Abstract
Rev Bras Ter Intensiva. 2022;34(1):96-106
DOI 10.5935/0103-507X.20220004-en
Early reversion of sepsis-induced tissue hypoperfusion is essential for survival in septic shock. However, consensus regarding the best initial resuscitation strategy is lacking given that interventions designed for the entire population with septic shock might produce unnecessary fluid administration. This article reports the rationale, study design and analysis plan of the ANDROMEDA-2 study, which aims to determine whether a peripheral perfusion-guided strategy consisting of capillary refill time-targeted resuscitation based on clinical and hemodynamic phenotypes is associated with a decrease in a composite outcome of mortality, time to organ support cessation, and hospital length of stay compared to standard care in patients with early (< 4 hours of diagnosis) septic shock.
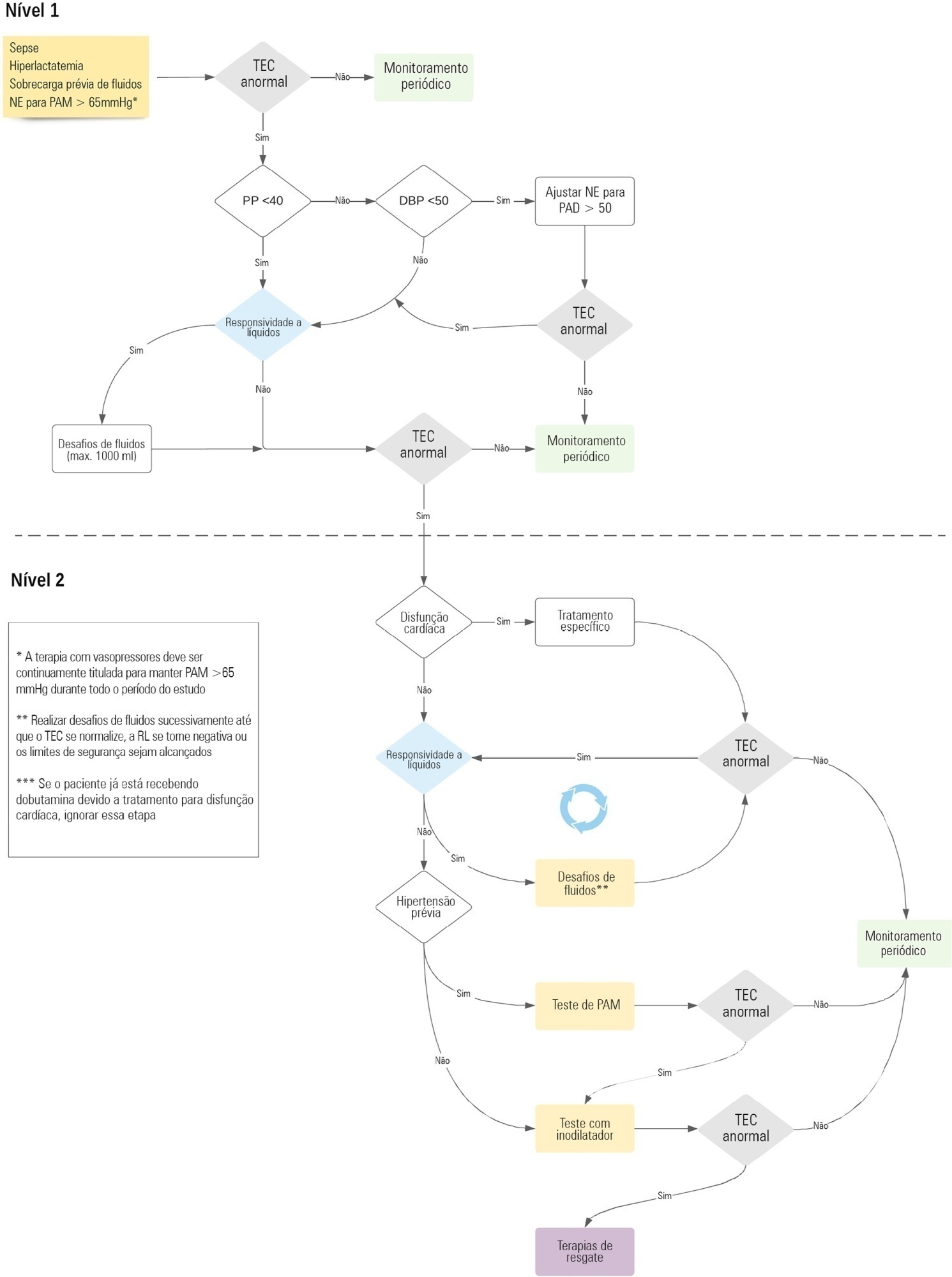
The ANDROMEDA-2 study is a multicenter, multinational randomized controlled trial. In the intervention group, capillary refill time will be measured hourly for 6 hours. If abnormal, patients will enter an algorithm starting with pulse pressure assessment. Patients with pulse pressure less than 40mmHg will be tested for fluid responsiveness and receive fluids accordingly. In patients with pulse pressure > 40mmHg, norepinephrine will be titrated to maintain diastolic arterial pressure > 50mmHg. Patients who fail to normalize capillary refill time after the previous steps will be subjected to critical care echocardiography for cardiac dysfunction evaluation and subsequent management. Finally, vasopressor and inodilator tests will be performed to further optimize perfusion. A sample size of 1,500 patients will provide 88% power to demonstrate superiority of the capillary refill time-targeted strategy.
If hemodynamic phenotype-based, capillary refill time-targeted resuscitation demonstrates to be a superior strategy, care processes in septic shock resuscitation can be optimized with bedside tools.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):423-428
DOI 10.5935/0103-507X.20180060
To evaluate the short-term evolution of patients with septic shock refractory to norepinephrine treated with vasopressin in an intensive care unit of a university hospital.
An unmatched retrospective study (case series) was performed. Clinical, laboratory, and anthropometric data were collected from patients who received vasopressin infusion for treatment of catecholamine-refractory shock from December 2014 to June 2016. For the assessment of severity, APACHE II and SOFA scores were used. The main outcome was mortality at 3 and 30 days.
A total of 80 patients were included, of which 60% were male. In 86.3% of the cases, APACHE II was observed in the highest ranges (> 20). The 30-day mortality was 86.2%, and 75% of the patients died within 72 hours after starting vasopressin.
The series evaluated had high mortality in the first 72 hours of treatment with vasopressin. The use of vasopressin in patients who are refractory to norepinephrine had little or no impact on mortality. It was not possible to exclude the possibility that the high mortality in the present study was linked to the relatively late onset (after established refractoriness of norepinephrine) of vasopressin; this hypothesis should be further evaluated in a randomized study.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):349-352
DOI 10.1590/S0103-507X2009000400003
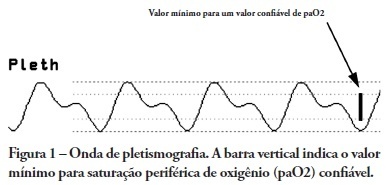
OBJECTIVES: Arterial pulse pressure respiratory variation is a good predictor of fluid response in ventilated patients. Recently, it was shown that respiratory variation in arterial pulse pressure correlates with variation in pulse oximetry plethysmographic waveform amplitude. We wanted to evaluate the correlation between respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude, and to determine whether this correlation was influenced by norepinephrine administration. METHODS: Prospective study of sixty patients with normal sinus rhythm on mechanical ventilation, profoundly sedated and with stable hemodynamics. Oxygenation index and invasive arterial pressure were monitored. Respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude were recorded simultaneously in a beat-to-beat evaluation, and were compared using the Pearson coefficient of agreement and linear regression. RESULTS: Thirty patients (50%) required norepinephrine. There was a significant correlation (K = 0.66; p < 0.001) between respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude. Area under the ROC curve was 0.88 (range, 0.79 - 0.97), with a best cutoff value of 14% to predict a respiratory variation in arterial pulse pressure of 13. The use of norepinephrine did not influence the correlation (K = 0.63, p = 0.001, respectively). CONCLUSIONS: Respiratory variation in arterial pulse pressure above 13% can be accurately predicted by a respiratory variation in pulse oximetry plethysmographic waveform amplitude of 14%. The use of norepinephrine does not alter this relationship.
Abstract
Rev Bras Ter Intensiva. 2008;20(1):49-56
DOI 10.1590/S0103-507X2008000100008
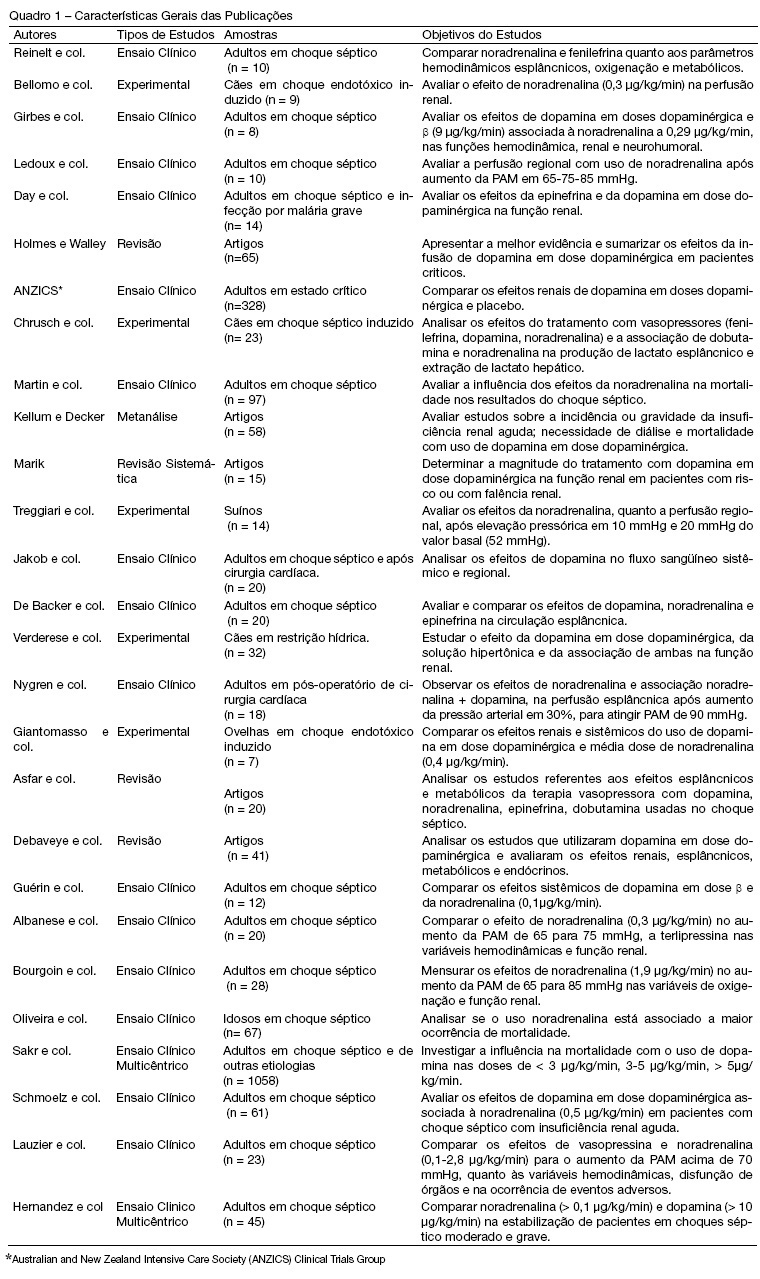
BACKGROUND AND OBJECTIVES: Norepinephrine and dopamine are used, in the state of shock, with the intention of offering hemodynamic support and to reestablish tissue perfusion. The pharmacological effects of these vasopressors can be diverse, for this reason, their use requires, through the clinician, an interpretation of the hemodynamic effects with observation of the systemic variations and region. With this in mind, the objective of this study was to analyze the publications regarding the effects of norepinephrine and low-dose dopamine in hepatosplenic perfusion and renal in treatment of septic shock. METHODS: Articles were selected (n = 27) concerning the use of norepinephrine and dopamine in septic shock, published during the period of 1997 to September 2007, revised in PubMed, data base of the National Library of Medicine (NLM). The MESH method was utilized with the descriptors norepinephrine, dopamine and sepsis. RESULTS: The effects of dopamine and norepinephrine in kidney perfusion are similar; there is an increase in diuresis and no change in creatinine clearance. Norepinephrine did not affect kidney tissue perfusion in spite of the increase of vascular tone. Regarding the splancnic effects, these drugs showed an increase in blood flow, though redistributing the blood in this compartment. CONCLUSIONS: The best agent for the hemodynamic reestablishment that keeps the adequate regional perfusion remains inconclusive.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)