Abstract
Rev Bras Ter Intensiva. 2014;26(4):373-378
DOI 10.5935/0103-507X.20140057
The objective of this study was to translate and culturally adapt the Behavioral Pain Scale to Brazilian Portuguese and to evaluate the psychometric properties of this scale.
This study was conducted in two phases: the Behavioral Pain Scale was translated and culturally adapted to Brazilian Portuguese and the psychometric properties of this scale were subsequently assessed (reliability and clinical utility). The study sample consisted of 100 patients who were older than 18 years of age, admitted to an intensive care unit, intubated, mechanically ventilated, and subjected or not to sedation and analgesia from July 2012 to December 2012. Pediatric and non-intubated patients were excluded. The study was conducted at a large private hospital that was situated in the city of São Paulo (SP).
Regarding reproducibility, the results revealed that the observed agreement between the two evaluators was 92.08% for the pain descriptor “adaptation to mechanical ventilation”, 88.1% for “upper limbs”, and 90.1% for “facial expression”. The kappa coefficient of agreement for “adaptation to mechanical ventilation” assumed a value of 0.740. Good agreement was observed between the evaluators with an intraclass correlation coefficient of 0.807 (95% confidence interval: 0.727-0.866).
The Behavioral Pain Scale was easy to administer and reproduce. Additionally, this scale had adequate internal consistency. The Behavioral Pain Scale was satisfactorily adapted to Brazilian Portuguese for the assessment of pain in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):93-98
DOI 10.5935/0103-507X.20130019
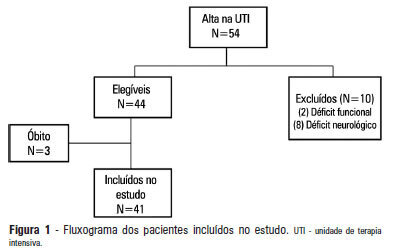
OBJECTIVE: 1) To evaluate the functional independence measures immediately after discharge from an intensive care unit and to compare these values with the FIMs 30 days after that period. 2) To evaluate the possible associated risk factors. METHODS: The present investigation was a prospective cohort study that included individuals who were discharged from the intensive care unit and underwent physiotherapy in the unit. Functional independence was evaluated using the functional independence measure immediately upon discharge from the intensive care unit and 30 days thereafter via a phone call. The patients were admitted to the Hospital Santa Clara intensive care unit during the period from May 2011 to August 2011. RESULTS: During the predetermined period of data collection, 44 patients met the criteria for inclusion in the study. The mean age of the patients was 55.4±10.5 years. Twenty-seven of the subjects were female, and 15 patients were admitted due to pulmonary disease. The patients exhibited an functional independence measure of 84.1±24.2. When this measure was compared to the measure at 30 days after discharge, there was improvement across the functional independence variables except for that concerned with sphincter control. There were no significant differences when comparing the gender, age, clinical diagnosis, length of stay in the intensive care unit, duration of mechanical ventilation, and the presence of sepsis during this period. CONCLUSION: Functional independence, as evaluated by the functional independence measure scale, was improved at 30 days after discharge from the intensive care unit, but it was not possible to define the potentially related factors.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):44-48
DOI 10.1590/S0103-507X2013000100009
OBJECTIVE: To evaluate the effectiveness of a tongue cleaner in the removal of tongue biofilm in mechanically ventilated patients. METHODS: Tongue biofilm and tracheal secretion samples were collected from a total of 50 patients: 27 in the study group (SG) who were intubated or tracheostomized under assisted ventilation and treated with the tongue cleaner and 23 in the control group (CG) who did not undergo tongue cleaning. Oral and tracheal secretion cultures of the SG (initially and after 5 days) and the CG (at a single time-point) were performed to evaluate the changes in bacterial flora. RESULTS: The median age of the SG patients was 77 years (45-99 years), and that of the CG patients was 79 years (21-94 years). The length of hospital stay ranged from 17-1,370 days for the SG with a median stay of 425 days and from 4-240 days for the CG with a median stay of 120 days. No significant differences were found when the dental plaque indexes were compared between the SG and the CG. There was no correlation between the index and the length of hospital stay. The same bacterial flora was found in the dental plaque of 9 of the 27 SG patients before and after the tongue scraper was used for 5 days compared with the CG (p=0.683). Overall, 7 of the 27 SG patients had positive bacterial cultures for the same strains in both tongue biofilm and tracheal secretions compared with the CG (p=0.003). Significant similarities in strain resistance and susceptibility of the assessed microorganisms were observed between oral and tracheal microflora in 6/23 cases in the CG (p=0.006). CONCLUSION: The use of a tongue cleaner is effective at reducing tongue biofilm in patients on mechanical ventilation and facilitates oral hygiene interventions performed by caregivers.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):188-196
DOI 10.5935/0103-507X.20130034
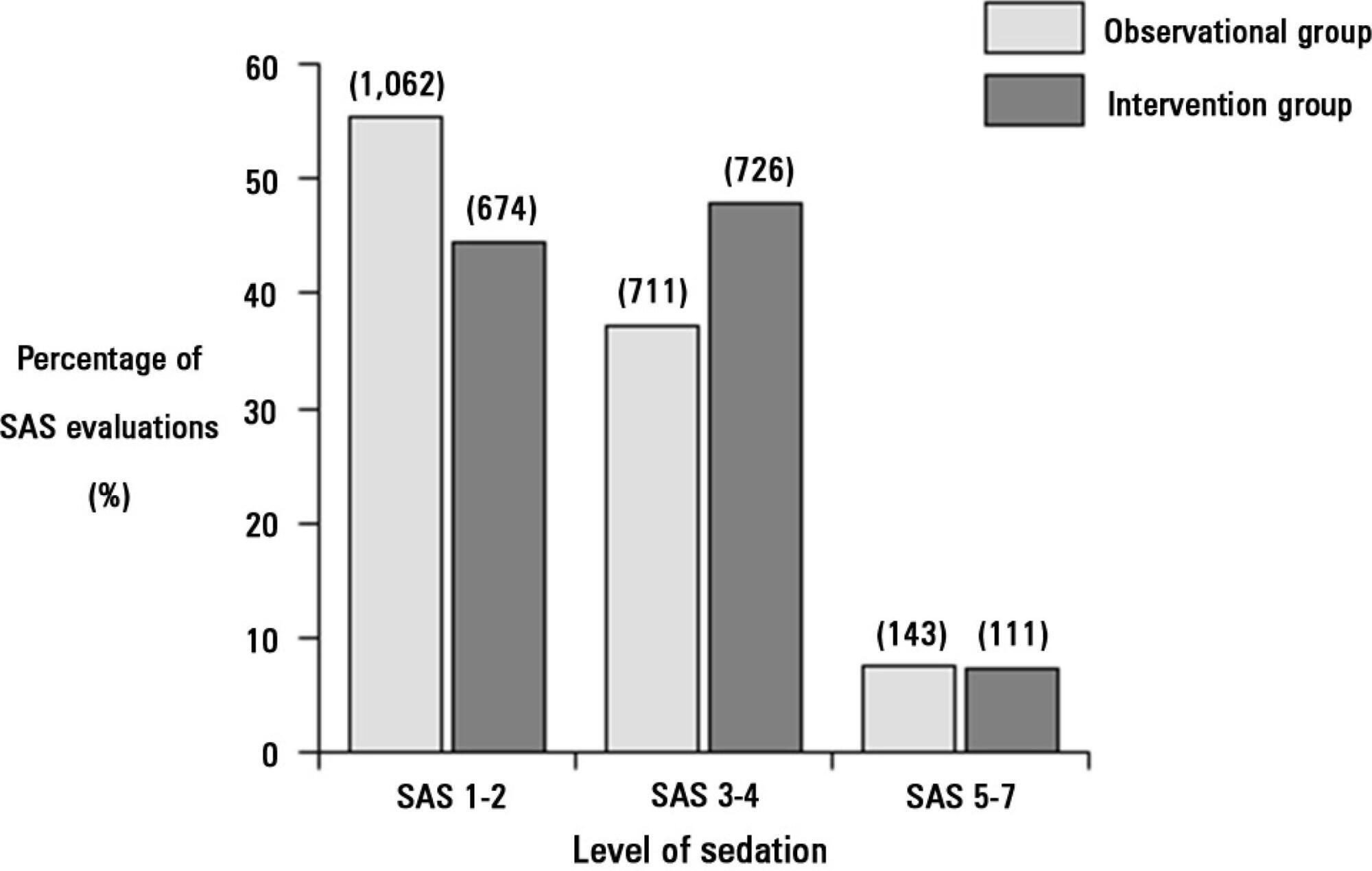
Deep sedation in critically ill patients is associated with a longer duration of mechanical ventilation and a prolonged length of stay in the intensive care unit. Several protocols have been used to improve these outcomes. We implement and evaluate an analgesia-based, goal-directed, nurse-driven sedation protocol used to treat critically ill patients who receive mechanical ventilation.
We performed a prospective, two-phase (before-after), non-randomized multicenter study that involved 13 intensive care units in Chile. After an observational phase (observational group, n=155), we designed, implemented and evaluated an analgesia-based, goal-directed, nurse-driven sedation protocol (intervention group, n=132) to treat patients who required mechanical ventilation for more than 48 hours. The primary outcome was to achieve ventilator-free days by day 28.
The proportion of patients in deep sedation or in a coma decreased from 55.2% to 44.0% in the interventional group. Agitation did not change between the periods and remained approximately 7%. Ventilator-free days to day 28, length of stay in the intensive care unit and mortality were similar in both groups. At one year, post-traumatic stress disorder symptoms in survivors were similar in both groups.
We designed and implemented an analgesia-based, goal-directed, nurse-driven sedation protocol in Chile. Although there was no improvement in major outcomes, we observed that the present protocol was safe and feasible and that it resulted in decreased periods of deep sedation without increasing agitation.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):212-217
DOI 10.5935/0103-507X.20130037
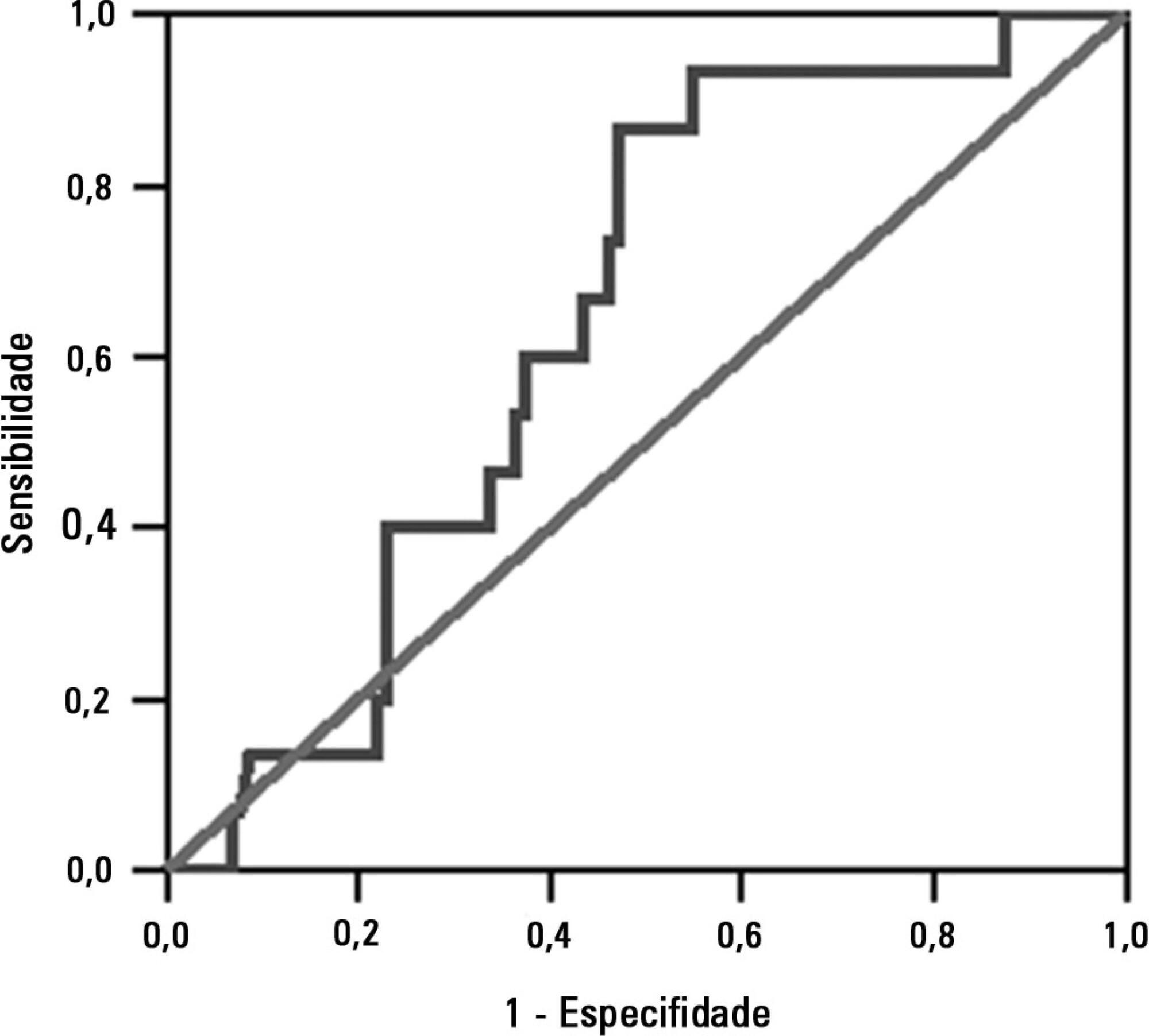
To investigate the association between the rapid shallow breathing index and successful extubation in patients with traumatic brain injury.
This study was a prospective study conducted in patients with traumatic brain injury of both genders who underwent mechanical ventilation for at least two days and who passed a spontaneous breathing trial. The minute volume and respiratory rate were measured using a ventilometer, and the data were used to calculate the rapid shallow breathing index (respiratory rate/tidal volume). The dependent variable was the extubation outcome: reintubation after up to 48 hours (extubation failure) or not (extubation success). The independent variable was the rapid shallow breathing index measured after a successful spontaneous breathing trial.
The sample comprised 119 individuals, including 111 (93.3%) males. The average age of the sample was 35.0±12.9 years old. The average duration of mechanical ventilation was 8.1±3.6 days. A total of 104 (87.4%) participants achieved successful extubation. No association was found between the rapid shallow breathing index and extubation success.
The rapid shallow breathing index was not associated with successful extubation in patients with traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):312-318
DOI 10.5935/0103-507X.20130053
The development of abdominal surgery represents an alternative therapy for the morbidly obese; however, patients undergoing this surgical procedure often experience postoperative pulmonary complications. The use of alveolar recruitment maneuvers and/or perioperative ventilatory strategies is a possible alternative to reduce these complications, focusing on the reduction of postoperative pulmonary complications. In this review, the benefits of perioperative ventilatory strategies and the implementation of alveolar recruitment maneuvers in obese patients undergoing abdominal surgery are described.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):319-326
DOI 10.5935/0103-507X.20130054
In preterm infants, the need for intubation and mechanical ventilation is associated with ventilator-induced lung injuries and subsequent bronchopulmonary dysplasia. The aim of the present review was to improve the understanding of the mechanisms of injury that involve cytokine-mediated inflammation to contribute to the development of new preventive strategies. Relevant articles were retrieved from the PubMed database using the search terms "ventilator-induced lung injury preterm", "continuous positive airway pressure", "preterm", and "bronchopulmonary dysplasia". The resulting data and other relevant information were divided into several topics to ensure a thorough, critical view of ventilation-induced lung injury and its consequences in preterm infants. The role of pro-inflammatory cytokines (particularly interleukins 6 and 8 and tumor necrosis factor alpha) as mediators of lung injury was assessed. Evidence from studies conducted with animals and human newborns is described. This evidence shows that brief periods of mechanical ventilation is sufficient to induce the release of pro-inflammatory cytokines. Other forms of mechanical and non-invasive ventilation were also analyzed as protective alternatives to conventional mechanical ventilation. It was concluded that non-invasive ventilation, intubation followed by early surfactant administration and quick extubation for nasal continuous positive airway pressure, and strategies that regulate tidal volume and avoid volutrauma (such as volume guarantee ventilation) protect against ventilator-induced lung injury in preterm infants.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):263-269
DOI 10.1590/S0103-507X2012000300010
OBJECTIVE: This study evaluated the relationship between nutritional intake and protein and caloric requirements and observed clinical outcomes on the 7th day of intensive care unit stay. METHODS: This was a retrospective cohort study of 126 patients who were admitted to the intensive care unit for >7 days. The patients were categorized according to the adequacy of energy and protein intake in relation to requirements (a >60% Adequate Intake Group and a <60% Inadequate Intake Group). The length of stay, ventilator free time and mortality in the intensive care unit and hospital were evaluated. RESULTS: Enteral nutrition was used in 95.6% of the 126 included patients, and nutrition was initiated 41 hours after admission to the intensive care unit. The adequacy of intake was 84% for energy and 72.5% for protein. No differences in the length of stay [16 (11-23) versus 15 (11-21) days, p=0.862], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.985] or mortality in the intensive care unit [12 (41.4%) versus 38 (39.1%), p=0.831] and hospital [15 (51.7%) versus 44 (45.4%), p=0.348] were observed between the adequate and inadequate energy intake groups, respectively. Similar results in protein intake and the length of hospital stay [15 (12-21) versus 15 (11-21) days, p=0.996], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.846], and mortality in the intensive care unit [15 (28.3%) versus 35 (47.9%), p=0.536)] and hospital [18 (52.9%) versus 41 (44.6%), p=0.262] were observed between groups. CONCLUSION: The results did not establish that energy and protein intakes of greater or less than 60% of nutritional requirements were reliable dividers of clinical outcomes.