Abstract
Rev Bras Ter Intensiva. 2007;19(4):434-436
DOI 10.1590/S0103-507X2007000400005
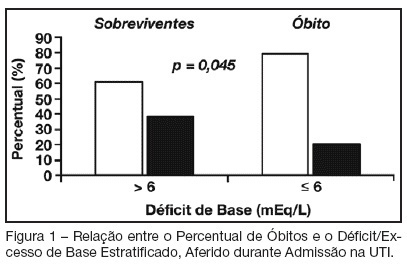
BACKGROUND AND OBJECTIVES: Base deficit is considered an indicator of tissue injury, shock and resuscitation. The objective of this study was to establish an association between base deficit obtained on the admission of patients in intensive care unit (ICU) and their prognosis. METHODS: A retrospective study with analysis of 110 patients admitted consecutively in the ICU, during the period of June to December 2006. RESULTS: There was a predominance of women, with age mean 54.2 ± 18.7 years old. Length of stay in ICU was 6.5 ± 7.4 days and the mean APACHE II score was 21 ± 8.1 points. The standardized mortality ratio was 0.715. Mortality was higher in patients with base deficit > 6 mEq/L (38.9%) than in those with base deficit < 6 mEq/L (20.6%); p < 0.05. Patients with early mortality had lower base deficit (7.75 ± 8.33 mEq/L) than survivors (3.17 ± 5.43 mEq/L); p < 0.05. Patients with permanence in ICU until 7 days and patients that stayed in this unit for more than 7 days had similar base deficit. CONCLUSIONS: Base deficit had been associated with early mortality during ICU internment. Base deficit > 6 mEq/L is a marker of significant mortality.