Abstract
Rev Bras Ter Intensiva. 2013;25(1):32-38
DOI 10.1590/S0103-507X2013000100007
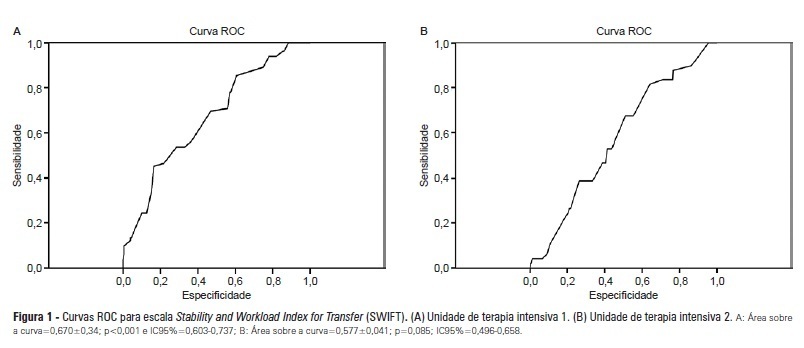
OBJECTIVES: Identify patients at risk for intensive care unit readmission, the reasons for and rates of readmission, and mortality after their stay in the intensive care unit; describe the sensitivity and specificity of the Stability and Workload Index for Transfer scale as a criterion for discharge from the intensive care unit. METHODS: Adult, critical patients from intensive care units from two public hospitals in Porto Alegre, Brazil, comprised the sample. The patients' clinical and demographic characteristics were collected within 24 hours of admission. They were monitored until their final outcome on the intensive care unit (death or discharge) to apply the Stability and Workload Index for Transfer. The deaths during the first intensive care unit admission were disregarded, and we continued monitoring the other patients using the hospitals' electronic systems to identify the discharges, deaths, and readmissions. RESULTS: Readmission rates were 13.7% in intensive care unit 1 (medical-surgical, ICU1) and 9.3% in intensive care unit 2 (trauma and neurosurgery, ICU2). The death rate following discharge was 12.5% from ICU1 and 4.2% from ICU2. There was a statistically significant difference in Stability and Workload Index for Transfer (p<0.05) regarding the ICU1 patients' outcome, which was not found in the ICU2 patients. In ICU1, 46.5% (N=20) of patients were readmitted very early (within 48 hours of discharge). Mortality was high among those readmitted: 69.7% in ICU1 and 48.5% in ICU2. CONCLUSIONS: The Stability and Workload Index for Transfer scale showed greater efficacy in identifying patients more prone to readmission and death following discharge from a medical-surgical intensive care unit. The patients' intensive care unit readmission during the same hospitalization resulted in increased morbidity, mortality, length of stay, and total costs.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
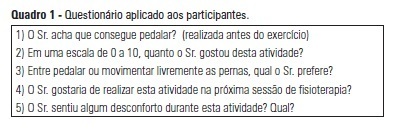
OBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients' satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 - 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):44-48
DOI 10.1590/S0103-507X2013000100009
OBJECTIVE: To evaluate the effectiveness of a tongue cleaner in the removal of tongue biofilm in mechanically ventilated patients. METHODS: Tongue biofilm and tracheal secretion samples were collected from a total of 50 patients: 27 in the study group (SG) who were intubated or tracheostomized under assisted ventilation and treated with the tongue cleaner and 23 in the control group (CG) who did not undergo tongue cleaning. Oral and tracheal secretion cultures of the SG (initially and after 5 days) and the CG (at a single time-point) were performed to evaluate the changes in bacterial flora. RESULTS: The median age of the SG patients was 77 years (45-99 years), and that of the CG patients was 79 years (21-94 years). The length of hospital stay ranged from 17-1,370 days for the SG with a median stay of 425 days and from 4-240 days for the CG with a median stay of 120 days. No significant differences were found when the dental plaque indexes were compared between the SG and the CG. There was no correlation between the index and the length of hospital stay. The same bacterial flora was found in the dental plaque of 9 of the 27 SG patients before and after the tongue scraper was used for 5 days compared with the CG (p=0.683). Overall, 7 of the 27 SG patients had positive bacterial cultures for the same strains in both tongue biofilm and tracheal secretions compared with the CG (p=0.003). Significant similarities in strain resistance and susceptibility of the assessed microorganisms were observed between oral and tracheal microflora in 6/23 cases in the CG (p=0.006). CONCLUSION: The use of a tongue cleaner is effective at reducing tongue biofilm in patients on mechanical ventilation and facilitates oral hygiene interventions performed by caregivers.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):6-11
DOI 10.1590/S0103-507X2013000100003
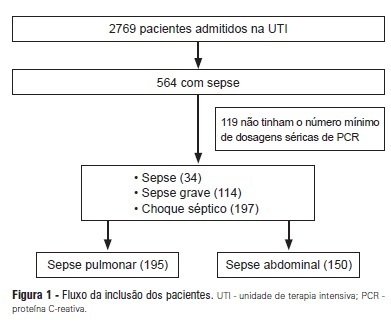
OBJECTIVES: To evaluate the C-reactive protein serum levels in patients with pulmonary and abdominal sepsis during the first five days of sepsis progression. METHODS: The present investigation was a retrospective cohort study conducted at the university hospital with 345 patients who were admitted to the intensive care unit and diagnosed with sepsis of pulmonary or abdominal origin. Serum C-reactive protein concentrations were measured by the turbidimetric immunoassay. For analysis of C-reactive protein, day 1 was defined as the day on which the patient was clinically diagnosed with sepsis. RESULTS: Thirty-four patients with sepsis (9.8%), 114 patients with severe sepsis (33.0%), and 197 patients with septic shock (57.2%) were evaluated. The age of the patients was 56.4±19.8 years. The serum C-reactive protein concentrations were higher on the day of sepsis diagnosis in the group with abdominal infection compared with the group with pulmonary sepsis (17.8±10.1 mg/dL versus 14.9±11.1 mg/dL, p=0.025) and remained significantly higher during the first five days of sepsis progression. CONCLUSION: The serum C-reactive protein concentrations were significantly higher in the patients with abdominal sepsis compared with the patients with pulmonary sepsis during the first five days of sepsis progression.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):12-16
DOI 10.1590/S0103-507X2013000100004
OBJECTIVE: This study aimed to evaluate the outcomes for patients with lung cancer admitted to intensive care units and assess their clinical and demographic profiles. METHODS: Retrospective, analytical, observational study, wherein the outcomes for patients diagnosed with lung cancer admitted to the intensive care unit of university hospital from January 2010 until February 2011 were evaluated. RESULTS: Thirty-four patients' medical records were included. Twenty-six (76.5%) patients received some type of ventilatory support, of whom 21 (61.8%) used invasive mechanical ventilation and 11 (32.4%) used noninvasive ventilation at some point during their stay at the intensive care unit. Regarding mortality, 12 (35.3%) patients died during hospitalization at the intensive care unit, totaling 15 (44.1%) deaths during the entire hospitalization period; 19 (55.9%) patients were discharged from the hospital. The analysis of the variables showed that the patients who died had remained on invasive mechanical ventilation for a longer period 5.0 (0.25 to 15.0) days than the survivors (1.0 (0 to 1.0) days) (p=0.033) and underwent dialysis during their stay at the intensive care unit (p=0.014). CONCLUSIONS: The mortality of patients with lung cancer admitted to the intensive care unit is associated with the time spent on invasive mechanical ventilation and the need for dialysis.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):17-24
DOI 10.1590/S0103-507X2013000100005
OBJECTIVE: Evaluate the compliance of septic patients' nutritional management with enteral nutrition guidelines for critically ill patients. METHODS: Prospective cohort study with 92 septic patients, age ≥18 years, hospitalized in an intensive care unit, under enteral nutrition, evaluated according to enteral nutrition guidelines for critically ill patients, compliance with caloric and protein goals, and reasons for not starting enteral nutrition early or for discontinuing it. Prognostic scores, length of intensive care unit stay, clinical progression, and nutritional status were also analyzed. RESULTS: The patients had a mean age of 63.4±15.1 years, were predominantly male, were diagnosed predominantly with septic shock (56.5%), had a mean intensive care unit stay of 11 (7.2 to 18.0) days, had 8.2±4.2 SOFA and 24.1±9.6 APACHE II scores, and had 39.1% mortality. Enteral nutrition was initiated early in 63% of patients. Approximately 50% met the caloric and protein goals on the third day of intensive care unit stay, a percentage that decreased to 30% at day 7. Reasons for the late start of enteral nutrition included gastrointestinal tract complications (35.3%) and hemodynamic instability (32.3%). Clinical procedures were the most frequent reason to discontinue enteral nutrition (44.1%). There was no association between compliance with the guidelines and nutritional status, length of intensive care unit stay, severity, or progression. CONCLUSION: Although the number of septic patients under early enteral nutrition was significant, caloric and protein goals at day 3 of intensive care unit stay were met by only half of them, a percentage that decreased at day 7.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):386-392
DOI 10.1590/S0103-507X2012000400016
OBJECTIVE: To analyze the process of care provided to premature infants in a neonatal intensive care unit and the factors associated with their mortality. METHODS: Cross-sectional retrospective study of premature infants in an intensive care unit between 2008 and 2010. The characteristics of the mothers and premature infants were described, and a bivariate analysis was performed on the following characteristics: the study period and the "death" outcome (hospital, neonatal and early) using Pearson's chi-square test, Fisher's exact test or a chi-square test for linear trends. Bivariate and multivariable logistic regression analyses were performed using a stepwise backward logistic regression method between the variables with p<0.20 and the "death" outcome. A p value <0.05 was considered to be significant. RESULTS: In total, 293 preterm infants were studied. Increased access to complementary tests (transfontanellar ultrasound and Doppler echocardiogram) and breastfeeding rates were indicators of improving care. Mortality was concentrated in the neonatal period, especially in the early neonatal period, and was associated with extreme prematurity, small size for gestational age and an Apgar score <7 at 5 minutes after birth. The late-onset sepsis was also associated with a greater chance of neonatal death, and antenatal corticosteroids were protective against neonatal and early deaths. CONCLUSIONS: Although these results are comparable to previous findings regarding mortality among premature infants in Brazil, the study emphasizes the need to implement strategies that promote breastfeeding and reduce neonatal mortality and its early component.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):341-346
DOI 10.1590/S0103-507X2012000400008
OBJECTIVE: To examine the reliability of the SF-36 general health questionnaire when used to evaluate the health status of critically ill patients before admission to intensive care and to measure their health-related quality of life prior to admission and its relation to severity of illness and length of stay in the intensive care unit. METHODS: Prospective cohort study conducted in the intensive care unit of a public teaching hospital. Over three months, communicative and oriented patients were interviewed within the first 72 hours of intensive care unit admission; 91 individuals participated. The APACHE II score was used to assess severity of illness, and the SF-36 questionnaire was used to measure health-related quality of life. RESULTS: The reliability of SF-36 was verified in all dimensions using Cronbach's alpha coefficient. In six dimensions of eight domains the value exceeded 0.70. The average SF-36 scores of the health-related quality of life dimensions for the patients before admission to intensive care unit were 57.8 for physical functioning, 32.4 for role-physical, 53.0 for bodily pain, 63.2 for general health, 50.6 for vitality, 56.2 for social functioning, 54.6 for role-emotional and 60.3 for mental health. The correlations between severity of illness and length of stay and the health-related quality of life scores were very low, ranging from -0.152 to 0.175 and -0.158 to 0.152, respectively, which were not statistically significant. CONCLUSION: In the sample studied, the SF-36 demonstrated good reliability when used to measure health-related quality of life in critically ill patients before admission to the intensive care unit. The worst score was role-physical and the best was general health. Health-related quality of life of patients before admission was not correlated with severity of illness or length of stay in the intensive care unit.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)