 74 years old. More than 80% of the patients had come from the university hospital itself. The main dysfunctions were from the cardiocirculatory and respiratory systems. Sepsis caused 23.8% of the admissions. Length of stay in ICU was 8.2 ± 7.6 days. The mean of APACHE II was 18.2 ± 7.2. Lesser values of APACHE II, length of stay and mortality were observed in patients with cardiocirculatory dysfunction. The in-ICU mortality was 33.9%, 6.2% before 48 hours. The standardized mortality ratio (SMR) was 0.988. CONCLUSIONS: The age groups did not determine difference between values of APACHE II. They were related neither to higher mortality rate, nor to higher ICU length of stay. Patients with cardiocirculatory dysfunctions had lesser values of APACHE II, ICU length of stay and in-ICU mortality.
-
Base deficit at intensive care unit admission: an early mortality indicator
Rev Bras Ter Intensiva. 2007;19(4):434-436
Abstract
Base deficit at intensive care unit admission: an early mortality indicator
Rev Bras Ter Intensiva. 2007;19(4):434-436
DOI 10.1590/S0103-507X2007000400005
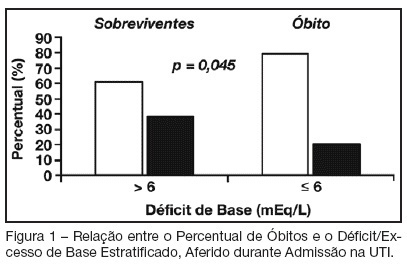
Views0See moreBACKGROUND AND OBJECTIVES: Base deficit is considered an indicator of tissue injury, shock and resuscitation. The objective of this study was to establish an association between base deficit obtained on the admission of patients in intensive care unit (ICU) and their prognosis. METHODS: A retrospective study with analysis of 110 patients admitted consecutively in the ICU, during the period of June to December 2006. RESULTS: There was a predominance of women, with age mean 54.2 ± 18.7 years old. Length of stay in ICU was 6.5 ± 7.4 days and the mean APACHE II score was 21 ± 8.1 points. The standardized mortality ratio was 0.715. Mortality was higher in patients with base deficit > 6 mEq/L (38.9%) than in those with base deficit < 6 mEq/L (20.6%); p < 0.05. Patients with early mortality had lower base deficit (7.75 ± 8.33 mEq/L) than survivors (3.17 ± 5.43 mEq/L); p < 0.05. Patients with permanence in ICU until 7 days and patients that stayed in this unit for more than 7 days had similar base deficit. CONCLUSIONS: Base deficit had been associated with early mortality during ICU internment. Base deficit > 6 mEq/L is a marker of significant mortality.
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis




