Abstract
Rev Bras Ter Intensiva. 2013;25(2):87-92
DOI 10.5935/0103-507X.20130018
OBJECTIVES: To evaluate the incidence of constipation in critical patients on enteral nutrition in a hospital intensive care unit and to correlate this incidence with the variables found for critical patients. METHODS: The present investigation was a retrospective analytical study conducted in the intensive care unit of Hospital Regional da Asa Norte (DF) via the analysis of medical records of patients admitted during the period from January to December 2011. Data on the incidence of constipation and enteral nutritional support, gastrointestinal changes, stool frequency, ventilatory support, and outcomes were collected and analyzed. RESULTS: The initial sample consisted of 127 patients admitted to the unit during the period from January to December 2011. Eighty-four patients were excluded, and the final sample consisted of 43 patients. The incidence of constipation, defined as no bowel movement during the first 4 days of hospitalization, was 72% (n=31). The patients were divided into a control group and a constipated group. The group of constipated patients reached the caloric target, on average, at 6.5 days, and the control group reached the caloric target in 5.6 days (p=0.51). Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization. There was an association between evacuation during hospitalization and a longer duration of hospitalization for a subgroup of patients who did not evacuate during the entire period (p=0.009). CONCLUSION: The incidence of constipation in the unit studied was 72%. Only the absence of evacuation during hospitalization was associated with longer hospital stays. Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization.
Abstract
Rev Bras Ter Intensiva. 2009;21(3):324-331
DOI 10.1590/S0103-507X2009000300014
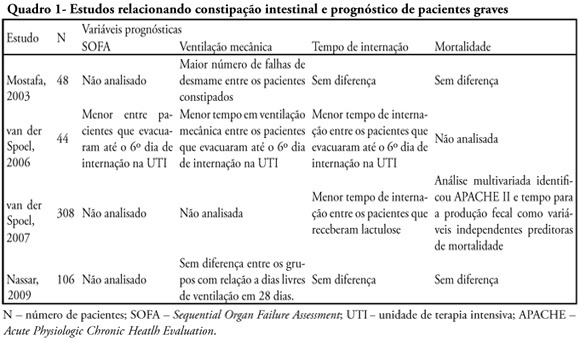
Constipation is a common complication identified among critically ill patients. Its incidence is highly variable due to lack of definition of such patients. Besides the already known consequences of constipation, in recent years it was observed that this complication may also be related to worse prognosis of critically ill patients. This review endeavors to describe the main available scientific evidence showing that constipation is a prognostic marker and a clinical representation of intestinal dysfunction, in addition to eventually interfering in the prognosis with treatment. Ogilvie syndrome, a major cause of morbidity and mortality in intensive care units was also reviewed. Considering the above cases it was concluded that more attention to this disorder is required in intensive care units as well as development of protocols for diagnosis and management of critically ill patients.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)