Abstract
Rev Bras Ter Intensiva. 2020;32(1):28-36
DOI 10.5935/0103-507X.20200006
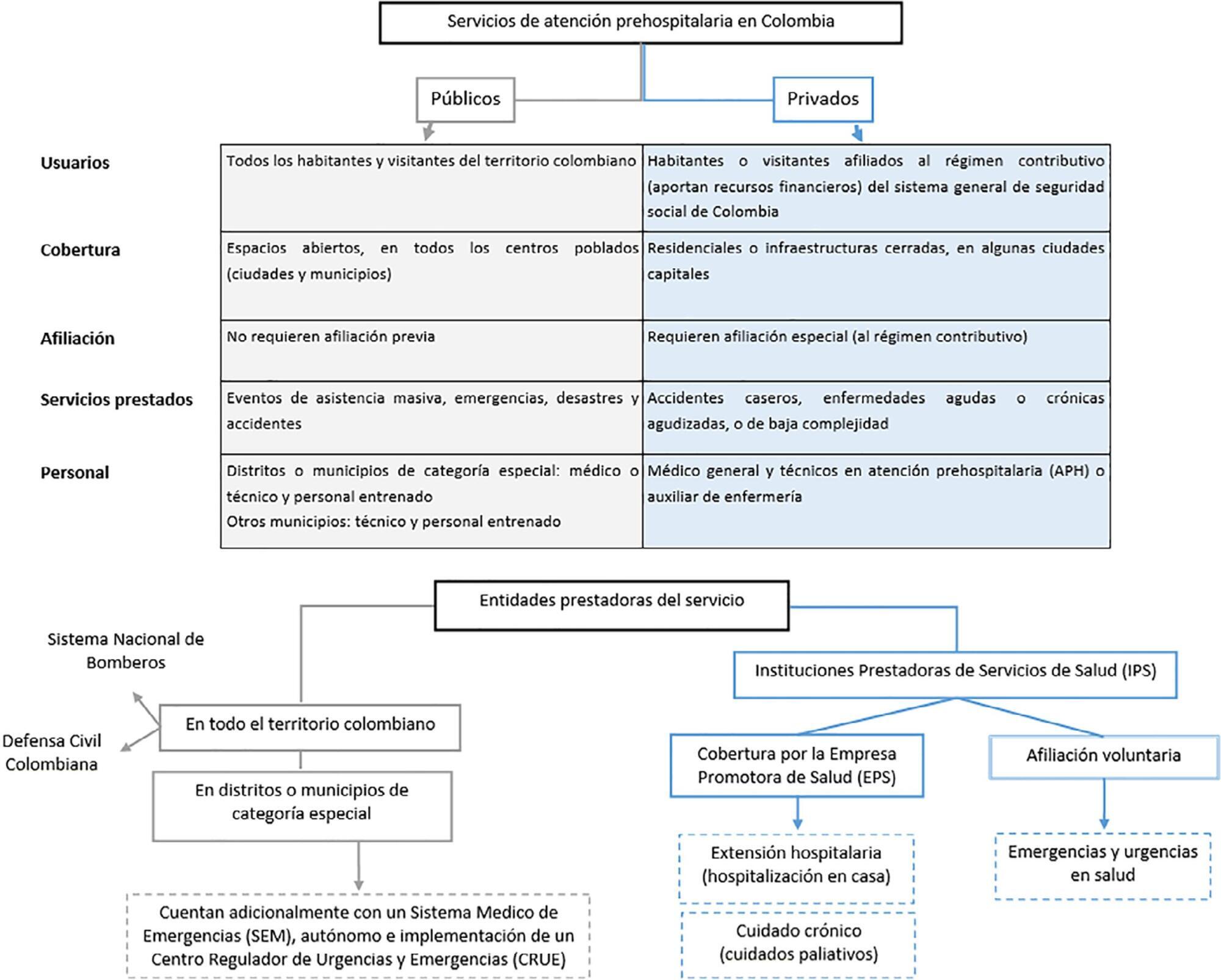
To explore the association between demographic and clinical factors and the presentation of septic shock in patients treated by prehospital emergency services in five Colombian cities between 2015 and 2016.
This was a cross-sectional study with retrospective data collection. Clinical and demographic data were collected from the medical records of patients diagnosed with sepsis who received prehospital care in five Colombian cities in 2015 and 2016. The diagnosis of septic shock was checked in 20% of the cases, generating two analyzed scenarios: observed and verified. Data were analyzed using the chi-square test, Student’s t test and an adjusted logistic regression model. Covariates with p < 0.05 were considered significant.
There was a higher frequency of septic shock in women (62.6%) and in individuals older than 80 years (64.5%), but these were not differentiating factors for septic shock. The most common source of infection was the urinary tract. In the observed scenario, age over 60 (prevalence ratio (PR): 3.22; 95% confidence interval (CI): 1.45 - 35.01) and history of cancer (PR: 1.20; 95%CI: 1.2 - 12.87) were the characteristics associated with septic shock, whereas in the verified scenario, chronic obstructive pulmonary disease (PR: 1.99; 95%CI: 1.26 - 7.14), history of cancer (PR: 1.15; 95%CI: 1.11 - 6.62) and presence of hypovolemia (PR: 1.41; 95%CI: 1.02 - 5.50) were observed.
The most important risk factors for septic shock in prehospital care patients in five Colombian cities were oncological and pulmonary diseases and hypovolemia.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):2-10
DOI 10.5935/0103-507X.20200002
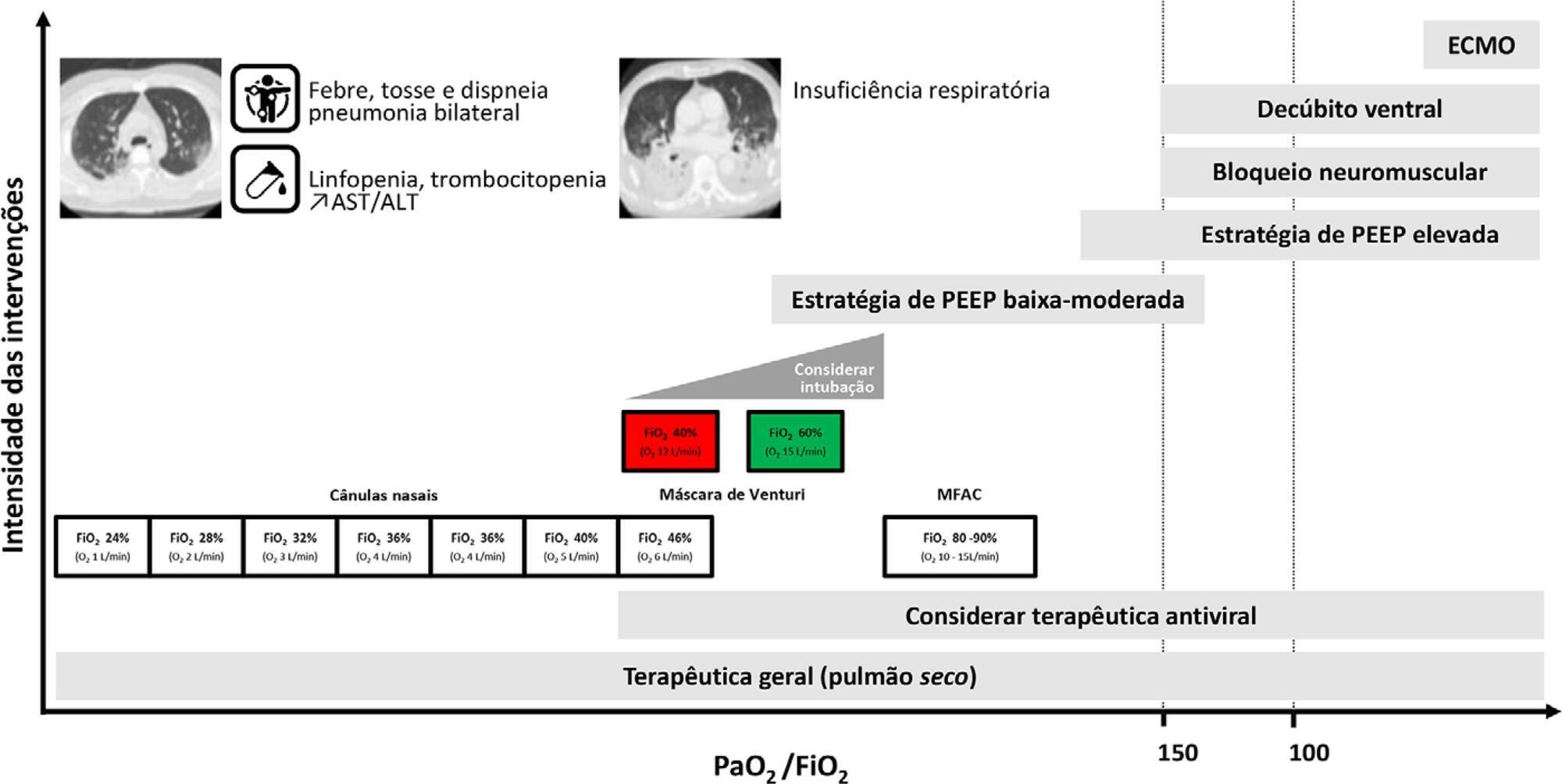
Current COVID-19 epidemics was declared on December 31, 2019 at the Wuhan city seafood market, rapidly spreading throughout China, and later reaching several countries (mainly South Korea, Japan, Italy and Iran) and, since March 1, reaching Portugal. Most of the infected patients present with mild symptoms, not requiring hospitalization. Among those admitted to the hospital, 6% to 10% require admission to the intensive care unit. These recommendations are aimed to support the organization of intensive care services to respond COVID-19, providing optimized care to the patient and protection for healthcare professionals.
Abstract
Rev Bras Ter Intensiva. 2020;32(1):108-114
DOI 10.5935/0103-507X.20200016
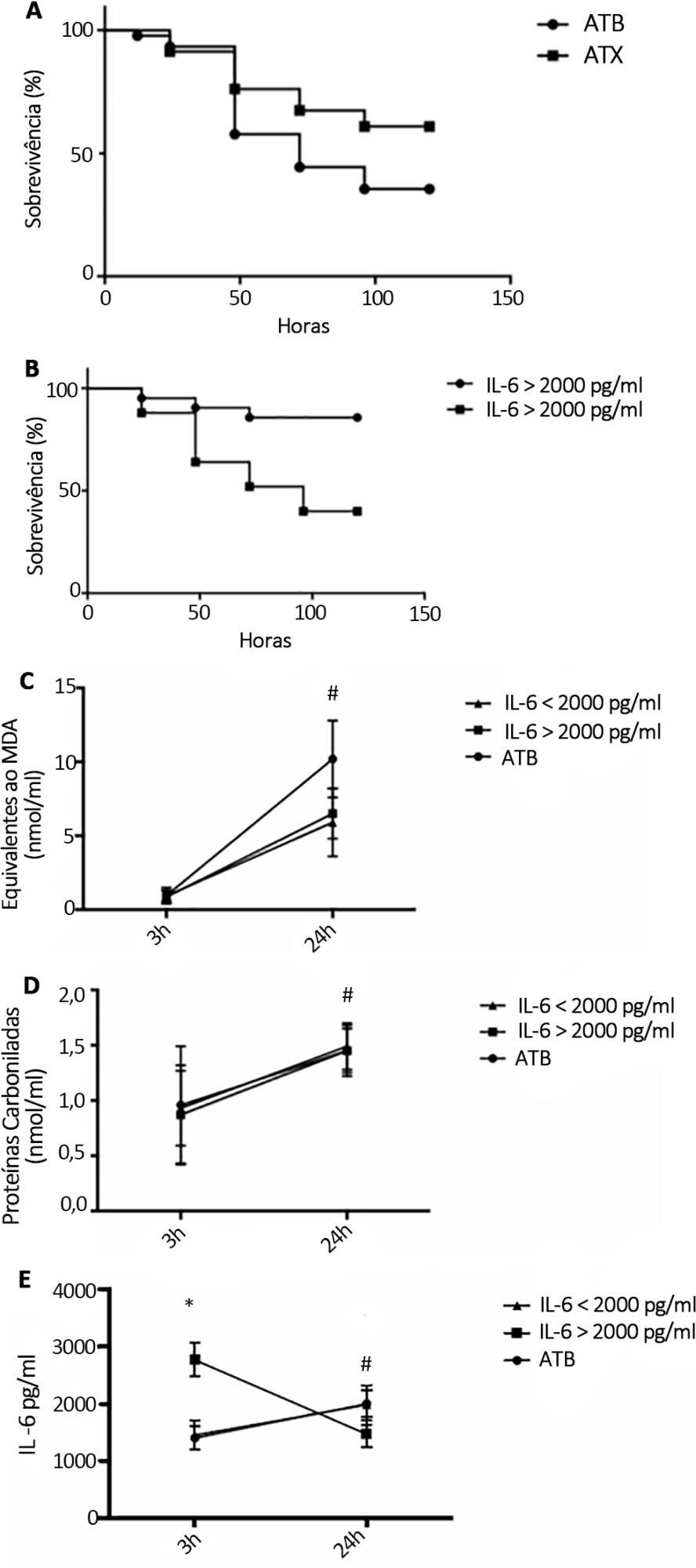
To examine the effectiveness of stratification to identify and target antioxidant therapy for animal models of lethal sepsis and in patients who develop sustained hypotension.
Rats were subjected to sepsis induced by cecal ligation and puncture. Animals were divided into two groups: those with high and low plasma levels of interleukin-6. Following stratification, N-acetylcysteine plus deferoxamine or saline was administered to animals starting 3 and 12 hours after surgery. N-Acetylcysteine plus deferoxamine or placebo was administered within 12 hours of meeting the inclusion criteria in hypotensive patients.
N-Acetylcysteine plus deferoxamine increased survival in the cecal ligation and puncture model when administered 3 and 12 hours after sepsis induction. When dividing animals that received antioxidants using plasma interleukin-6 levels, the protective effect was observed only in those animals with high IL-6 levels. The antioxidant effect of N-acetylcysteine + deferoxamine was similar in the two groups, but a significant decrease in plasma interleukin-6 levels was observed in the high-interleukin-6-level group. Compared with patients treated with antioxidants in the low-interleukin-6 subgroup, those in the high-interleukin-6 subgroup had a lower incidence of acute kidney injury but were not different in terms of acute kidney injury severity or intensive care unit mortality.
Targeting antioxidant therapy to a high inflammatory phenotype would select a responsive population.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):340-346
DOI 10.5935/0103-507X.20190049
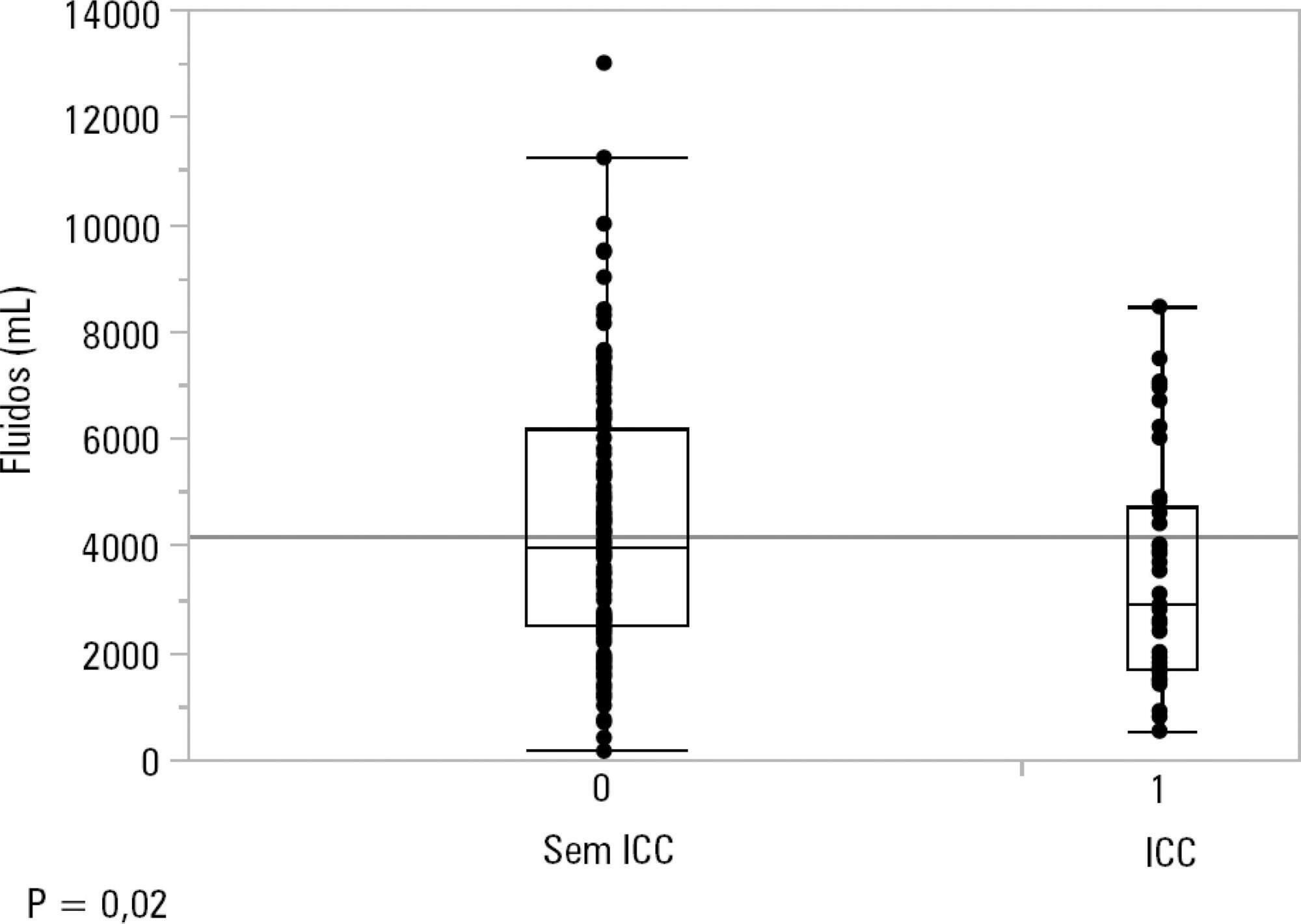
To identify the underlying factors that affect fluid resuscitation in septic patients.
The present study was a case-control study of 181 consecutive patients admitted to a Medical Intensive Care Unit between 2012 and 2016 with a diagnosis of sepsis. Demographic, clinical, radiological and laboratory data were analyzed.
One hundred-thirty patients (72%) received ≥ 30mL/kg of IV fluids on admission. On univariate analyses, a past history of coronary artery disease and heart failure was associated with less fluid therapy. On multivariate analyses, a history of heart failure (OR = 2.31; 95%CI 1.04 - 5.14) remained significantly associated with receiving less IV fluids. Left ventricular ejection fraction, systolic/diastolic function, left ventricular hypertrophy and pulmonary hypertension were not associated with IV fluids. The amount of IV fluids was not associated with differences in mortality. During the first 24 hours, patients with a past history of heart failure received 2,900mLof IV fluids [1,688 - 4,714mL] versus 3,977mL [2,500 - 6,200mL] received by those without a history of heart failure, p = 0.02.
Septic patients with a past history of heart failure received 1L less IV fluids in the first 24 hours with no difference in mortality.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):368-378
DOI 10.5935/0103-507X.20190060
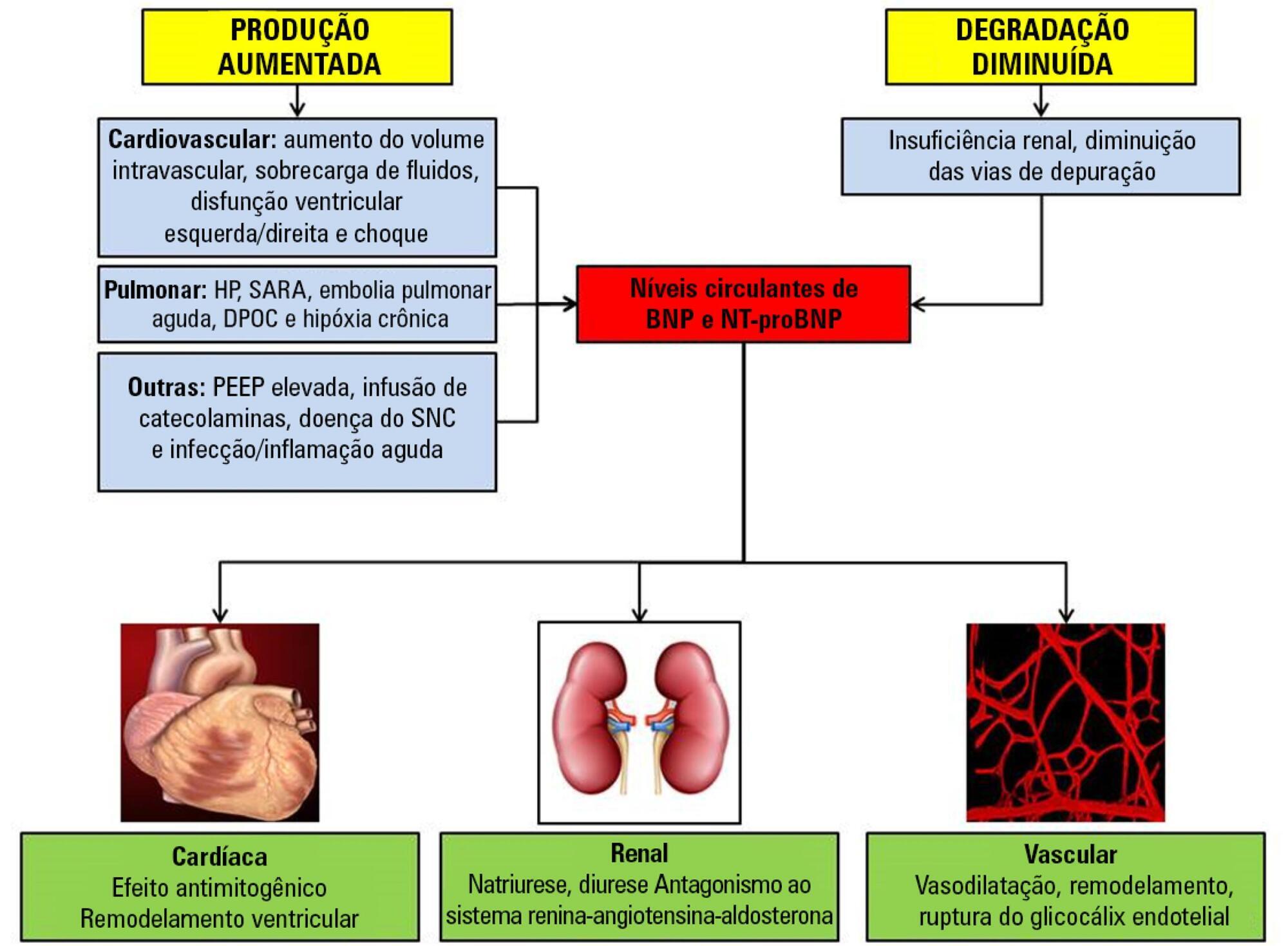
Sepsis continues to be a leading public health burden in the United States and worldwide. With the increasing use of advanced laboratory technology, there is a renewed interest in the use of biomarkers in sepsis to aid in more precise and targeted decision-making. Natriuretic peptides have been increasingly recognized to play a role outside of heart failure. They are commonly elevated among critically ill patients in the setting of cardiopulmonary dysfunction and may play a role in identifying patients with sepsis and septic shock. There are limited data on the role of these biomarkers in the diagnosis, management, outcomes and prognosis of septic patients. This review seeks to describe the role of natriuretic peptides in fluid resuscitation, diagnosis of ventricular dysfunction and outcomes and the prognosis of patients with sepsis. B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) have been noted to be associated with left ventricular systolic and diastolic and right ventricular dysfunction in patients with septic cardiomyopathy. BNP/NT-proBNP may predict fluid responsiveness, and trends of these peptides may play a role in fluid resuscitation. Despite suggestions of a correlation with mortality, the role of BNP in mortality outcomes and prognosis during sepsis needs further evaluation.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):122-128
DOI 10.5935/0103-507X.20190037
To evaluate the impact of the presence of sepsis on in-hospital mortality after intensive care unit discharge.
Retrospective, observational, single-center study. All consecutive patients discharged alive from the intensive care unit of Hospital Vila Franca de Xira (Portugal) from January 1 to December 31, 2015 (N = 473) were included and followed until death or hospital discharge. In-hospital mortality after intensive care unit discharge was calculated for septic and non-septic patients.
A total of 61 patients (12.9%) died in the hospital after being discharged alive from the intensive care unit. This rate was higher among the patients with sepsis on admission, 21.4%, whereas the in-hospital, post-intensive care unit mortality rate for the remaining patients was nearly half that, 9.3% (p < 0.001). Other patient characteristics associated with mortality were advanced age (p = 0.02), male sex (p < 0.001), lower body mass index (p = 0.02), end-stage renal disease (p = 0.04) and high Simplified Acute Physiology Score II (SAPS II) at intensive care unit admission (p < 0.001), the presence of shock (p < 0.001) and medical admission (p < 0.001). We developed a logistic regression model and identified the independent predictors of in-hospital mortality after intensive care unit discharge.
Admission to the intensive care unit with a sepsis diagnosis is associated with an increased risk of dying in the hospital, not only in the intensive care unit but also after resolution of the acute process and discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2019;31(1):93-105
DOI 10.5935/0103-507X.20190001
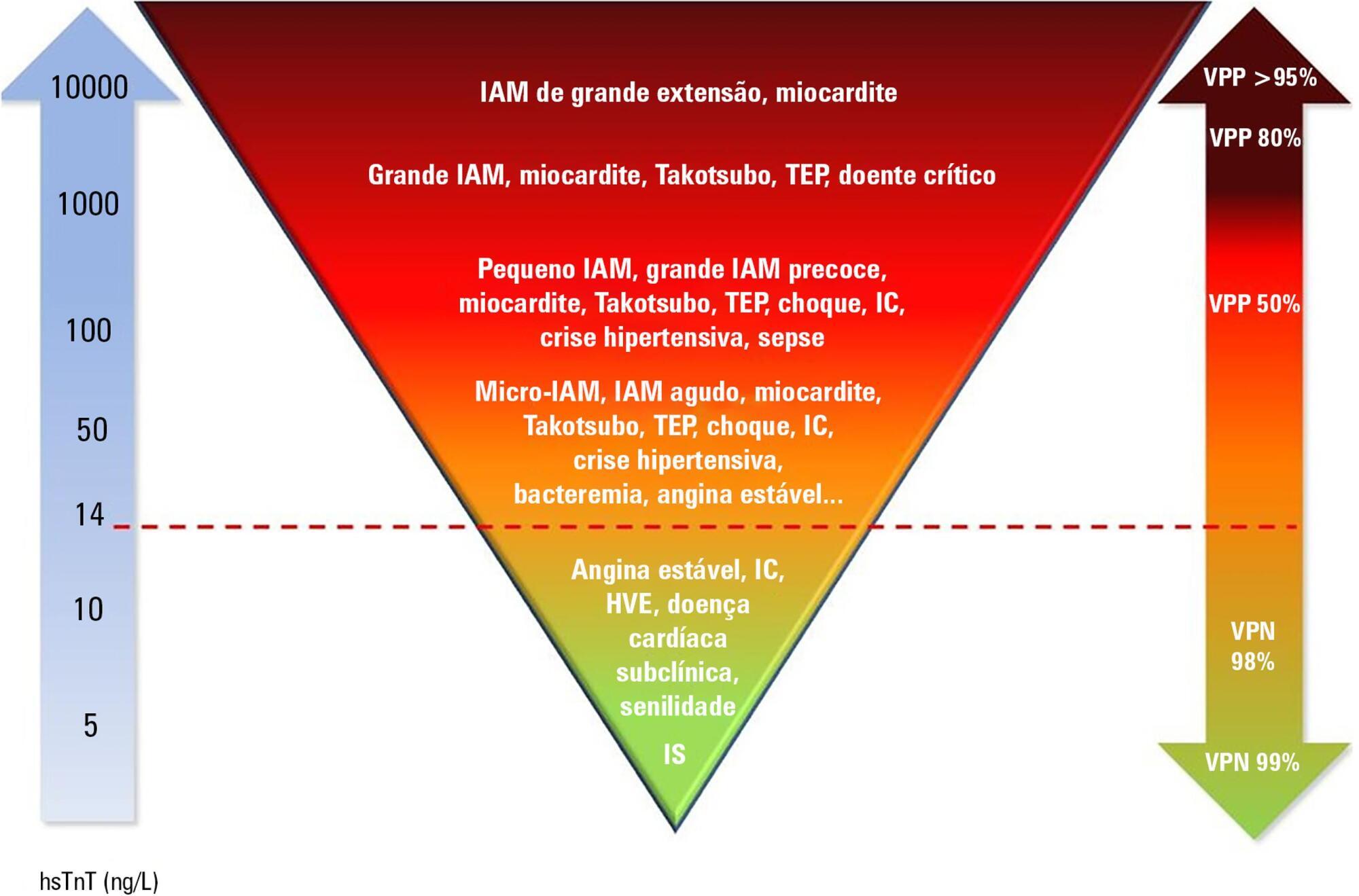
Cardiac troponins T and I are considered highly sensitive and specific markers for the diagnosis of acute myocardial infarction. Currently, a series of nonprimary cardiac abnormalities may manifest as an elevation in high-sensitive assays. The reduction in their detection limits has allowed earlier diagnosis and the use of evidence-based therapeutic measures; however, this characteristic has increased the spectrum of detectable noncoronary heart diseases, which poses challenges for characterizing acute coronary syndromes and creates a new role for these tests in known disorders in intensive care units, especially sepsis. Management of patients through a greater understanding of how these markers behave should be re-evaluated to ensure their correct interpretation.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):443-452
DOI 10.5935/0103-507X.20180064
To evaluate the accuracy of IL-3 to predict the outcome of septic patients.
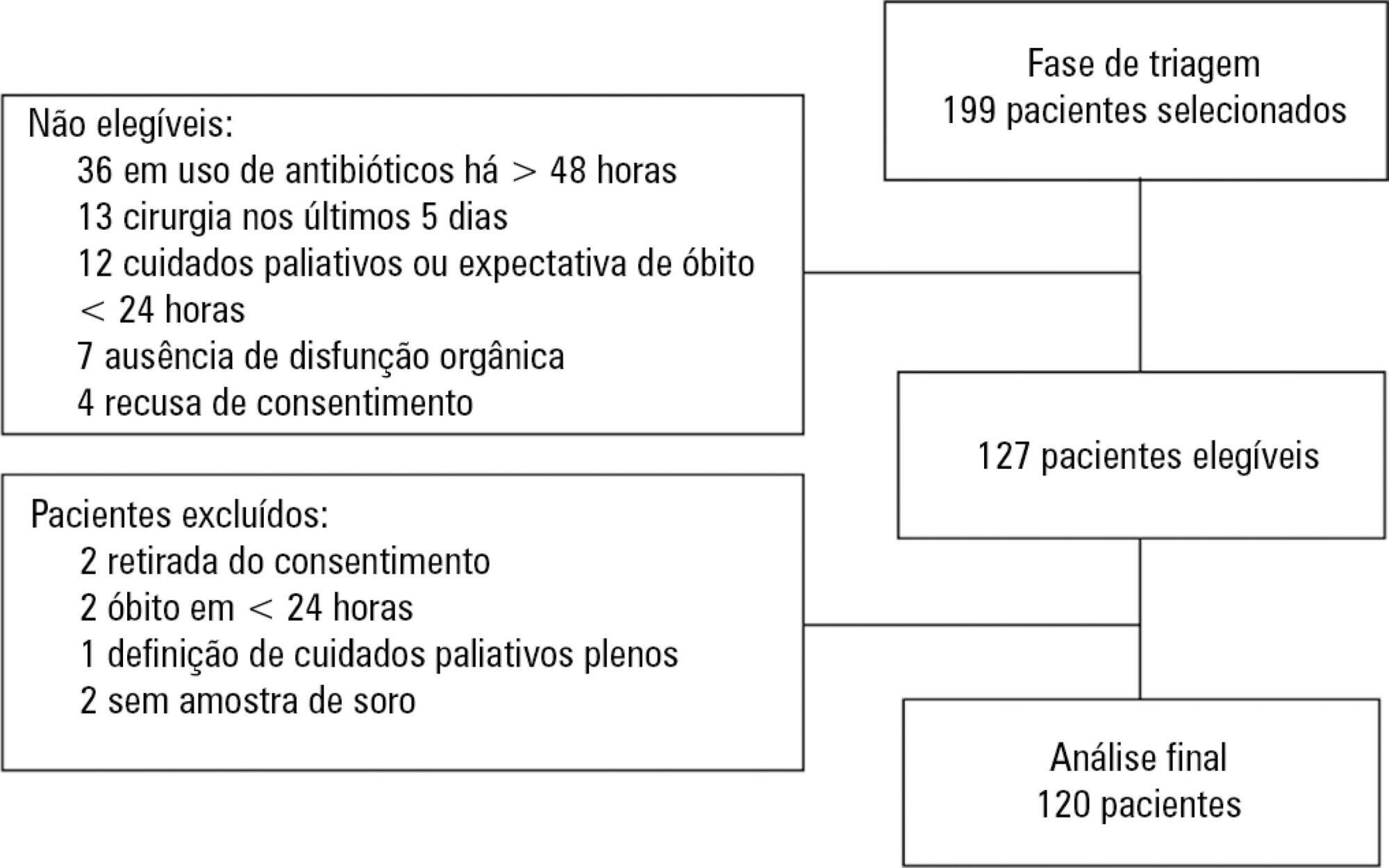
Prospective cohort study with adult patients in an intensive care unit with sepsis or septic shock diagnosed within the previous 48 hours. Circulating IL-3 levels were measured upon inclusion (day 1) and on days 3 and 7. The primary outcome was hospital mortality.
One hundred and twenty patients were included. Serum levels of IL-3 on day 1 were significantly higher among patients who died than among patients who survived the hospital stay (91.2pg/mL versus 36pg/mL, p = 0.024). In a Cox survival model considering the IL-3 levels at inclusion, age and sequential SOFA, IL-3 values remained independently associated with mortality (HR 1.032; 95%CI 1.010 - 1.055; p = 0.005). An receiver operating characteristic curve was built to further investigate the accuracy of IL-3, with an area under the curve of 0.62 (95%CI 0.51 - 0.73; p = 0.024) for hospital mortality. A cutoff initial IL-3 value above 127.5pg/mL was associated with hospital mortality (OR 2.97; 95%CI: 1.27 - 6.97; p = 0.0019) but with a low performance (82% for specificity, 39% for sensibility, 53% for the positive predictive value, 72% for the negative predictive value, 0.73 for the negative likelihood and 2.16 for the positive likelihood ratio).
Higher levels of IL-3 are shown to be independently associated with hospital mortality in septic patients but with poor clinical performance.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)