Abstract
Crit Care Sci. 2023;35(2):217-225
DOI 10.5935/2965-2774.20230289-pt
To analyze the effect of CytoSorb® on mortality, interleukin levels, vasopressor use and adverse events in patients with sepsis.
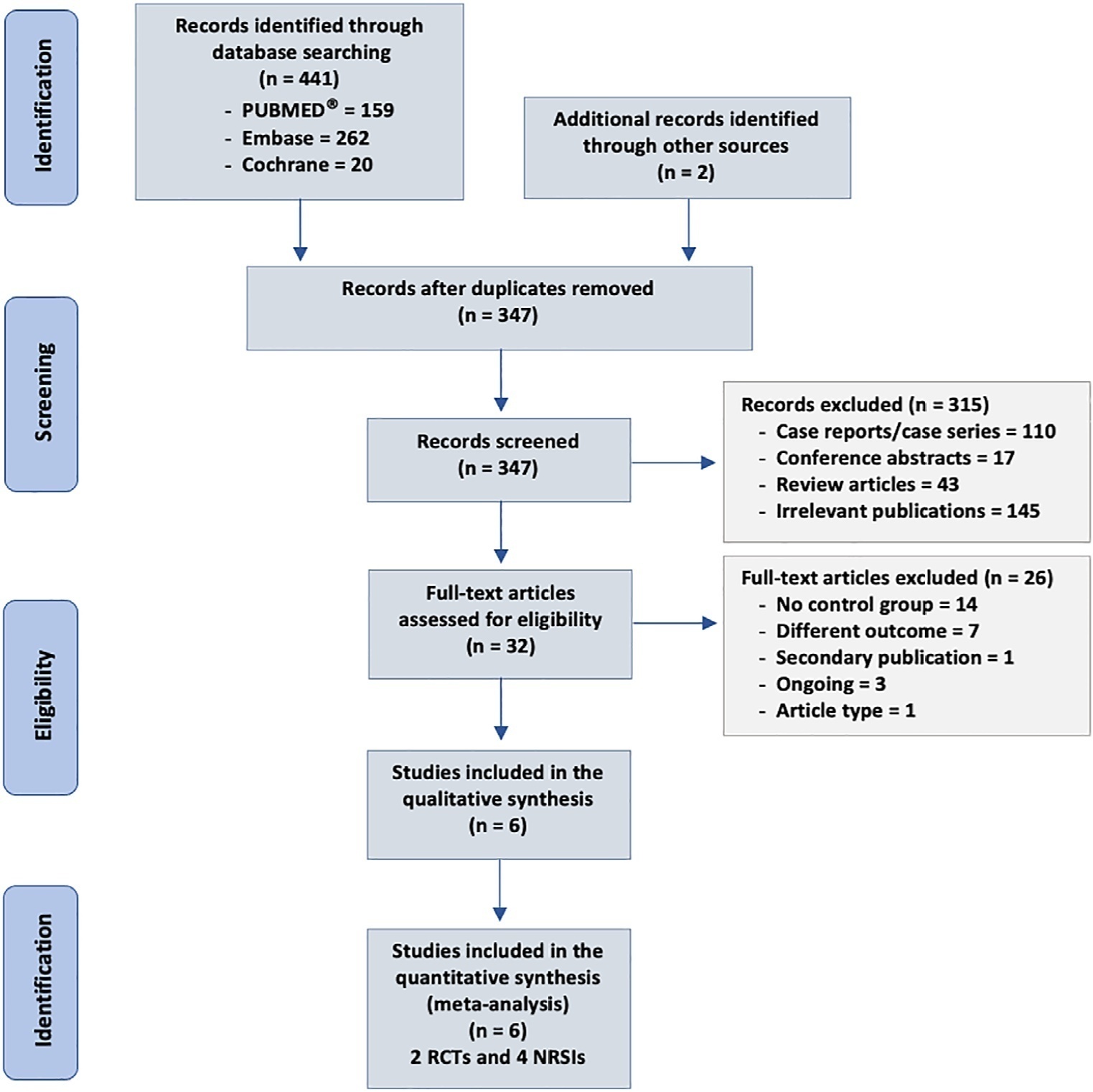
We searched MEDLINE®, Embase and the Cochrane Library for randomized controlled trials and cohort studies that reported the use of CytoSorb® among septic patients. The primary outcome was mortality, and secondary outcomes included the use of vasopressors, levels of inflammatory markers, predicted versus observed mortality, length of stay in the intensive care unit, and adverse events.
We included 6 studies enrolling 413 patients, and assessment for risk of bias indicated variations in study quality from high to moderate. The overall mortality rate was 45%, and no significant effect on mortality was found at 28 - 30 days (RR 0.98 [0.12 - 8.25] for the randomized clinical trial and RR 0.74 [0.49 - 1.13] for cohort studies). We did not perform a metanalysis for other outcomes due to the small number of studies found or the lack of data.
Our study found very low certainty evidence, due to imprecision, risk of bias, and heterogeneity, thereby showing no benefit of CytoSorb® use in terms of mortality at 28 - 30 days. We cannot recommend the use of CytoSorb® in septic or septic shock patients outside clinical trials. Further high-quality randomized trials with a common intervention arm are needed to evaluate the influence of CytoSorb® in this population.
Abstract
Crit Care Sci. 2023;35(1):84-96
DOI 10.5935/2965-2774.20230405-pt
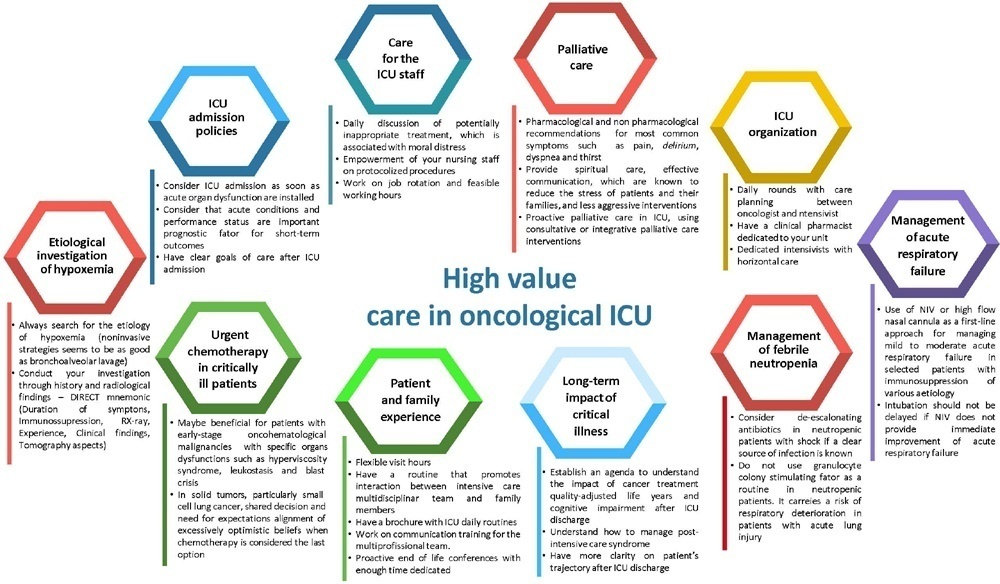
The number of patients with cancer requiring intensive care unit admission is increasing around the world. The improvement in the pathophysiological understanding of this group of patients, as well as the increasingly better and more targeted treatment options for their underlying disease, has led to a significant increase in their survival over the past three decades. Within the organizational concepts, it is necessary to know what adds value in the care of critical oncohematological patients. Practices in medicine that do not benefit patients and possibly cause harm are called low-value practices, while high-value practices are defined as high-quality care at relatively low cost. In this article, we discuss ten domains with high-value evidence in the care of cancer patients: (1) intensive care unit admission policies; (2) intensive care unit organization; (3) etiological investigation of hypoxemia; (4) management of acute respiratory failure; (5) management of febrile neutropenia; (6) urgent chemotherapy treatment in critically ill patients; (7) patient and family experience; (8) palliative care; (9) care of intensive care unit staff; and (10) long-term impact of critical disease on the cancer population. The disclosure of such policies is expected to have the potential to change health care standards. We understand that it is a lengthy process, and initiatives such as this paper are one of the first steps in raising awareness and beginning a discussion about high-value care in various health scenarios.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)