Abstract
Rev Bras Ter Intensiva. 2012;24(4):334-340
DOI 10.1590/S0103-507X2012000400007
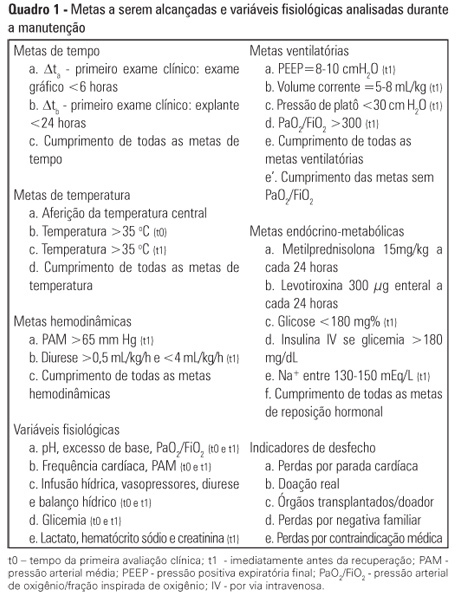
OBJECTIVE: To assess the effect of the application of a managed protocol for the maintenance care of deceased potential multiple organ donors at two hospitals. METHODS: A before (Phase 1)/after (Phase 2) study conducted at two general hospitals, which included consecutively potential donors admitted to two intensive care units. In Phase 1 (16 months), the data were collected retrospectively, and the maintenance care measures of the potential donors were instituted by the intensivists. In Phase 2 (12 months), the data collection was prospective, and a managed protocol was used for maintenance care. The two phases were compared in terms of their demographic variables, physiological variables at diagnosis of brain death and the end of the process, time to performance of brain death confirmatory test and end of the process, adherence to bundles of maintenance care essential measures, losses due to cardiac arrest, family refusal, contraindications, and the conversion rate of potential into actual donors. Student's t- and chi-square tests were used, and p-value < 0.05 was considered to be significant. RESULTS: A total of 42 potential donors were identified (18 in Phase 1 and 24 in Phase 2). The time interval between the first clinical assessment and the recovery decreased in Phase 2 (Phase 1: 35.0±15.5 hours versus Phase 2: 24.6±6.2 hours; p = 0.023). Adherence increased to 10 out of the 19 essential items of maintenance care, and losses due to cardiac arrest also decreased in Phase 2 (Phase 1: 27.8 versus 0% in Phase 2; p = 0.006), while the convertion rate increased (Phase 1: 44.4 versus 75% in Phase 2; p = 0.044). The losses due to family refusal and medical contraindication did not vary. CONCLUSION: The adoption of a managed protocol focused on the application of essential measures for the care of potential deceased donors might reduce the loss of potential donors due to cardiac arrest.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):381-385
DOI 10.1590/S0103-507X2012000400015
OBJECTIVE: The aim of this study was to describe the incidence and epidemiology of nosocomial infection in newborns who were admitted to a neonatal intensive care unit in a hospital in south Santa Catarina, Brazil. METHODS: A prospective cohort study was conducted for 1 year among 239 neonates who remained as in-patients 48 hours after admission. The criteria that were used to diagnose infection were in accordance with the Centers for Disease Control and Prevention and the National Health Surveillance Agency. RESULTS: The incidence of nosocomial infection was 45.8%. The primary reasons for admission were primary bloodstream infection (80.7%) and pneumonia (6.7%). Coagulase-negative Staphylococcus was the most commonly identified agent in the blood cultures and in the hospital unit. Prematurity was the most prevalent reason for admission. The general mortality rate was 12.1%, and mortality from nosocomial infection was 33.8%. CONCLUSIONS: The incidence of nosocomial infection in the hospital unit was higher than rates that have been reported in other national studies. The major types of nosocomial infection were primary bloodstream infection and pneumonia.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):375-380
DOI 10.1590/S0103-507X2012000400014
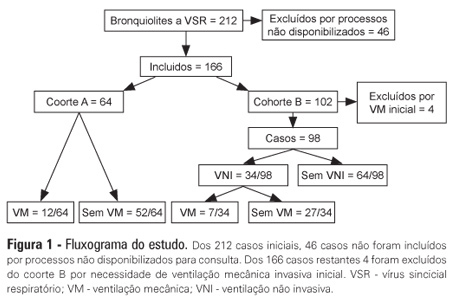
OBJECTIVES: The present study focused on respiratory syncytial virus bronchiolitis with respiratory failure. The aim of the study was to determine whether noninvasive ventilation reduces the need for endotracheal intubation or slows the clinical progression of acute respiratory syncytial virus bronchiolitis by reducing the incidence of infectious complications. METHODS: The present study was a retrospective cohort study. Cohort A was comprised of children who were admitted to the pediatric intensive and special care unit from 2003-2005 before starting noninvasive ventilation; cohort B was comprised of children who were admitted to the pediatric intensive and special care unit from 2006-2008 after starting noninvasive ventilation. With the exception of noninvasive ventilation, the therapeutic support was the same for the two groups. All children who were diagnosed with respiratory syncytial virus bronchiolitis and respiratory failure between November 2003 and March 2008 were included in the cohort. Demographic, clinical and blood gas variables were analyzed. RESULTS: A total of 162 children were included; 75% of the subjects were less than 3 months old. Group A included 64 children, and group B included 98 children. In group B, 34 of the children required noninvasive ventilation. The distributions of the variables age, preterm birth, congenital heart disease, cerebral palsy and chronic lung disease were similar between the two groups. On admission, the data for blood gas analysis and the number of apneas were not significantly different between the groups. In group B, fewer children required invasive ventilation (group A: 12/64 versus group B: 7/98; p=0.02), and there was a reduction in the number of cases of bacterial pneumonia (group A: 19/64 versus group B: 12/98; p=0.008). There was no record of mortality in either of the groups. CONCLUSION: By comparing children with the same disease both before and after noninvasive ventilation was used for ventilation support, we verified a reduction in infectious complications and cases requiring intubation.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):369-374
DOI 10.1590/S0103-507X2012000400013
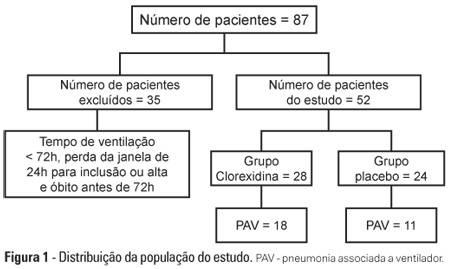
OBJECTIVE: To evaluate the effects of oral chlorhexidine hygiene with toothbrushing on the rate of ventilator-associated pneumonia in a mixed population of critically ill patients under prolonged mechanical ventilation. METHODS: Prospective, randomized, and placebo-controlled pilot study. Patients who were receiving mechanical ventilation, had been admitted less than 24 hours prior, and were anticipated to require mechanical ventilation for more than 72 hours were included in the study. The patients were randomly divided into one of the following groups: chlorhexidine hygiene with toothbrushing or a placebo group (gel with the same color and consistency and toothbrushing). RESULTS: The planned interim analysis was conducted using 52 patients, and the study was terminated prematurely. In total, 28 patients were included in the chlorhexidine / toothbrushing group, and 24 patients were included in the placebo group. Ventilator-associated pneumonia occurred in 45.8% of the placebo group and in 64.3% of the chlorhexidine hygiene with toothbrushing group (RR=1.4; 95% CI=0.83-2.34; p=0.29). CONCLUSION: Because the study was terminated due to futility, it was not possible to evaluate the impact of oral hygiene using 2% chlorhexidine and toothbrushing on the incidence of ventilator-associated pneumonia in this heterogeneous population of critical patients receiving long-term mechanical ventilation, and no beneficial effect was observed for this intervention.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):362-368
DOI 10.1590/S0103-507X2012000400012
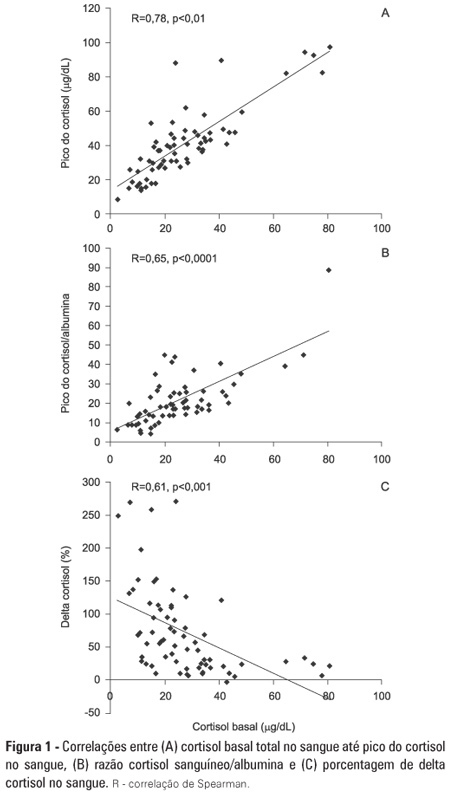
OBJECTIVE: To evaluate if cortisol responses to 250 µg of intravenously administered adrenocorticotropic hormone are related to disease severity and, hence, mortality. METHODS: This is a retrospective study in a medical-surgical intensive care unit of a university hospital. We studied 69 consecutive patients with septic shock over a 1-yr period; these patients underwent a short 250-µg adrenocorticotropic hormone test because they exhibited >6 hours of progressive hemodynamic instability requiring repeated fluid challenges and vasopressor treatment to maintain blood pressure. The test was performed by intravenously injecting 250 µg of synthetic adrenocorticotropic hormone and measuring cortisol immediately before injection, 30 minutes post-injection and 60 minutes post-injection. RESULTS: The mean APACHE II score was 22±7. The intensive care unit mortality rate at day 28 was 55%. Median baseline cortisol levels (19 [11-27] µg/dL versus 24 [18-34] µg/dL, p=0.047) and median baseline cortisol/albumin ratios (7.6 [4.6-12.3] versus 13.9 [8.8-18.5]; p=0.01) were lower in survivors than in non-survivors. Responders and non-responders had similar baseline clinical data and outcomes. The variables that were significantly correlated with outcome based on the area under the ROC curves (AUC) were APACHE II (AUC=0.67 [0.535 to 0.781]), baseline cortisol (µg/dl) (AUC=0.662 [0.536 to 0.773], peak cortisol (µg/dl) (AUC=0.642 [0.515 to 0.755]) and baseline cortisol/albumin (AUC=0.75 [0.621 to 0.849]). CONCLUSIONS: Increased basal cortisol is associated with mortality and disease severity. Cortisol responses upon adrenocorticotropic hormone stimulation were not related to outcome. The cortisol/albumin ratio does not predict unfavorable outcomes better than total cortisol levels or help to improve the accuracy of the adrenocorticotropic hormone test.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):352-356
DOI 10.1590/S0103-507X2012000400010
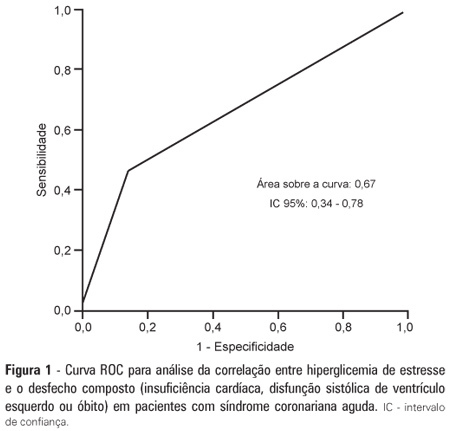
OBJECTIVE: To demonstrate the prevalence of stress hyperglycemia in a cohort of patients with acute coronary syndrome and to determine the correlation of stress hyperglycemia with death, heart failure and/or left ventricular systolic dysfunction during the intrahospital phase. METHODS: A prospective initial cohort study of hospitalized patients with acute coronary syndrome with or without ST segment elevation. The groups were compared to demonstrate the correlation between stress hyperglycemia and cardiovascular events. The chi-square test or Fisher's exact test and student's t-test were used to compare the groups with and without stress hyperglycemia. The variables with p<0.20 in the univariate analysis were submitted to logistic regression. RESULTS: In total, 363 patients with an average age of 12.45 ± 62.06 were studied. There was a predominance of males (64.2%). In total, 96 patients (26.4%) presented with stress hyperglycemia. There were no differences between the groups with or without stress hyperglycemia. The area under the ROC curve was 0.67 for the relationship between stress hyperglycemia and the composite outcome heart failure, left ventricular systolic dysfunction or death at the end of the hospital admission. The ROC curve proved that stress hyperglycemia was the predictor of the composite outcome (death, heart failure and/or ventricular dysfunction). The multivariate analysis did not indicate age, stress hyperglycemia or admission heart rate as risk factors. CONCLUSION: Stress hyperglycemia was common in the studied sample. In the univariate analysis, the presence of stress hyperglycemia was associated with such events as death, heart failure and/or intrahospital ventricular dysfunction in patients with acute coronary syndrome.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):357-361
DOI 10.1590/S0103-507X2012000400011
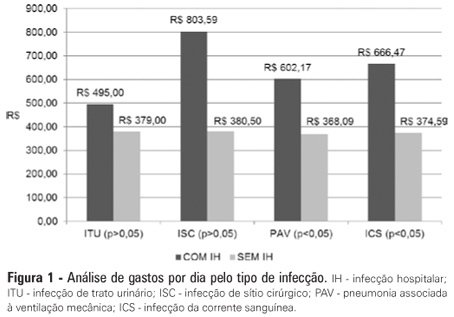
OBJECTIVE: Infections in intensive care units are often associated with a high morbidity and mortality in addition to high costs. An analysis of these aspects can assist in optimizing the allocation of relevant financial resources. METHODS: This retrospective study analyzed the hospital administration and quality in intensive care medical databases [Sistema de Gestão Hospitalar (SGH)] and RM Janus®. A cost analysis was performed by evaluating the medical products and materials used in direct medical care. The costs are reported in the Brazilian national currency (Real). The cost and length of stay analyses were performed for all the costs studied. The median was used to determine the costs involved. Costs were also adjusted by the patients' length of stay in the intensive care unit. RESULTS: In total, 974 individuals were analyzed, of which 51% were male, and the mean age was 57±18.24 years. There were 87 patients (8.9%) identified who had nosocomial infections associated with the intensive care unit. The median cost per admission and the length of stay for all the patients sampled were R$1.257,53 and 3 days, respectively. Compared to the patients without an infection, the patients with an infection had longer hospital stays (15 [11-25] versus 3 [2-6] days, p<0.01), increased costs per patient in the intensive care unit (median R$9.763,78 [5445.64 - 18,007.90] versus R$1.093,94 [416.14 - 2755.90], p<0.01) and increased costs per day of hospitalization in the intensive care unit (R$618,00 [407.81 - 838.69] versus R$359,00 [174.59 - 719.12], p<0.01). CONCLUSION: Nosocomial infections associated with the intensive care unit were determinants of increased costs and longer hospital stays. However, the study design did not allow us to evaluate specific aspects of cause and effect.