Abstract
Rev Bras Ter Intensiva. 2019;31(4):474-482
DOI 10.5935/0103-507X.20190073
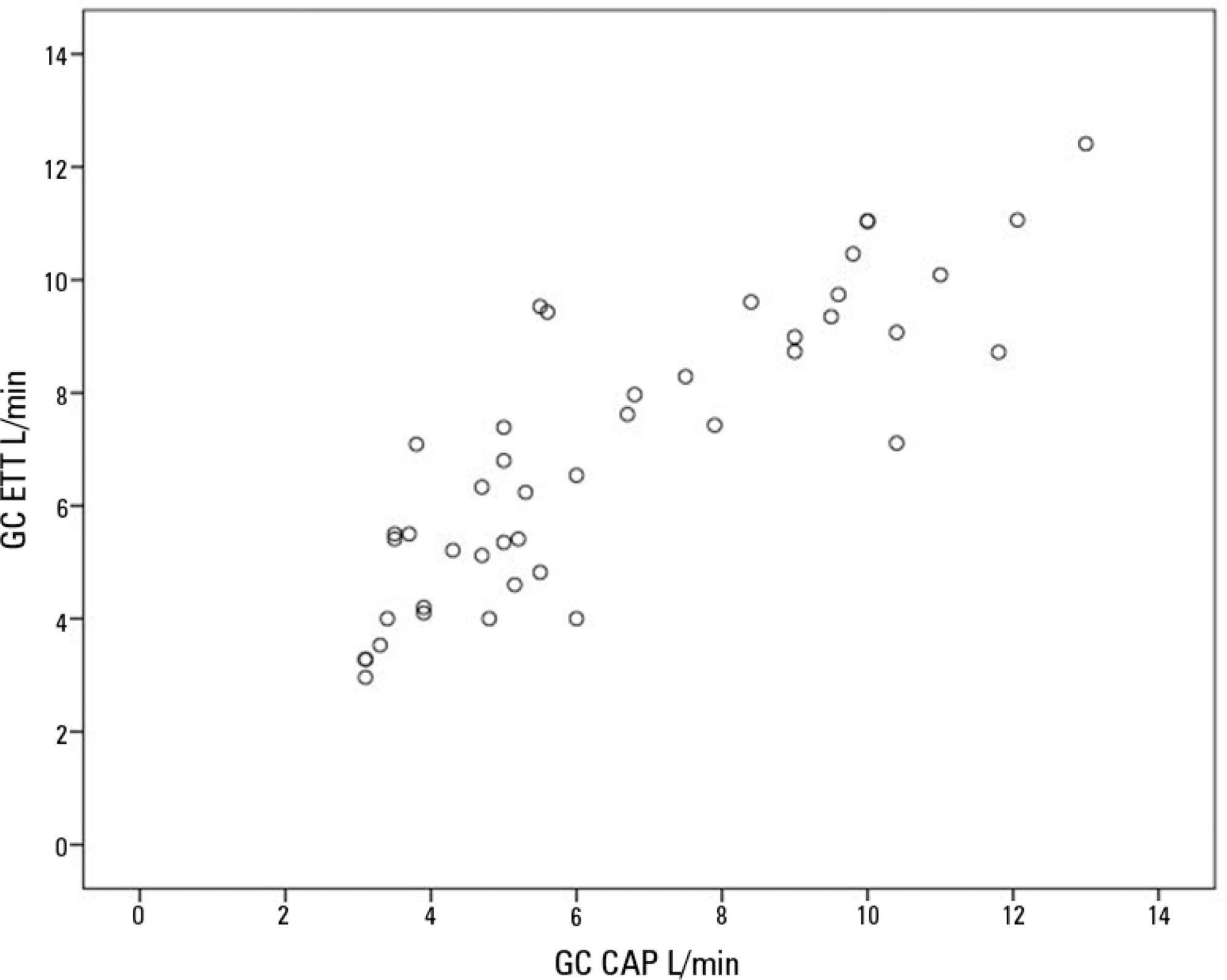
To compare cardiac output measurements by transthoracic echocardiography and a pulmonary artery catheter in mechanically ventilated patients with high positive end-expiratory pressure. To evaluate the effect of tricuspid regurgitation.
Sixteen mechanically ventilated patients were studied. Cardiac output was measured by pulmonary artery catheterization and transthoracic echocardiography. Measurements were performed at different levels of positive end-expiratory pressure (10cmH2O, 15cmH2O, and 20cmH2O). The effect of tricuspid regurgitation on cardiac output measurement was evaluated. The intraclass correlation coefficient was studied; the mean error and limits of agreement were studied with the Bland-Altman plot. The error rate was calculated.
Forty-four pairs of cardiac output measurements were obtained. An intraclass correlation coefficient of 0.908 was found (p < 0.001). The mean error was 0.44L/min for cardiac output values between 5 and 13L/min. The limits of agreement were 3.25L/min and -2.37L/min. With tricuspid insufficiency, the intraclass correlation coefficient was 0.791, and without tricuspid insufficiency, 0.935. Tricuspid insufficiency increased the error rate from 32% to 52%.
In patients with high positive end-expiratory pressure, cardiac output measurement by transthoracic echocardiography is comparable to that with a pulmonary artery catheter. Tricuspid regurgitation influences the intraclass correlation coefficient. In patients with high positive end-expiratory pressure, the use of transthoracic echocardiography to measure cardiac output is comparable to invasive measures.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):483-489
DOI 10.5935/0103-507X.20190071
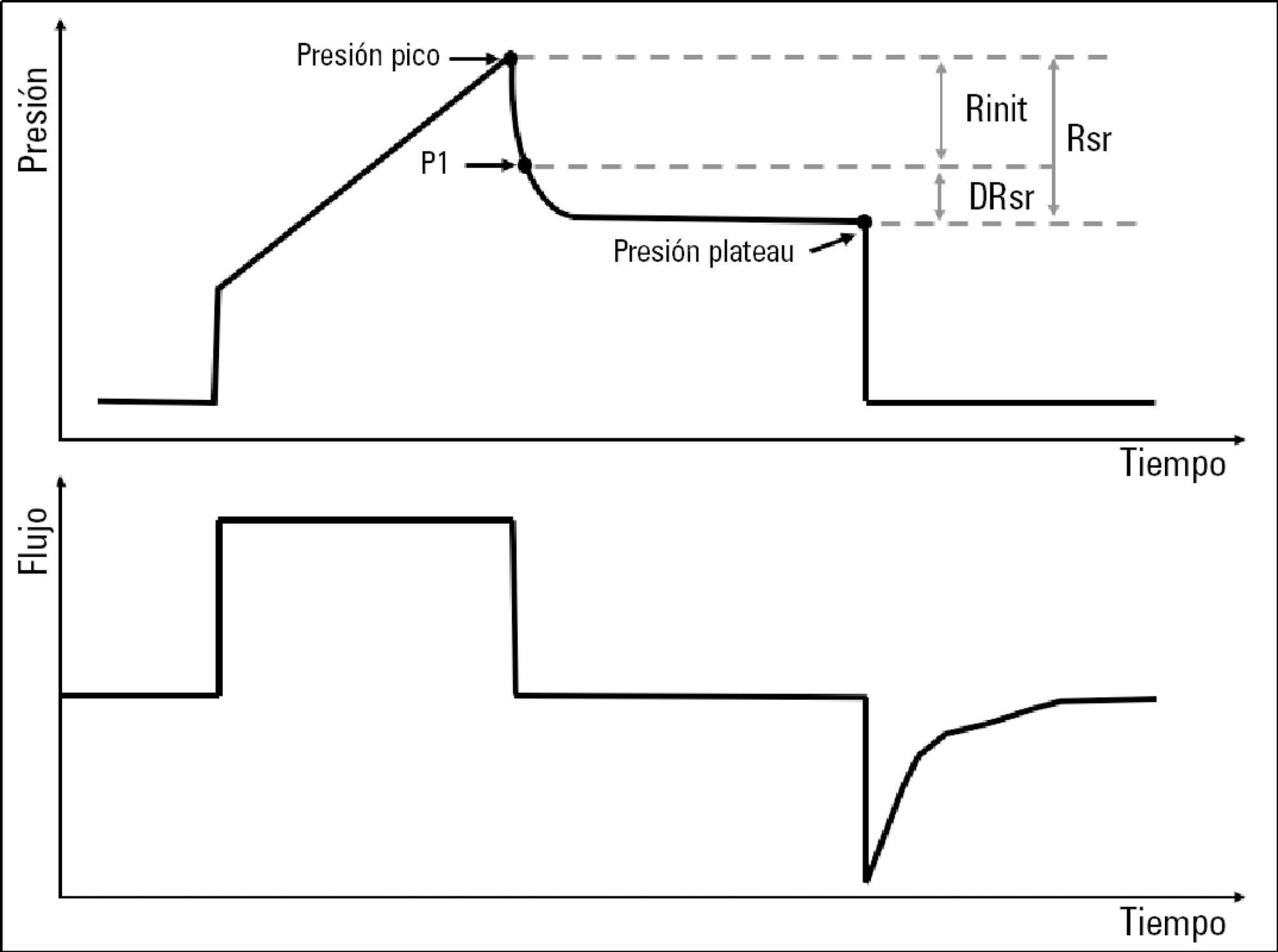
To describe the behavior of inspiratory resistance components when positive end-expiratory pressure (PEEP) increases in patients with acute respiratory distress syndrome under a protective ventilation strategy.
In volume-controlled mode, at 6mL/kg and constant flow, end-inspiratory occlusions were performed at 0, 5 10, 15 and 20cmH2O PEEP. Peak, initial and plateau pressure values were assessed, calculating the maximum, minimum and differential resistances. The results were compared by repeated measures analysis of variance (ANOVA) with post hoc Bonferroni correction, considering p < 0.05 significant.
The highest maximum resistance was observed at the lowest PEEP levels. The values for 10 and 15cmH2O PEEP significantly differed from those for 5 and 0cmH2O PEEP, whereas that for 20cmH2O PEEP only significantly differed from that for 0cmH2O PEEP (p < 0.05). The minimum resistance behaved similarly to the maximum resistance; the values for PEEP levels from 10cmH2O to 20cmH2O significantly differed from those for 0 and 5cmH2O PEEP (p < 0.05). Differential resistance showed the opposite variation to the maximum and minimum resistances. The only PEEP level that showed significant differences from 0 and 5cmH2O PEEP was 20cmH2O PEEP. Significant differences were also found between 15 and 5cmH2O PEEP (p < 0.05).
During protective ventilation in patients with acute respiratory distress syndrome, the maximum resistance of the respiratory system decreases with PEEP, reflecting the minimum resistance response, whereas differential resistance increases with PEEP.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):497-503
DOI 10.5935/0103-507X.20190087
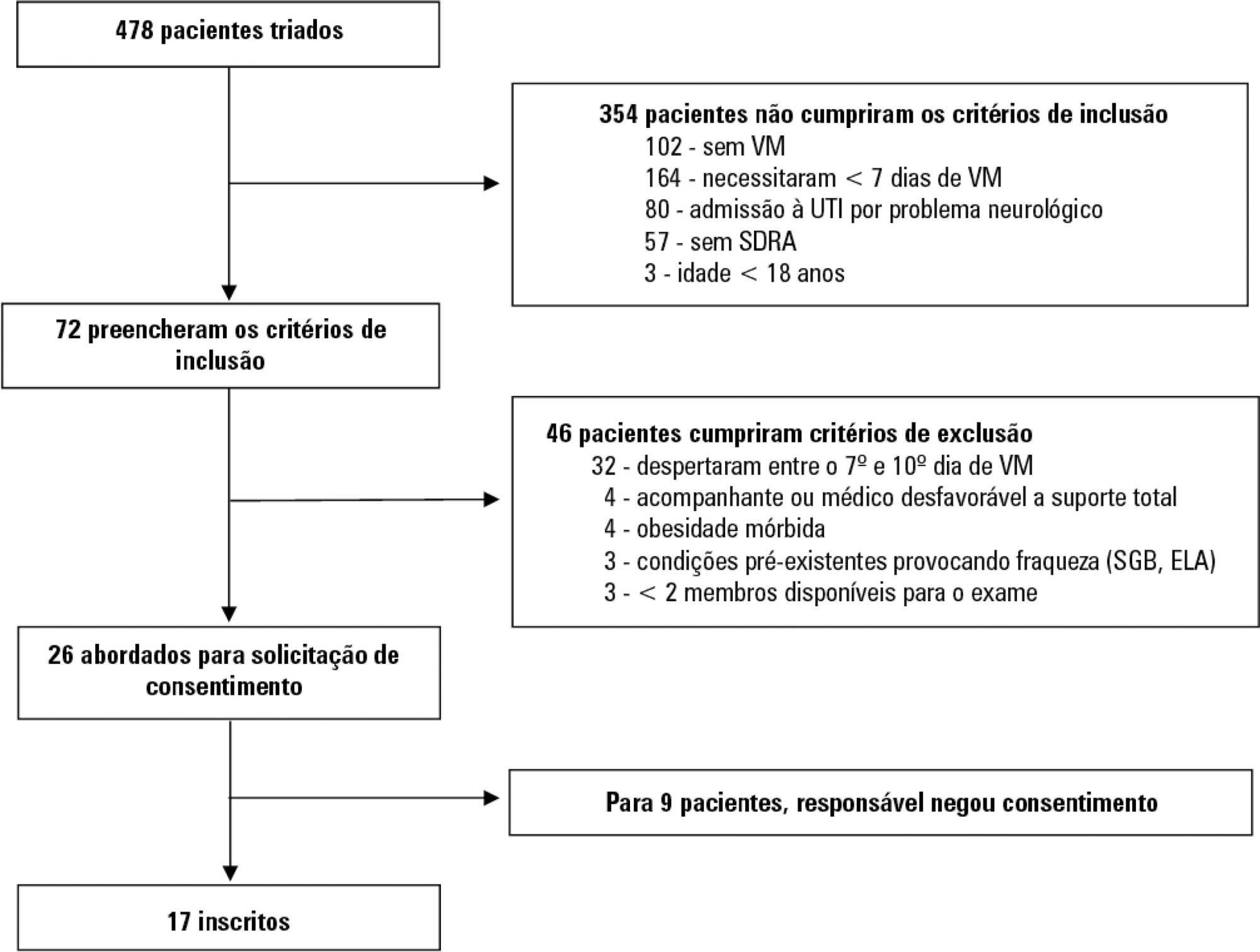
To evaluate whether electromyographical findings could predict intensive care unit mortality among mechanically ventilated septic patients under profound sedation.
A prospective cohort study that consecutively enrolled moderate-severe acute respiratory distress syndrome (partial pressure of oxygen/fraction of inspired oxygen < 200) patients who were ≥ 18 years of age, dependent on mechanical ventilation for ≥ 7 days, and under profound sedation (Richmond Agitation Sedation Scale ≤ -4) was conducted. Electromyographic studies of the limbs were performed in all patients between the 7th and the 10th day of mechanical ventilation. Sensory nerve action potentials were recorded from the median and sural nerves. The compound muscle action potentials were recorded from the median (abductor pollicis brevis muscle) and common peroneal (extensor digitorum brevis muscle) nerves.
Seventeen patients were enrolled during the seven months of the study. Nine patients (53%) had electromyographic signs of critical illness myopathy or neuropathy. The risk of death during the intensive care unit stay was increased in patients with electromyographical signs of critical illness myopathy or neuropathy in comparison to those without these diagnostics (77.7% versus 12.5%, log-rank p = 0.02).
Electromyographical signs of critical illness myopathy or neuropathy between the 7th and the 10th day of mechanical ventilation may be associated with intensive care unit mortality among moderate-severe acute respiratory distress syndrome patients under profound sedation, in whom clinical strength assessment is not possible.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):434-443
DOI 10.5935/0103-507X.20190084
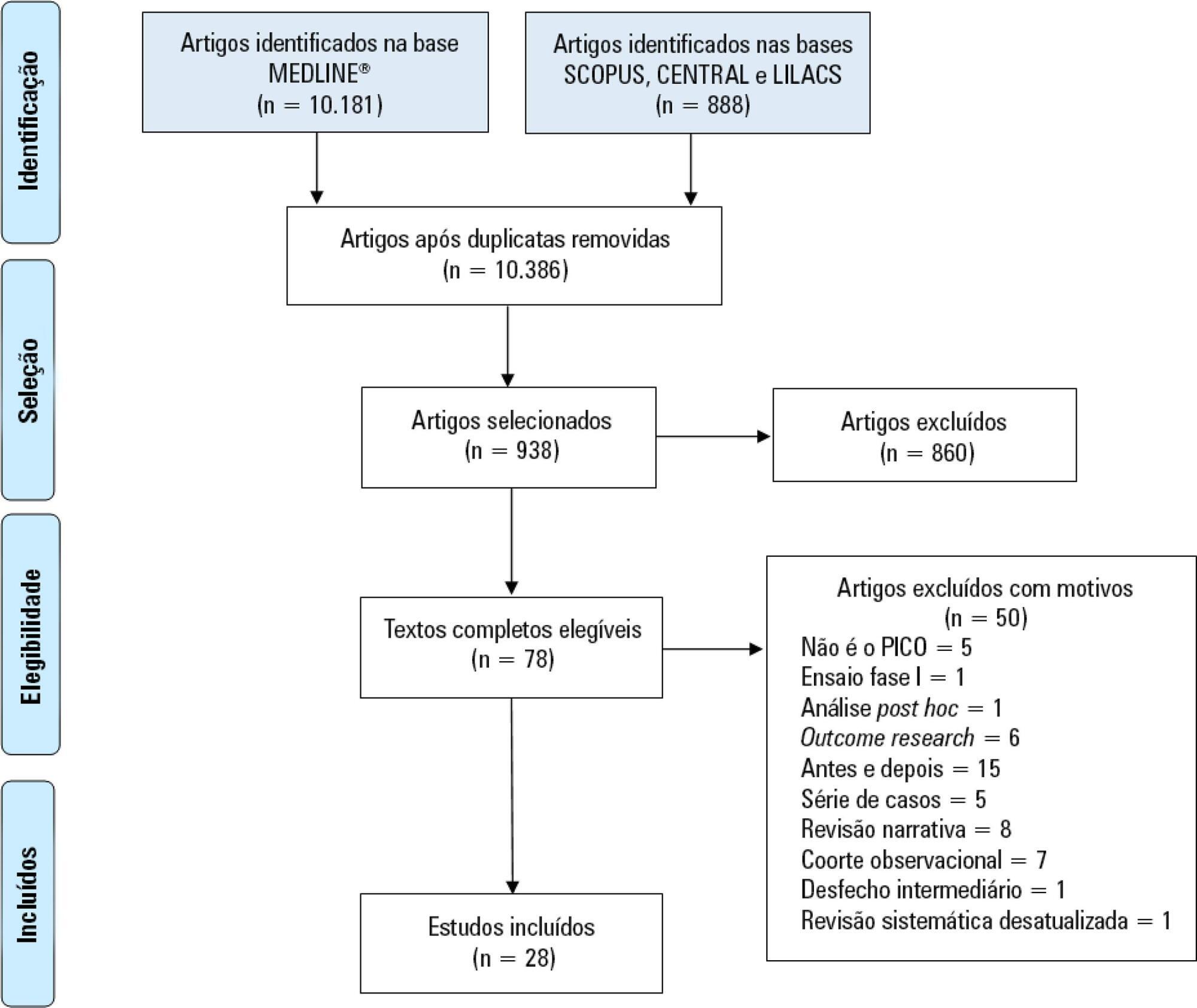
Immobility can cause several complications, including skeletal muscle atrophy and weakness, that influence the recovery of critically ill patients. This effect can be mitigated by early mobilization. Six key questions guided this research: Is early mobilization safe? Which patients are candidates for early mobilization? What are the contraindications? What is the appropriate dose, and how should it be defined? What results are obtained? What are the prognostic indicators for the use of early mobilization? The objective of this guideline was to produce a document that would provide evidence-based recommendations and suggestions regarding the early mobilization of critically ill adult patients, with the aim of improving understanding of the topic and making a positive impact on patient care. This guideline was based on a systematic review of articles conducted using the PICO search strategy, as recommended by the Guidelines Project of the Associação Médica Brasileira. Randomized clinical trials, prognostic cohort studies, and systematic reviews with or without meta-analysis were selected, and the evidence was classified according to the Oxford Center for Evidence-based Medicine Levels of Evidence. For all the questions addressed, enough evidence was found to support safe and well-defined early mobilization, with prognostic indicators that support and recommend the technique. Early mobilization is associated with better functional outcomes and should be performed whenever indicated. Early mobilization is safe and should be the goal of the entire multidisciplinary team.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):511-520
DOI 10.5935/0103-507X.20190088
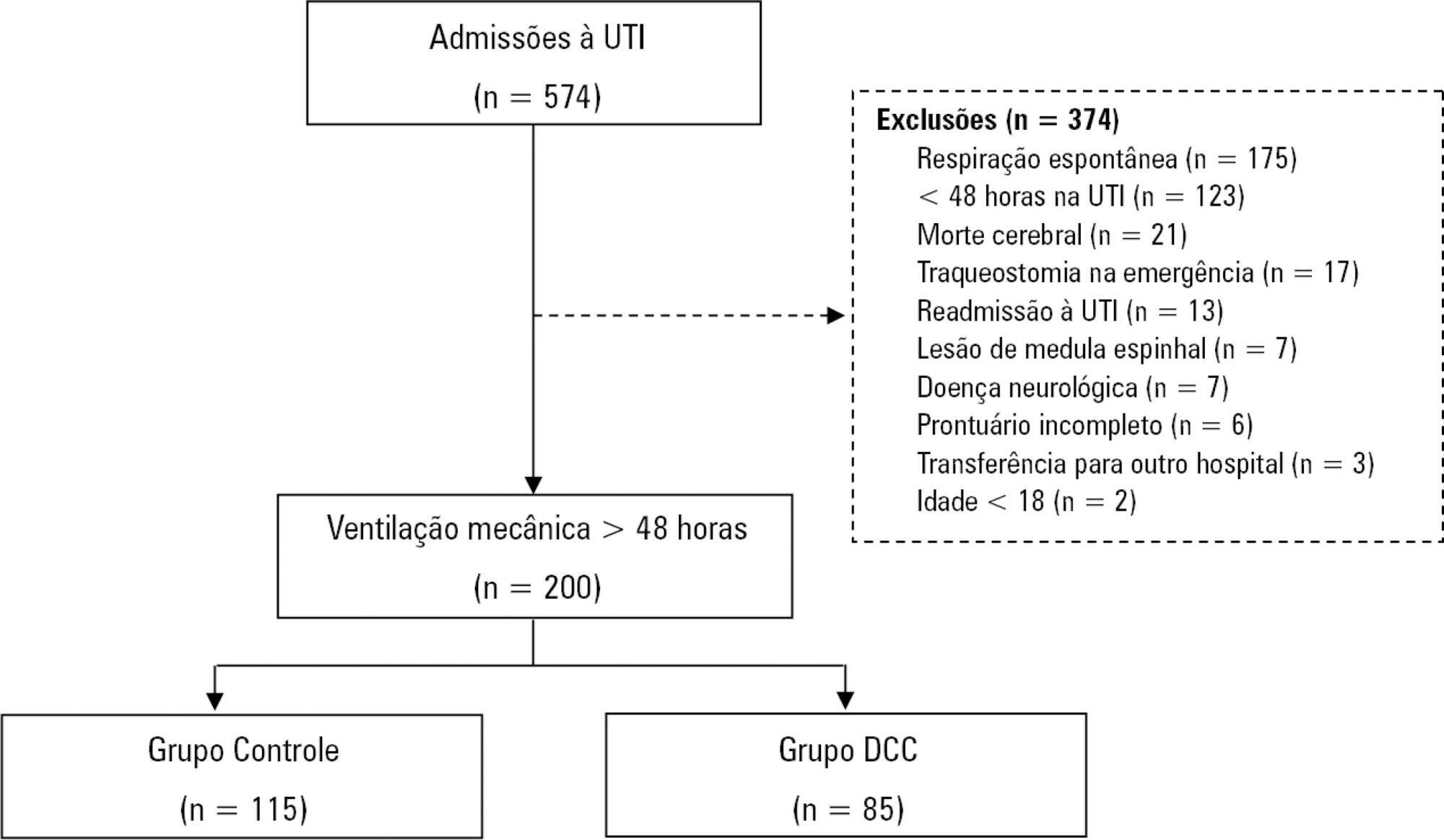
To characterize patients with chronic critical illness and identify predictors of development of chronic critical illness.
Prospective data was collected for 1 year in the intensive care unit of a general hospital in Southern Brazil. Three logistic regression models were constructed to identify factors associated with chronic critical illness.
Among the 574 subjects admitted to the intensive care unit, 200 were submitted to mechanical ventilation. Of these patients, 85 (43.5%) developed chronic critical illness, composing 14.8% of all the patients admitted to the intensive care unit. The regression model that evaluated the association of chronic critical illness with conditions present prior to intensive care unit admission identified chronic renal failure in patients undergoing hemodialysis (OR 3.57; p = 0.04) and a neurological diagnosis at hospital admission (OR 2.25; p = 0.008) as independent factors. In the model that evaluated the association of chronic critical illness with situations that occurred during intensive care unit stay, muscle weakness (OR 2.86; p = 0.01) and pressure ulcers (OR 9.54; p < 0.001) had the strongest associations. In the global multivariate analysis (that assessed previous factors and situations that occurred in the intensive care unit), hospital admission due to neurological diseases (OR 2.61; p = 0.03) and the development of pressure ulcers (OR 9.08; p < 0.001) had the strongest associations.
The incidence of chronic critical illness in this study was similar to that observed in other studies and had a strong association with the diagnosis of neurological diseases at hospital admission and chronic renal failure in patients undergoing hemodialysis, as well as complications developed during hospitalization, such as pressure ulcers and muscle weakness.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):289-295
DOI 10.5935/0103-507X.20190052
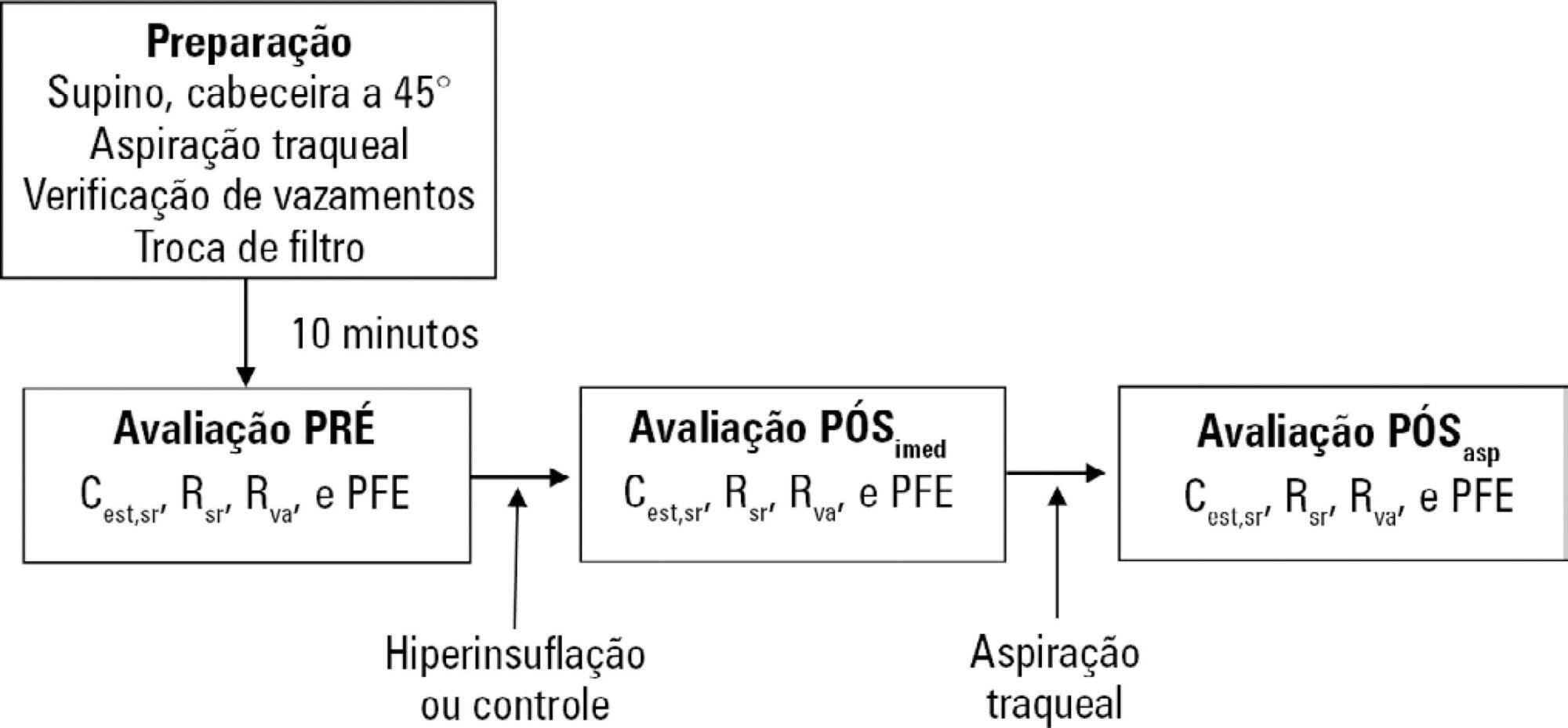
To evaluate the effects of ventilator hyperinflation on respiratory mechanics.
A randomized crossover clinical trial was conducted with 38 mechanically ventilated patients with pulmonary infection. The order of the hyperinflation and control (without changes in the parameters) conditions was randomized. Hyperinflation was performed for 5 minutes in pressure-controlled ventilation mode, with progressive increases of 5cmH2O until a maximum pressure of 35cmH2O was reached, maintaining positive end expiratory pressure. After 35cmH2O was reached, the inspiratory time and respiratory rate were adjusted so that the inspiratory and expiratory flows reached baseline levels. Measurements of static compliance, total resistance and airway resistance, and peak expiratory flow were evaluated before the technique, immediately after the technique and after aspiration. Two-way analysis of variance for repeated measures was used with Tukey's post hoc test, and p < 0.05 was considered significant.
Ventilator hyperinflation increased static compliance, which remained at the same level after aspiration (46.2 ± 14.8 versus 52.0 ± 14.9 versus 52.3 ± 16.0mL/cmH2O; p < 0.001). There was a transient increase in airway resistance (6.6 ± 3.6 versus 8.0 ± 5.5 versus 6.6 ± 3.5cmH2O/Ls-1; p < 0.001) and a transient reduction in peak expiratory flow (32.0 ± 16.0 versus 29.8 ± 14.8 versus 32.1 ± 15.3Lpm; p <0.05) immediately after the technique; these values returned to pretechnique levels after tracheal aspiration. There were no changes in the control condition, nor were hemodynamic alterations observed.
Ventilator hyperinflation promoted increased compliance associated with a transient increase in airway resistance and peak expiratory flow, with reduction after aspiration.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):361-367
DOI 10.5935/0103-507X.20190059
To compare the impact of two fast-track strategies regarding the extubation time and removal of invasive mechanical ventilation in adults after cardiac surgery on clinical and hospital outcomes.
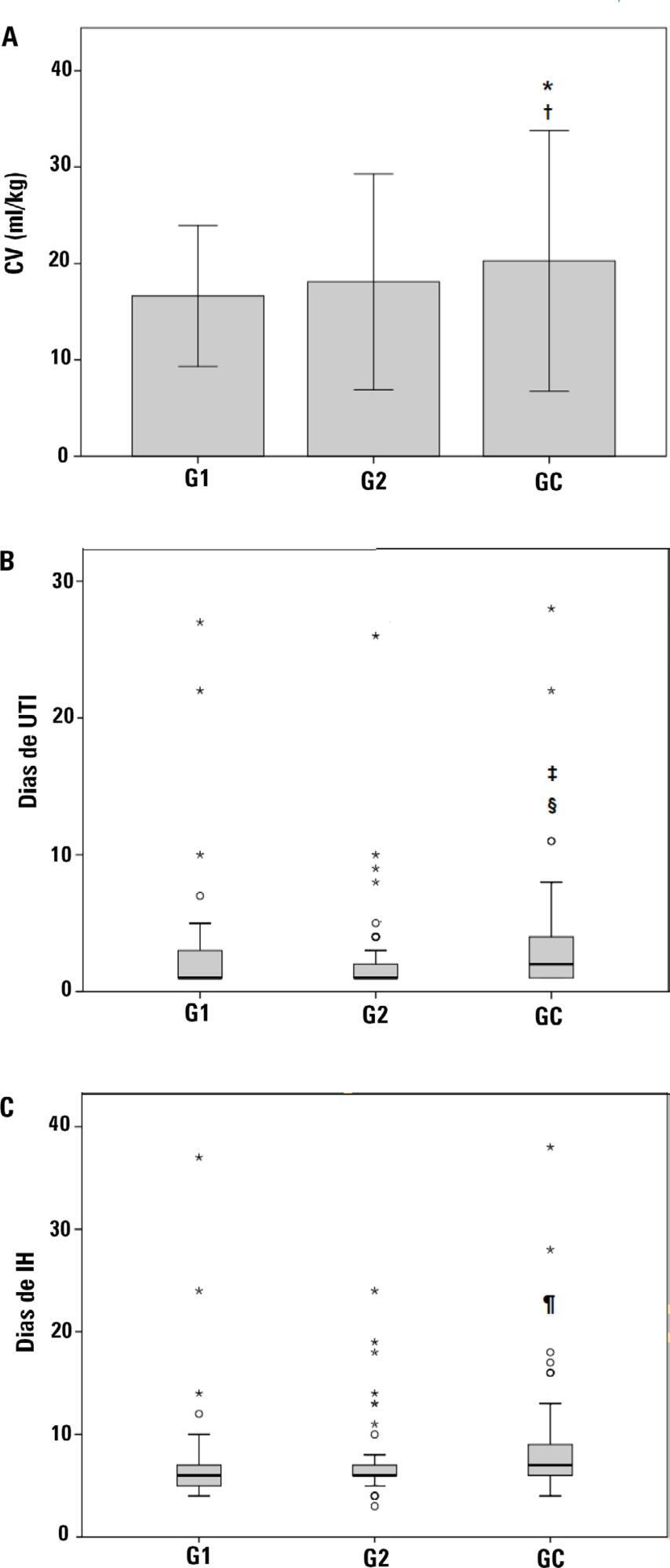
This was a retrospective cohort study with patients undergoing cardiac surgery. Patients were classified according to the extubation time as the Control Group (extubated 6 hours after admission to the intensive care unit, with a maximum mechanical ventilation time of 18 hours), Group 1 (extubated in the operating room after surgery) and Group 2 (extubated within 6 hours after admission to the intensive care unit). The primary outcomes analyzed were vital capacity on the first postoperative day, length of hospital stay, and length of stay in the intensive care unit. The secondary outcomes were reintubation, hospital-acquired pneumonia, sepsis, and death.
For the 223 patients evaluated, the vital capacity was lower in Groups 1 and 2 compared to the Control (p = 0.000 and p = 0.046, respectively). The length of stay in the intensive care unit was significantly lower in Groups 1 and 2 compared to the Control (p = 0.009 and p = 0.000, respectively), whereas the length of hospital stay was lower in Group 1 compared to the Control (p = 0.014). There was an association between extubation in the operating room (Group 1) with reintubation (p = 0.025) and postoperative complications (p = 0.038).
Patients undergoing fast-track management with extubation within 6 hours had shorter stays in the intensive care unit without increasing postoperative complications and death. Patients extubated in the operating room had a shorter hospital stay and a shorter stay in the intensive care unit but showed an increase in the frequency of reintubation and postoperative complications.