Abstract
Rev Bras Ter Intensiva. 2009;21(1):72-79
DOI 10.1590/S0103-507X2009000100011
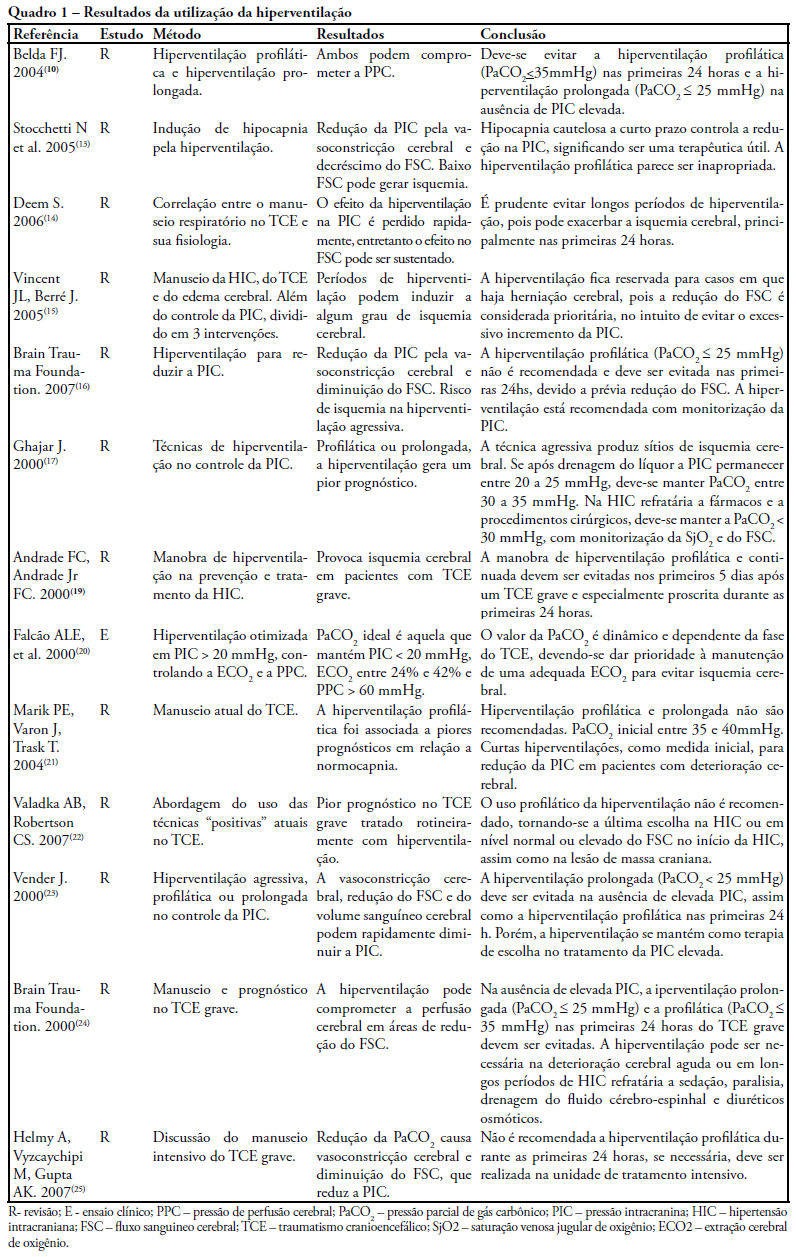
The study intended to make a critical review on use of pulmonary hyperventilation maneuvers and the different positive end-expiratory pressures applied to traumatic brain injury patients. As a reference were used publications in English, Spanish and Portuguese, contained in the following databases: MedLine, SciELO and LILACS, from 2000 to 2007, we included all studies about the use of pulmonary hyperventilation maneuvers and the different positive end-expiratory levels used for adult patients with brain injury at acute or chronic stage. Thirty one trials were selected, 13 about pulmonary hyperventilation, as prophylaxis, prolonged or optimized and 9 shows the levels of positive end-expiratory pressures used, ranging from 0 to 15 cmH2O. The prophylactic hyperventilation maneuver in the first 24 hours can lead to an increase of cerebral ischemia; the prolonged hyperventilation must be avoided if intracranial pressure did not increase; however optimized hyperventilation seems to be the most promising technique for control of the intracranial pressure and cerebral perfusion pressure; the rise of the positive end-expiratory pressure, up to 15cmH2O, can be applied in a conscientious form aiming to increase arterial oxygen saturation in lung injury.
Abstract
Rev Bras Ter Intensiva. 2008;20(4):339-343
DOI 10.1590/S0103-507X2008000400004
OBJECTIVE: After brain injury intracranial hypertension is the major cause of mortality, in addition to the possibility of functional, behavioral and cognitive sequels. Scarcity of studies on the effects of respiratory physiotherapy on these patients may lead to contradictory performances. This study aimed to assess the effects of customary respiratory physiotherapy maneuvers on intracranial and cerebral perfusion pressures in patients with severe brain injury. METHODS: Clinical, prospective trial with patients with severe traumatic brain injury, mechanically ventilated and with a continued measurement of intracranial pressure. The effects of manual vibrocompression maneuvers and intratracheal aspiration with or without saline infusion on the measurements of intracranial and cerebral perfusion pressures, between the first and third day after cerebral injury were evaluated. RESULTS: Data were collected from 11 patients, 41 years of age (median) and APACHE II of 19.5 ± 5. The manual vibrocompression maneuver did not cause an increase of intracranial pressure on any of the days assessed. Intracranial pressure significantly increased after intratracheal aspiration maneuvers in relation to the basal measurement (day1, 9.5 ± 0.9 mm Hg vs 18.0 ± 3.2 mm Hg; day 2, 10.6 ± 1.7 mm Hg vs 21.4 ± 3.8 mm Hg; day 3, 14.4 ± 1.0 vs 24.9 ± 2.7 mm Hg; p<0.05 for all). However, these elevations were transient (about 27 seconds) and accompanied by compensatory increases of the cerebral perfusion pressure. CONCLUSION: The manual vibrocompression maneuver did not increase intracranial pressure or cerebral perfusion pressure in patients with severe brain injury. Intratracheal aspiration induced a significant and transient increase of the intracranial and cerebral perfusion pressures.
