Abstract
Rev Bras Ter Intensiva. 2013;25(1):39-43
DOI 10.1590/S0103-507X2013000100008
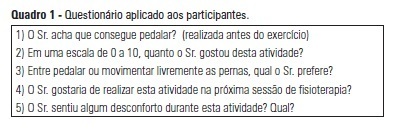
OBJECTIVE: The objective of this study was to use a cycle ergometer to assess cardiorespiratory changes during active exercise and to verify patients' satisfaction with this type of activity. METHODS: A single intervention involving active lower limb exercise was performed with a cycle ergometer (without load) for 5 minutes. The following variables were measured before, during and immediately after exercise: heart rate, blood pressure, respiratory rate, peripheral oxygen saturation and the Borg dyspnea scale score. Following the exercise, the patients answered a questionnaire to evaluate their satisfaction with this type of activity. RESULTS: A total of 38 patients (65% male) with a mean age of 48 ± 16 years old participated in the study. Enrolled patients presented a sequential organ failure assessment (SOFA) score of 2 (0 - 5 scale). During the exercise, 16% of the patients used ventilation support and 55% of them were breathing at room air. A comparison of the initial and final values of the variables indicated increases in the heart rate (92±17 beats/min vs. 95±18 beats/min; p<0.05), the respiratory rate (19 ± 8 breaths/min vs. 23±8 breaths/min; p<0.05) and the Borg dyspnea scale score (1.3±1.8 vs. 2.8±2.2; p<0.05). In addition, 85% of the patients reported enjoying the activity. Only 25% of the patients reported some discomfort, and 100% of the patients wanted to repeat this type of activity in future treatments. CONCLUSION: During the cycle ergometer exercises, minor cardiorespiratory changes were observed in the patients. The evaluated patients reported high satisfaction with this type of activity.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):341-346
DOI 10.1590/S0103-507X2012000400008
OBJECTIVE: To examine the reliability of the SF-36 general health questionnaire when used to evaluate the health status of critically ill patients before admission to intensive care and to measure their health-related quality of life prior to admission and its relation to severity of illness and length of stay in the intensive care unit. METHODS: Prospective cohort study conducted in the intensive care unit of a public teaching hospital. Over three months, communicative and oriented patients were interviewed within the first 72 hours of intensive care unit admission; 91 individuals participated. The APACHE II score was used to assess severity of illness, and the SF-36 questionnaire was used to measure health-related quality of life. RESULTS: The reliability of SF-36 was verified in all dimensions using Cronbach's alpha coefficient. In six dimensions of eight domains the value exceeded 0.70. The average SF-36 scores of the health-related quality of life dimensions for the patients before admission to intensive care unit were 57.8 for physical functioning, 32.4 for role-physical, 53.0 for bodily pain, 63.2 for general health, 50.6 for vitality, 56.2 for social functioning, 54.6 for role-emotional and 60.3 for mental health. The correlations between severity of illness and length of stay and the health-related quality of life scores were very low, ranging from -0.152 to 0.175 and -0.158 to 0.152, respectively, which were not statistically significant. CONCLUSION: In the sample studied, the SF-36 demonstrated good reliability when used to measure health-related quality of life in critically ill patients before admission to the intensive care unit. The worst score was role-physical and the best was general health. Health-related quality of life of patients before admission was not correlated with severity of illness or length of stay in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2012;24(4):369-374
DOI 10.1590/S0103-507X2012000400013
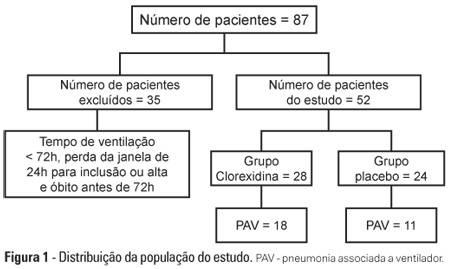
OBJECTIVE: To evaluate the effects of oral chlorhexidine hygiene with toothbrushing on the rate of ventilator-associated pneumonia in a mixed population of critically ill patients under prolonged mechanical ventilation. METHODS: Prospective, randomized, and placebo-controlled pilot study. Patients who were receiving mechanical ventilation, had been admitted less than 24 hours prior, and were anticipated to require mechanical ventilation for more than 72 hours were included in the study. The patients were randomly divided into one of the following groups: chlorhexidine hygiene with toothbrushing or a placebo group (gel with the same color and consistency and toothbrushing). RESULTS: The planned interim analysis was conducted using 52 patients, and the study was terminated prematurely. In total, 28 patients were included in the chlorhexidine / toothbrushing group, and 24 patients were included in the placebo group. Ventilator-associated pneumonia occurred in 45.8% of the placebo group and in 64.3% of the chlorhexidine hygiene with toothbrushing group (RR=1.4; 95% CI=0.83-2.34; p=0.29). CONCLUSION: Because the study was terminated due to futility, it was not possible to evaluate the impact of oral hygiene using 2% chlorhexidine and toothbrushing on the incidence of ventilator-associated pneumonia in this heterogeneous population of critical patients receiving long-term mechanical ventilation, and no beneficial effect was observed for this intervention.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):188-196
DOI 10.5935/0103-507X.20130034
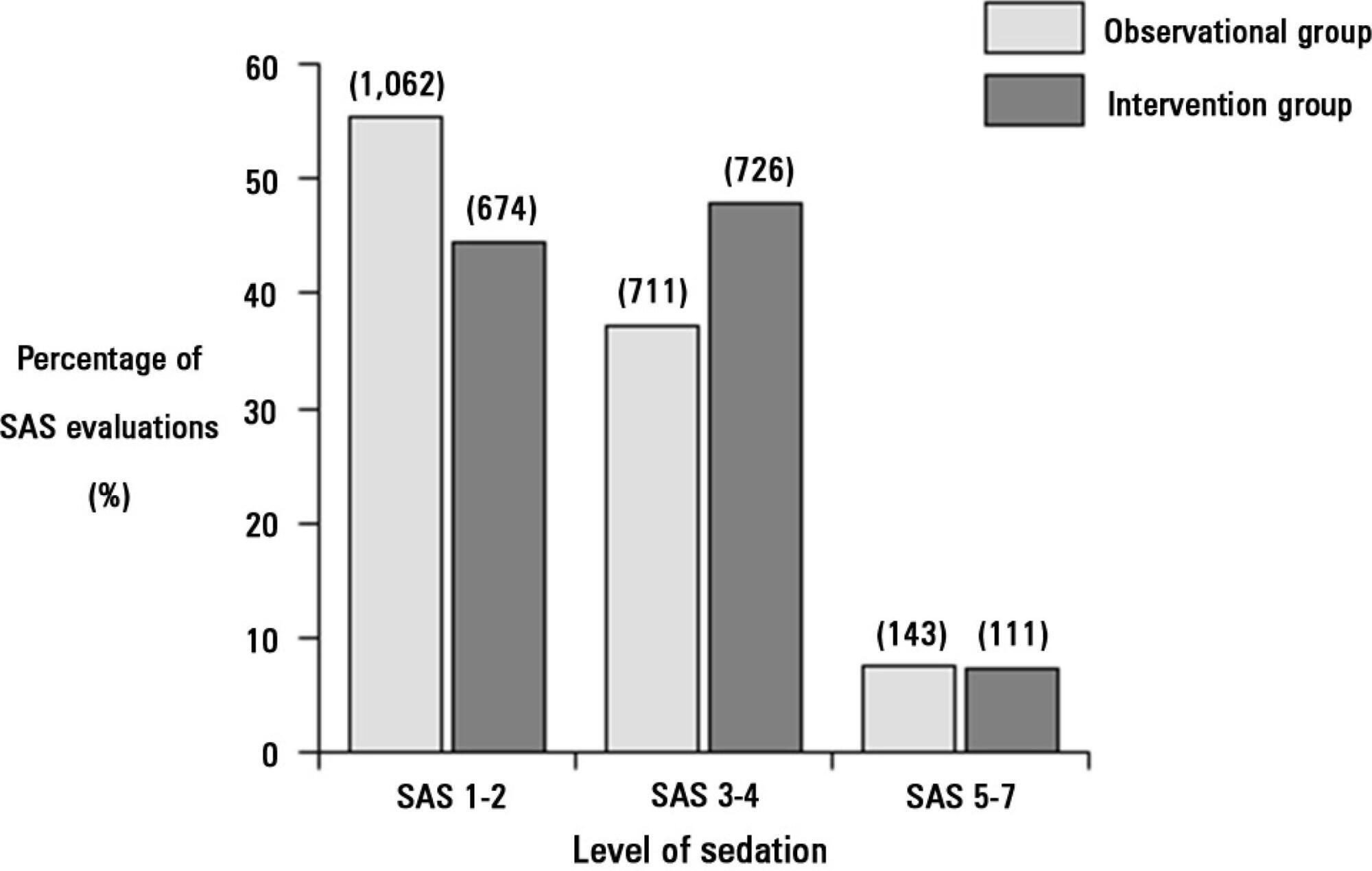
Deep sedation in critically ill patients is associated with a longer duration of mechanical ventilation and a prolonged length of stay in the intensive care unit. Several protocols have been used to improve these outcomes. We implement and evaluate an analgesia-based, goal-directed, nurse-driven sedation protocol used to treat critically ill patients who receive mechanical ventilation.
We performed a prospective, two-phase (before-after), non-randomized multicenter study that involved 13 intensive care units in Chile. After an observational phase (observational group, n=155), we designed, implemented and evaluated an analgesia-based, goal-directed, nurse-driven sedation protocol (intervention group, n=132) to treat patients who required mechanical ventilation for more than 48 hours. The primary outcome was to achieve ventilator-free days by day 28.
The proportion of patients in deep sedation or in a coma decreased from 55.2% to 44.0% in the interventional group. Agitation did not change between the periods and remained approximately 7%. Ventilator-free days to day 28, length of stay in the intensive care unit and mortality were similar in both groups. At one year, post-traumatic stress disorder symptoms in survivors were similar in both groups.
We designed and implemented an analgesia-based, goal-directed, nurse-driven sedation protocol in Chile. Although there was no improvement in major outcomes, we observed that the present protocol was safe and feasible and that it resulted in decreased periods of deep sedation without increasing agitation.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):212-217
DOI 10.5935/0103-507X.20130037
To investigate the association between the rapid shallow breathing index and successful extubation in patients with traumatic brain injury.
This study was a prospective study conducted in patients with traumatic brain injury of both genders who underwent mechanical ventilation for at least two days and who passed a spontaneous breathing trial. The minute volume and respiratory rate were measured using a ventilometer, and the data were used to calculate the rapid shallow breathing index (respiratory rate/tidal volume). The dependent variable was the extubation outcome: reintubation after up to 48 hours (extubation failure) or not (extubation success). The independent variable was the rapid shallow breathing index measured after a successful spontaneous breathing trial.
The sample comprised 119 individuals, including 111 (93.3%) males. The average age of the sample was 35.0±12.9 years old. The average duration of mechanical ventilation was 8.1±3.6 days. A total of 104 (87.4%) participants achieved successful extubation. No association was found between the rapid shallow breathing index and extubation success.
The rapid shallow breathing index was not associated with successful extubation in patients with traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):225-232
DOI 10.5935/0103-507X.20130039
This study sought to compare patients at public and private intensive care units according to the nursing workload and interventions provided.
This retrospective, comparative cohort study included 600 patients admitted to 4 intensive care units in São Paulo. The nursing workload and interventions were assessed using the Nursing Activities Score during the first and last 24 hours of the patient's stay at the intensive care unit. Pearson's chi-square test, Fisher's exact test, the Mann-Whitney test, and Student's t test were used to compare the patient groups.
The average Nursing Activities Score upon admission to the intensive care unit was 61.9, with a score of 52.8 upon discharge. Significant differences were found among the patients at public and private intensive care units relative to the average Nursing Activities Score upon admission, as well as for 12 out of 23 nursing interventions performed during the first 24 hours of stay at the intensive care units. The patients at the public intensive care units exhibited a higher average score and overall more frequent nursing interventions, with the exception of those involved in the "care of drains", "mobilization and positioning", and "intravenous hyperalimentation". The groups also differed with regard to the evolution of the Nursing Activities Score among the total case series as well as the groups of survivors from the time of admission to discharge from the intensive care unit.
Patients admitted to public and private intensive care units exhibit differences in their nursing care demands, which may help managers with nursing manpower planning.
Abstract
Rev Bras Ter Intensiva. 2013;25(4):290-296
DOI 10.5935/0103-507X.20130050
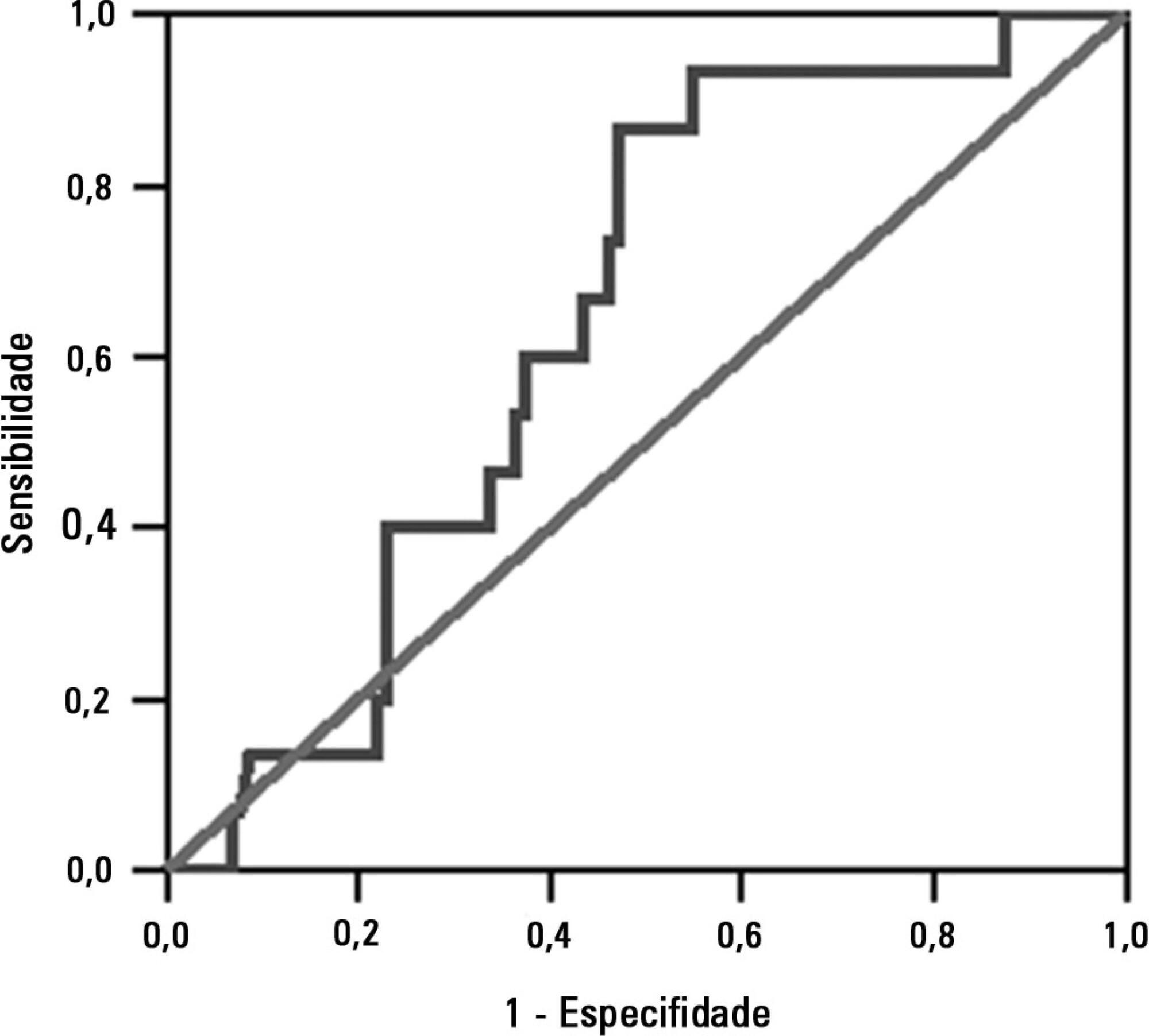
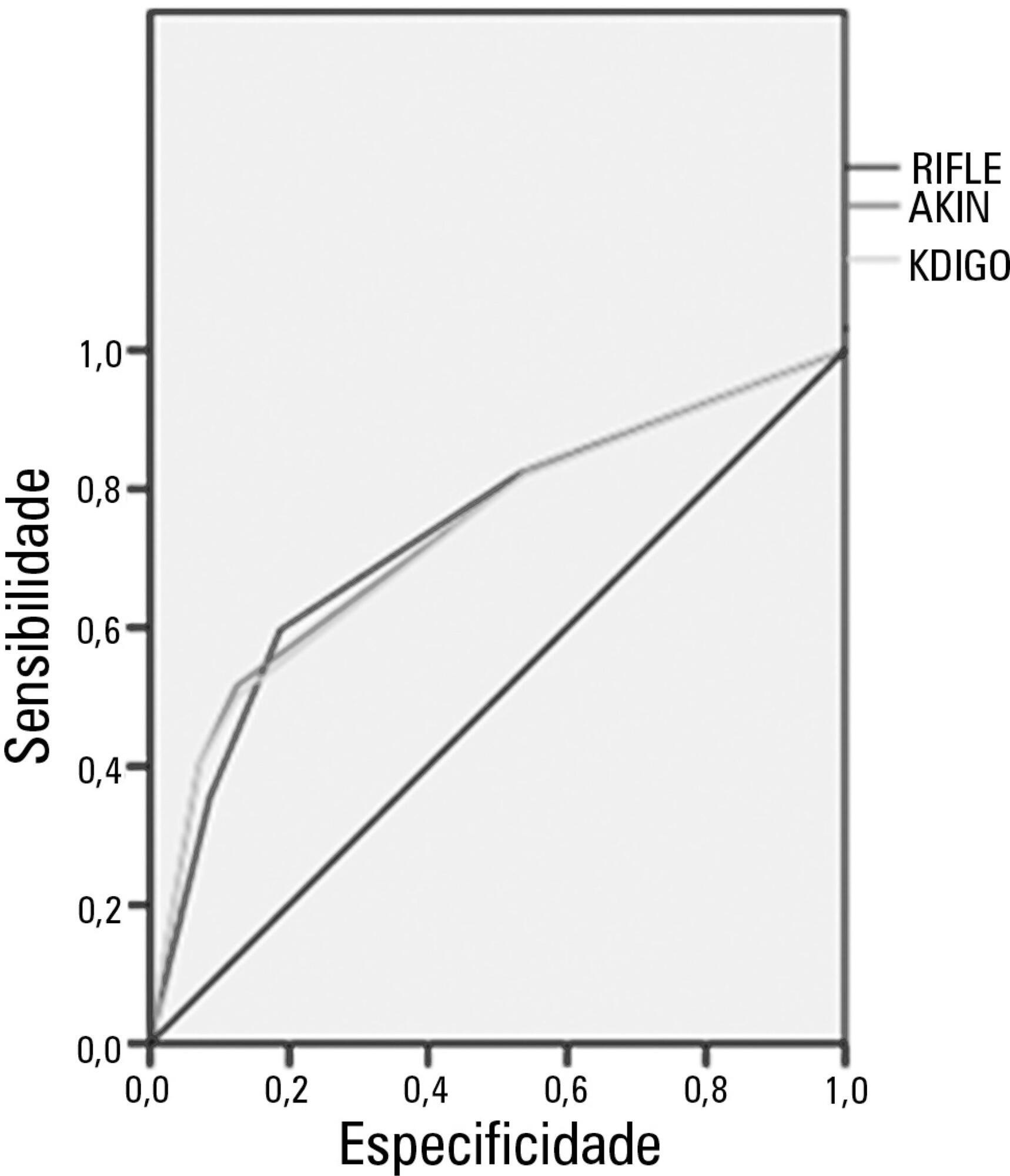
Acute kidney injury is a common complication in critically ill patients, and the RIFLE, AKIN and KDIGO criteria are used to classify these patients. The present study's aim was to compare these criteria as predictors of mortality in critically ill patients.
Prospective cohort study using medical records as the source of data. All patients admitted to the intensive care unit were included. The exclusion criteria were hospitalization for less than 24 hours and death. Patients were followed until discharge or death. Student's t test, chi-squared analysis, a multivariate logistic regression and ROC curves were used for the data analysis.
The mean patient age was 64 years old, and the majority of patients were women of African descent. According to RIFLE, the mortality rates were 17.74%, 22.58%, 24.19% and 35.48% for patients without acute kidney injury (AKI) in stages of Risk, Injury and Failure, respectively. For AKIN, the mortality rates were 17.74%, 29.03%, 12.90% and 40.32% for patients without AKI and at stage I, stage II and stage III, respectively. For KDIGO 2012, the mortality rates were 17.74%, 29.03%, 11.29% and 41.94% for patients without AKI and at stage I, stage II and stage III, respectively. All three classification systems showed similar ROC curves for mortality.
The RIFLE, AKIN and KDIGO criteria were good tools for predicting mortality in critically ill patients with no significant difference between them.
Abstract
Rev Bras Ter Intensiva. 2012;24(3):263-269
DOI 10.1590/S0103-507X2012000300010
OBJECTIVE: This study evaluated the relationship between nutritional intake and protein and caloric requirements and observed clinical outcomes on the 7th day of intensive care unit stay. METHODS: This was a retrospective cohort study of 126 patients who were admitted to the intensive care unit for >7 days. The patients were categorized according to the adequacy of energy and protein intake in relation to requirements (a >60% Adequate Intake Group and a <60% Inadequate Intake Group). The length of stay, ventilator free time and mortality in the intensive care unit and hospital were evaluated. RESULTS: Enteral nutrition was used in 95.6% of the 126 included patients, and nutrition was initiated 41 hours after admission to the intensive care unit. The adequacy of intake was 84% for energy and 72.5% for protein. No differences in the length of stay [16 (11-23) versus 15 (11-21) days, p=0.862], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.985] or mortality in the intensive care unit [12 (41.4%) versus 38 (39.1%), p=0.831] and hospital [15 (51.7%) versus 44 (45.4%), p=0.348] were observed between the adequate and inadequate energy intake groups, respectively. Similar results in protein intake and the length of hospital stay [15 (12-21) versus 15 (11-21) days, p=0.996], ventilator free time [2 (0-7) versus 3 (0-6) days, p=0.846], and mortality in the intensive care unit [15 (28.3%) versus 35 (47.9%), p=0.536)] and hospital [18 (52.9%) versus 41 (44.6%), p=0.262] were observed between groups. CONCLUSION: The results did not establish that energy and protein intakes of greater or less than 60% of nutritional requirements were reliable dividers of clinical outcomes.