Abstract
Rev Bras Ter Intensiva. 2008;20(3):249-253
DOI 10.1590/S0103-507X2008000300007
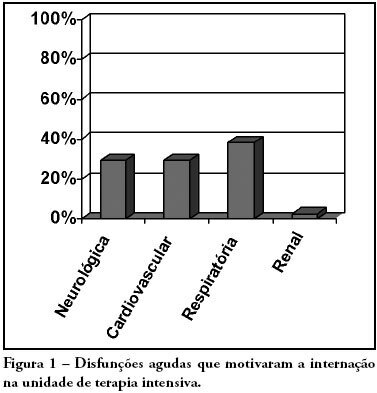
OBJECTIVES: Due to the high incidence in our service, we did object on this study describe the features and outcome of patients with systemic lupus erythematosus (SLE) admitted to the intensive care unit of Walter Cantídio University Hospital METHODS: Patients were restrospectively characterized according to demography parameters, time of diagnosis of SLE, organ dysfunction and laboratorial parameters at admission, supportive therapies during their stay, length of stay in the hospital before admission, length of stay in the unit, readmission to the unit and outcome. We also evaluated Systemic Lupus Erythematosus Disease Activity (SLEDAI) score, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, expected mortality and standardized mortality ratio. RESULTS: From November 2003 to October 2006, 1,052 patients were admitted to the intensive care unit. Fifty patients had SLE and were included in this retrospective study. Of the 50 patients with SLE admitted to the ICU, 88.2% were female. The mean age was 30.3 ± 12.8 years. The median time of diagnosis of SLE was 67 months. The most common organ dysfunctions were renal (70.6%), cardiovascular (61.8%), respiratory (55.9%) and neurological (55.9%). The main reasons for admission to the ICU were respiratory (38.2%), cardiologic (29.4%) and neurological (29.4%) dysfunctions. Among the intensive care therapies, 44.1% of the patients needed blood products, 41.2% vasopressor agents and 35.3% mechanical ventilation, 23.5% dialysis. The mean SLEDAI score was 15.0 ± 12.2. The mean APACHE II score was 19.3 ± 6.8, with a predicted mortality rate of 37.6%. The actual mortality rate in ICU was 29.4%, with 8.8% before 48 hours. The standardized mortality ratio was 0.78. Patients with APACHE II > 18, with more than 3 acute organ involvements, leukopenia (< 4000 cells/mm3) and gastrointestinal or metabolic involvement had higher mortality in the intensive care unit. CONCLUSION: Although the severity of patients at admission to the ICU, demonstrated by APACHE II and the acute dysfunctions, the outcomes of analysed patients sugest susceptibility to the therapy.