Abstract
Crit Care Sci. 2023;35(3):243-255
DOI 10.5935/2965-2774.20230136-pt
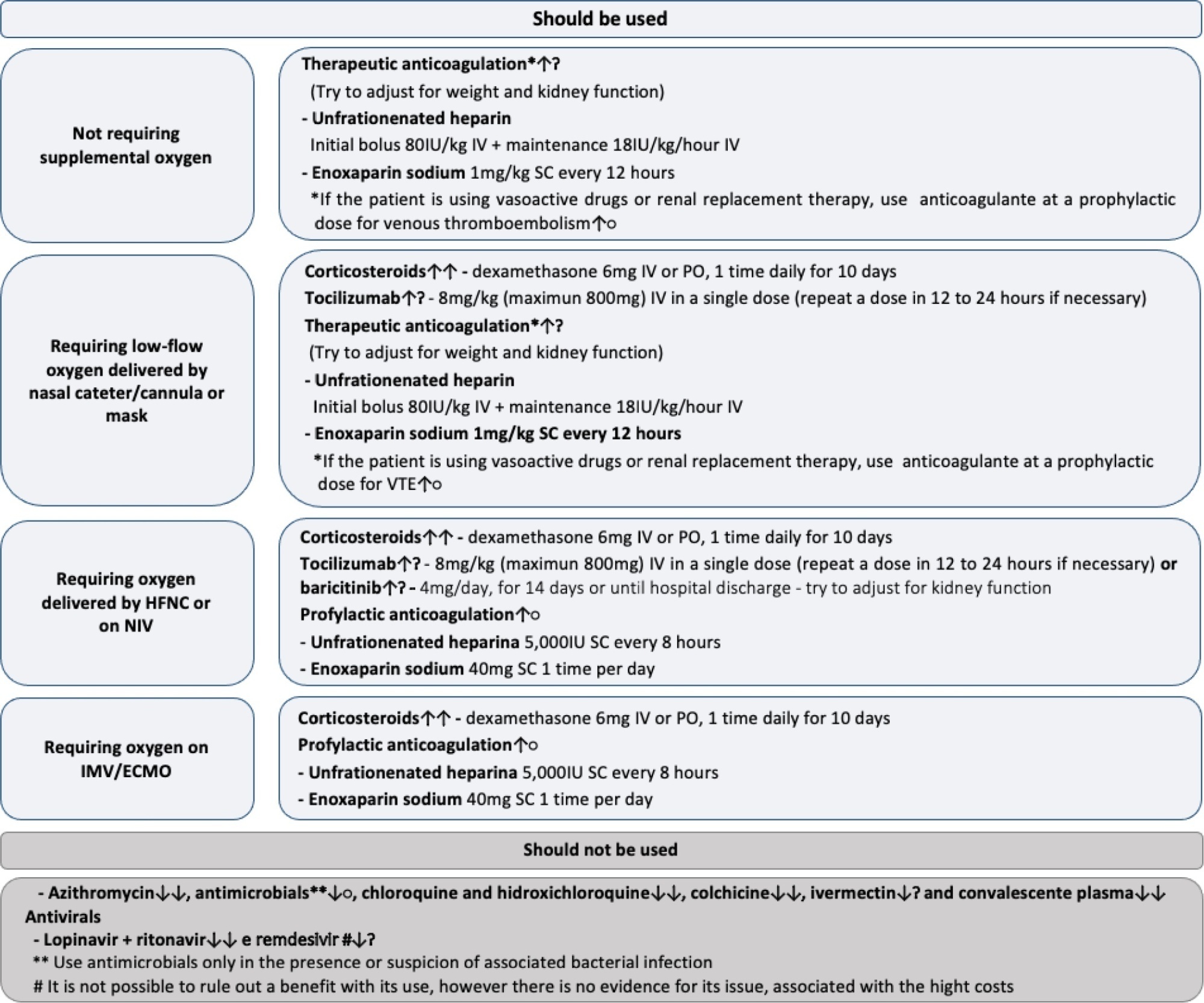
To update the recommendations to support decisions regarding the pharmacological treatment of patients hospitalized with COVID-19 in Brazil.
Experts, including representatives of the Ministry of Health and methodologists, created this guideline. The method used for the rapid development of guidelines was based on the adoption and/or adaptation of existing international guidelines (GRADE ADOLOPMENT) and supported by the e-COVID-19 RecMap platform. The quality of the evidence and the preparation of the recommendations followed the GRADE method.
Twenty-one recommendations were generated, including strong recommendations for the use of corticosteroids in patients using supplemental oxygen and conditional recommendations for the use of tocilizumab and baricitinib for patients on supplemental oxygen or on noninvasive ventilation and anticoagulants to prevent thromboembolism. Due to suspension of use authorization, it was not possible to make recommendations regarding the use of casirivimab + imdevimab. Strong recommendations against the use of azithromycin in patients without suspected bacterial infection, hydroxychloroquine, convalescent plasma, colchicine, and lopinavir + ritonavir and conditional recommendations against the use of ivermectin and remdesivir were made.
New recommendations for the treatment of hospitalized patients with COVID-19 were generated, such as those for tocilizumab and baricitinib. Corticosteroids and prophylaxis for thromboembolism are still recommended, the latter with conditional recommendation. Several drugs were considered ineffective and should not be used to provide the best treatment according to the principles of evidence-based medicine and to promote resource economy.
Abstract
Crit Care Sci. 2023;35(3):302-310
DOI 10.5935/2965-2774.20230141-pt
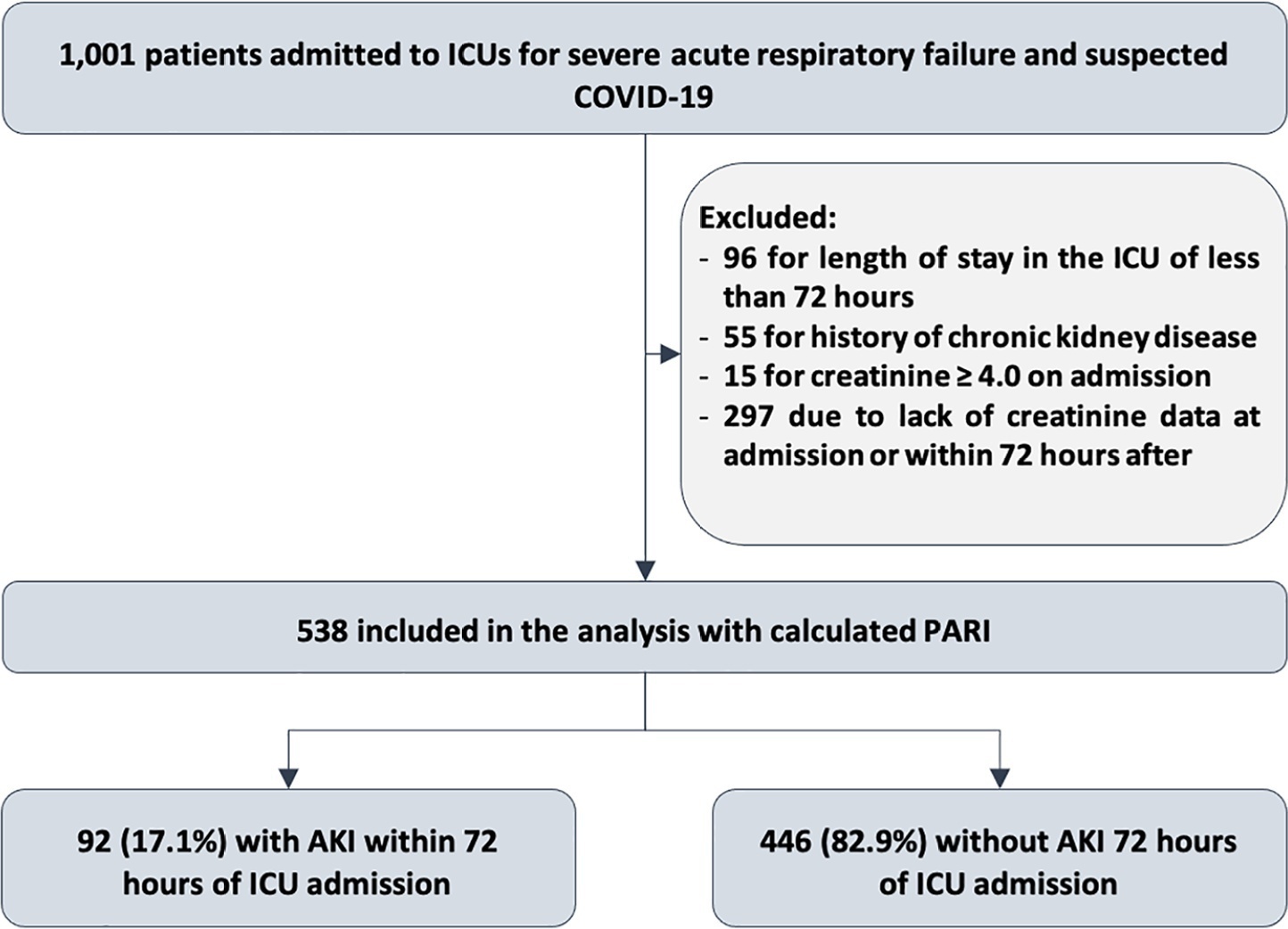
To evaluate the accuracy of the persistent AKI risk index (PARI) in predicting acute kidney injury within 72 hours after admission to the intensive care unit, persistent acute kidney injury, renal replacement therapy, and death within 7 days in patients hospitalized due to acute respiratory failure.
This study was done in a cohort of diagnoses of consecutive adult patients admitted to the intensive care unit of eight hospitals in Curitiba, Brazil, between March and September 2020 due to acute respiratory failure secondary to suspected COVID-19. The COVID-19 diagnosis was confirmed or refuted by RT-PCR for the detection of SARS-CoV-2. The ability of PARI to predict acute kidney injury at 72 hours, persistent acute kidney injury, renal replacement therapy, and death within 7 days was analyzed by ROC curves in comparison to delta creatinine, SOFA, and APACHE II.
Of the 1,001 patients in the cohort, 538 were included in the analysis. The mean age was 62 ± 17 years, 54.8% were men, and the median APACHE II score was 12. At admission, the median SOFA score was 3, and 83.3% had no renal dysfunction. After admission to the intensive care unit, 17.1% had acute kidney injury within 72 hours, and through 7 days, 19.5% had persistent acute kidney injury, 5% underwent renal replacement therapy, and 17.1% died. The PARI had an area under the ROC curve of 0.75 (0.696 - 0.807) for the prediction of acute kidney injury at 72 hours, 0.71 (0.613 - 0.807) for renal replacement therapy, and 0.64 (0.565 - 0.710) for death.
The PARI has acceptable accuracy in predicting acute kidney injury within 72 hours and renal replacement therapy within 7 days of admission to the intensive care unit, but it is not significantly better than the other scores.
Abstract
Crit Care Sci. 2023;35(2):156-162
DOI 10.5935/2965-2774.20230343-pt
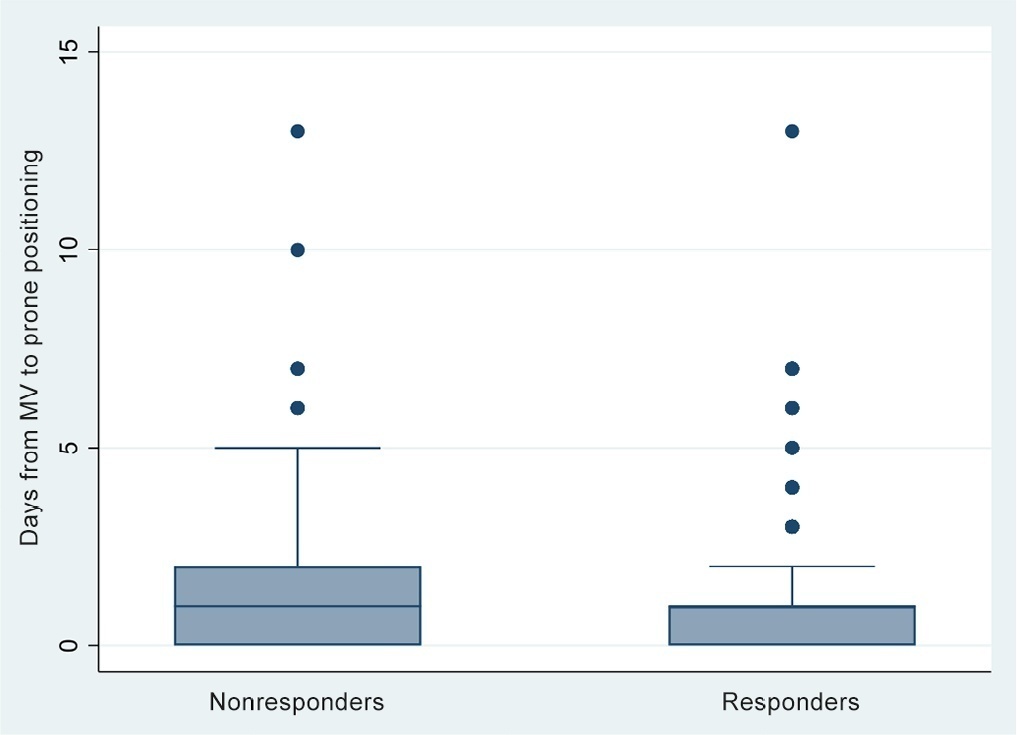
To identify risk factors for nonresponse to prone positioning in mechanically ventilated patients with COVID-19-associated severe acute respiratory distress syndrome and refractory hypoxemia in a tertiary care hospital in Colombia.
Observational study based on a retrospective cohort of mechanically ventilated patients with severe acute respiratory distress syndrome due to SARS-CoV-2 who underwent prone positioning due to refractory hypoxemia. The study considered an improvement ≥ 20% in the PaO2/FiO2 ratio after the first cycle of 16 hours in the prone position to be a ‘response’. Nonresponding patients were considered cases, and responding patients were controls. We controlled for clinical, laboratory, and radiological variables.
A total of 724 patients were included (58.67 ± 12.37 years, 67.7% males). Of those, 21.9% were nonresponders. Mortality was 54.1% for nonresponders and 31.3% for responders (p < 0.001). Variables associated with nonresponse were time from the start of mechanical ventilation to pronation (OR 1.23; 95%CI 1.10 - 1.41); preintubation PaO2/FiO2 ratio (OR 0.62; 95%CI 0.40 - 0.96); preprone PaO2/FiO2 ratio (OR 1.88. 95%CI 1.22 - 2.94); and radiologic multilobe consolidation (OR 2.12; 95%CI 1.33 - 3.33) or mixed pattern (OR 1.72; 95%CI 1.07 - 2.85) compared with a ground-glass pattern.
This study identified factors associated with nonresponse to prone positioning in patients with refractory hypoxemia and acute respiratory distress syndrome due to SARS-CoV-2 receiving mechanical ventilation. Recognizing such factors helps identify candidates for other rescue strategies, including more extensive prone positioning or extracorporeal membrane oxygenation. Further studies are needed to assess the consistency of these findings in populations with acute respiratory distress syndrome of other etiologies.
Abstract
Crit Care Sci. 2023;35(2):163-167
DOI 10.5935/2965-2774.20230009-pt
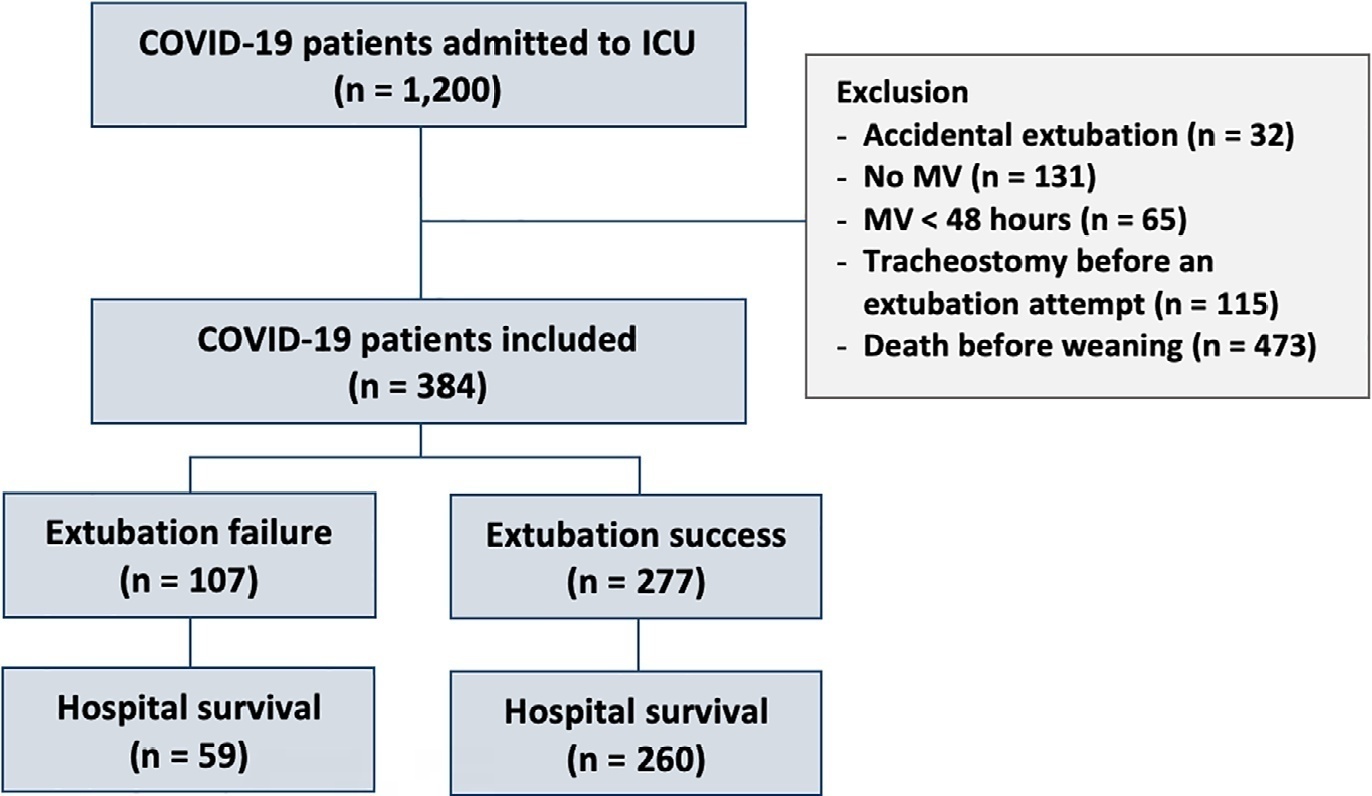
To assess the outcome of extubation in COVID-19 patients and the use of noninvasive ventilation in the weaning process.
This retrospective, observational, single-center study was conducted in COVID-19 patients aged 18 years or older who were admitted to an intensive care unit between April 2020 and December 2021, placed under mechanical ventilation for more than 48 hours and progressed to weaning. Early extubation was defined as extubation without a spontaneous breathing trial and immediate use of noninvasive ventilation after extubation. In patients who underwent a spontaneous breathing trial, noninvasive ventilation could be used as prophylactic ventilatory assistance when started immediately after extubation (prophylactic noninvasive ventilation) or as rescue therapy in cases of postextubation respiratory failure (therapeutic noninvasive ventilation). The primary outcome was extubation failure during the intensive care unit stay.
Three hundred eighty-four extubated patients were included. Extubation failure was observed in 107 (27.9%) patients. Forty-seven (12.2%) patients received prophylactic noninvasive ventilation. In 26 (6.8%) patients, early extubation was performed with immediate use of noninvasive ventilation. Noninvasive ventilation for the management of postextubation respiratory failure was administered to 64 (16.7%) patients.
We found that COVID-19 patients had a high rate of extubation failure. Despite the high risk of extubation failure, we observed low use of prophylactic noninvasive ventilation in these patients.
Abstract
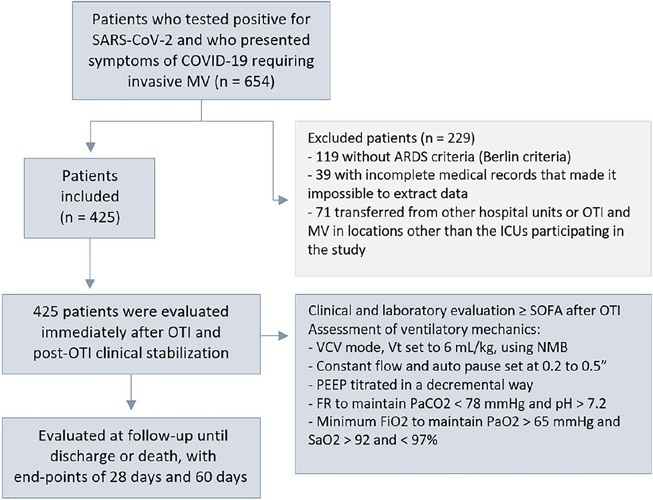
Crit Care Sci. 2023;35(1):19-30
DOI 10.5935/2965-2774.20230203-pt
To evaluate the factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19.
This was a retrospective, multicenter cohort study that included 425 mechanically ventilated adult patients with COVID-19 admitted to 4 intensive care units. Clinical data comprising the SOFA score, laboratory data and mechanical characteristics of the respiratory system were collected in a standardized way immediately after the start of invasive mechanical ventilation. The risk factors for death were analyzed using Cox regression to estimate the risk ratios and their respective 95%CIs.
Body mass index (RR 1.17; 95%CI 1.11 - 1.20; p < 0.001), SOFA score (RR 1.39; 95%CI 1.31 - 1.49; p < 0.001) and driving pressure (RR 1.24; 95%CI 1.21 - 1.29; p < 0.001) were considered independent factors associated with mortality in mechanically ventilated patients with acute respiratory distress syndrome due to COVID-19. Respiratory system compliance (RR 0.92; 95%CI 0.90 - 0.93; p < 0.001) was associated with lower mortality. The comparative analysis of the survival curves indicated that patients with respiratory system compliance (< 30mL/cmH2O), a higher SOFA score (> 5 points) and higher driving pressure (> 14cmH2O) were more significantly associated with the outcome of death at 28 days and 60 days.
Patients with a body mass index > 32kg/m2, respiratory system compliance < 30mL/cmH2O, driving pressure > 14cmH2O and SOFA score > 5.8 immediately after the initiation of invasive ventilatory support had worse outcomes, and independent risk factors were associated with higher mortality in this population.
Abstract
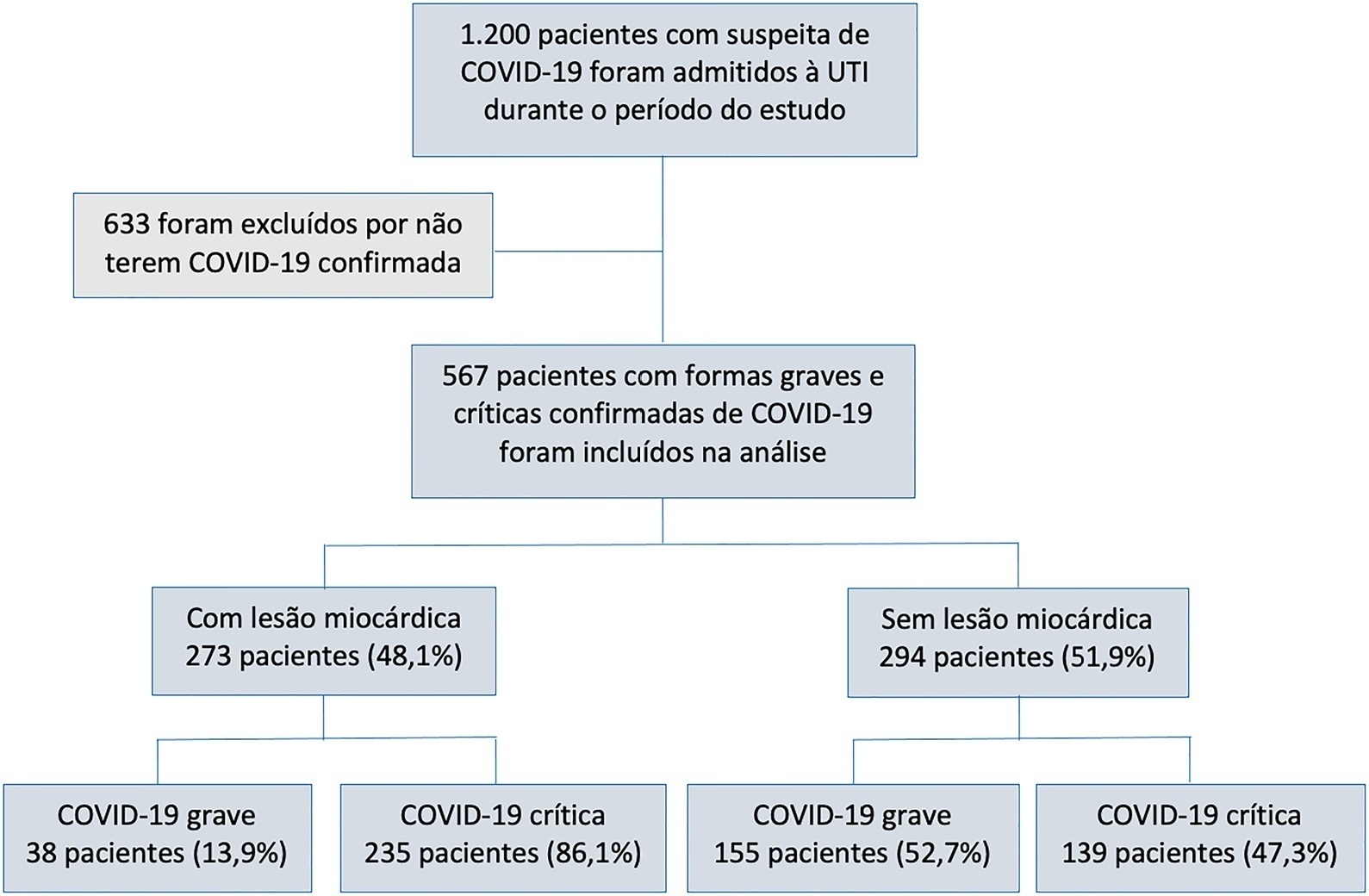
Rev Bras Ter Intensiva. 2022;34(4):443-451
DOI 10.5935/0103-507X.20220440-en
To characterize myocardial injury and cardiovascular complications and their predictors in severe and critical COVID-19 patients admitted to the intensive care unit.
This was an observational cohort study of severe and critical COVID-19 patients admitted to the intensive care unit. Myocardial injury was defined as blood levels of cardiac troponin above the 99th percentile upper reference limit. Cardiovascular events considered were the composite of deep vein thrombosis, pulmonary embolism, stroke, myocardial infarction, acute limb ischemia, mesenteric ischemia, heart failure and arrhythmia. Univariate and multivariate logistic regression or Cox proportional hazard models were used to determine predictors of myocardial injury.
Of 567 patients with severe and critical COVID-19 admitted to the intensive care unit, 273 (48.1%) had myocardial injury. Of the 374 patients with critical COVID-19, 86.1% had myocardial injury, and also showed more organ dysfunction and higher 28-day mortality (56.6% versus 27.1%, p < 0.001). Advanced age, arterial hypertension and immune modulator use were predictors of myocardial injury. Cardiovascular complications occurred in 19.9% of patients with severe and critical COVID-19 admitted to the intensive care unit, with most events occurring in patients with myocardial injury (28.2% versus 12.2%, p < 0.001). The occurrence of an early cardiovascular event during intensive care unit stay was associated with higher 28-day mortality compared with late or no events (57.1% versus 34% versus 41.8%, p = 0.01).
Myocardial injury and cardiovascular complications were commonly found in patients with severe and critical forms of COVID-19 admitted to the intensive care unit, and both were associated with increased mortality in these patients.
Abstract
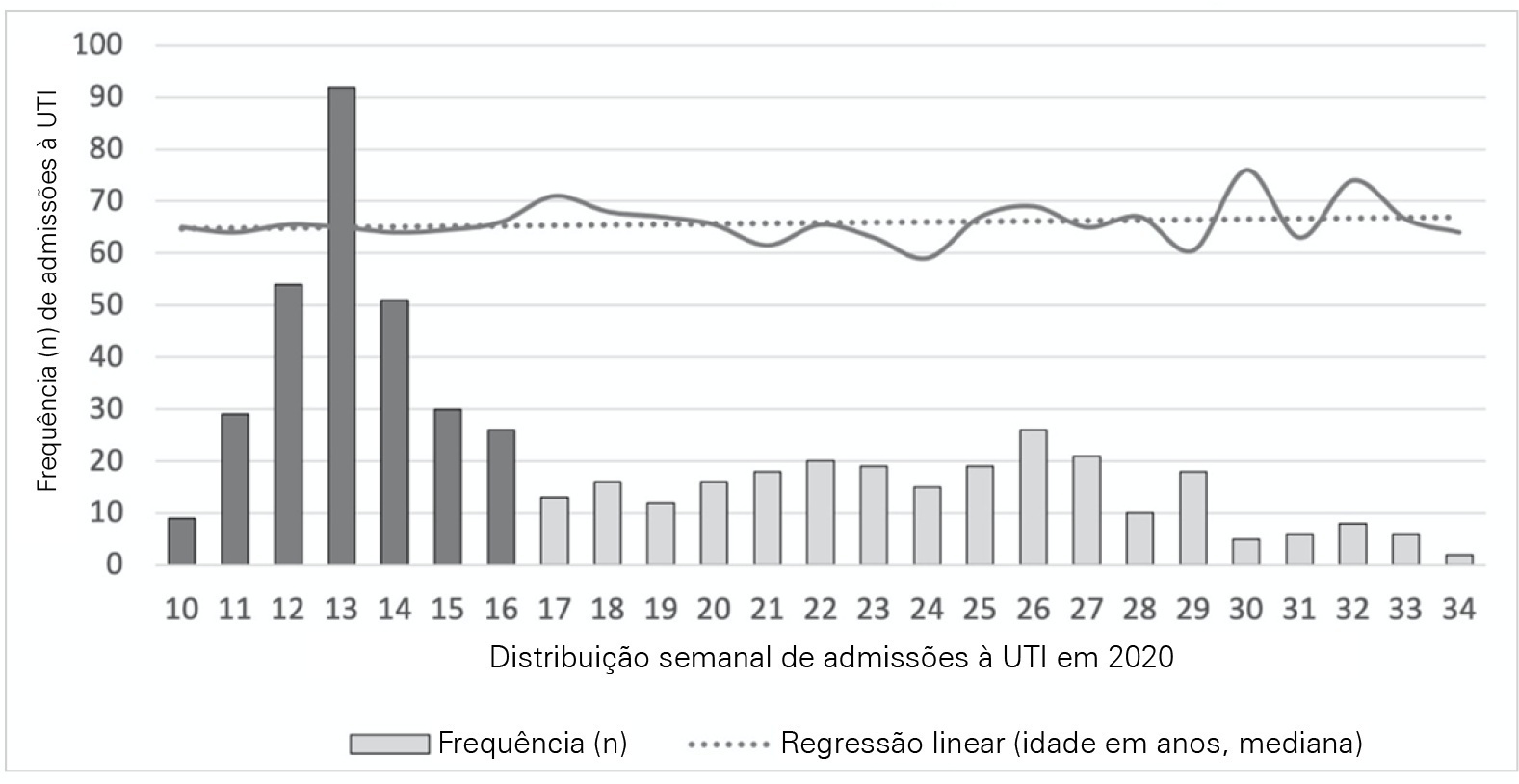
Rev Bras Ter Intensiva. 2022;34(4):433-442
DOI 10.5935/0103-507X.20210037-en
To analyze and compare COVID-19 patient characteristics, clinical management and outcomes between the peak and plateau periods of the first pandemic wave in Portugal.
This was a multicentric ambispective cohort study including consecutive severe COVID-19 patients between March and August 2020 from 16 Portuguese intensive care units. The peak and plateau periods, respectively, weeks 10 - 16 and 17 - 34, were defined.
Five hundred forty-one adult patients with a median age of 65 [57 - 74] years, mostly male (71.2%), were included. There were no significant differences in median age (p = 0.3), Simplified Acute Physiology Score II (40 versus 39; p = 0.8), partial arterial oxygen pressure/fraction of inspired oxygen ratio (139 versus 136; p = 0.6), antibiotic therapy (57% versus 64%; p = 0.2) at admission, or 28-day mortality (24.4% versus 22.8%; p = 0.7) between the peak and plateau periods. During the peak period, patients had fewer comorbidities (1 [0 - 3] versus 2 [0 - 5]; p = 0.002) and presented a higher use of vasopressors (47% versus 36%; p < 0.001) and invasive mechanical ventilation (58.1 versus 49.2%; p < 0.001) at admission, prone positioning (45% versus 36%; p = 0.04), and hydroxychloroquine (59% versus 10%; p < 0.001) and lopinavir/ritonavir (41% versus 10%; p < 0.001) prescriptions. However, a greater use of high-flow nasal cannulas (5% versus 16%, p < 0.001) on admission, remdesivir (0.3% versus 15%; p < 0.001) and corticosteroid (29% versus 52%, p < 0.001) therapy, and a shorter ICU length of stay (12 days versus 8, p < 0.001) were observed during the plateau.
There were significant changes in patient comorbidities, intensive care unit therapies and length of stay between the peak and plateau periods of the first COVID-19 wave.
Abstract
Rev Bras Ter Intensiva. 2022;34(3):342-350
DOI 10.5935/0103-507X.20220229-en
To evaluate whether critical SARS-CoV-2 infection is more frequently associated with signs of corticospinal tract dysfunction and other neurological signs, symptoms, and syndromes, than other infectious pathogens.
This was a prospective cohort study with consecutive inclusion of patients admitted to intensive care units due to primary infectious acute respiratory distress syndrome requiring invasive mechanical ventilation > 48 hours. Eligible patients were randomly assigned to three investigators for clinical evaluation, which encompassed the examination of signs of corticospinal tract dysfunction. Clinical data, including other neurological complications and possible predictors, were independently obtained from clinical records.
We consecutively included 54 patients with acute respiratory distress syndrome, 27 due to SARS-CoV-2 and 27 due to other infectious pathogens. The groups were comparable in most characteristics. COVID-19 patients presented a significantly higher risk of neurological complications (RR = 1.98; 95%CI 1.23 - 3.26). Signs of corticospinal tract dysfunction tended to be more prevalent in COVID-19 patients (RR = 1.62; 95%CI 0.72 - 3.44).
Our study is the first comparative analysis between SARS-CoV-2 and other infectious pathogens, in an intensive care unit setting, assessing neurological dysfunction. We report a significantly higher risk of neurological dysfunction among COVID-19 patients. As such, we suggest systematic screening for neurological complications in severe COVID-19 patients.