Abstract
Rev Bras Ter Intensiva. 2014;26(3):299-304
DOI 10.5935/0103-507X.20140042
To assess the opinions and practices of intensive care professionals with regard to diarrhea in critically ill patients.
A multicenter cross-sectional study was conducted among health care professionals working at three adult intensive care units. Participants responded individually to a self-administered questionnaire about their length of work experience in intensive care; the definition, characterization, and causes of diarrhea; types of records in the patient's medical record; and training received.
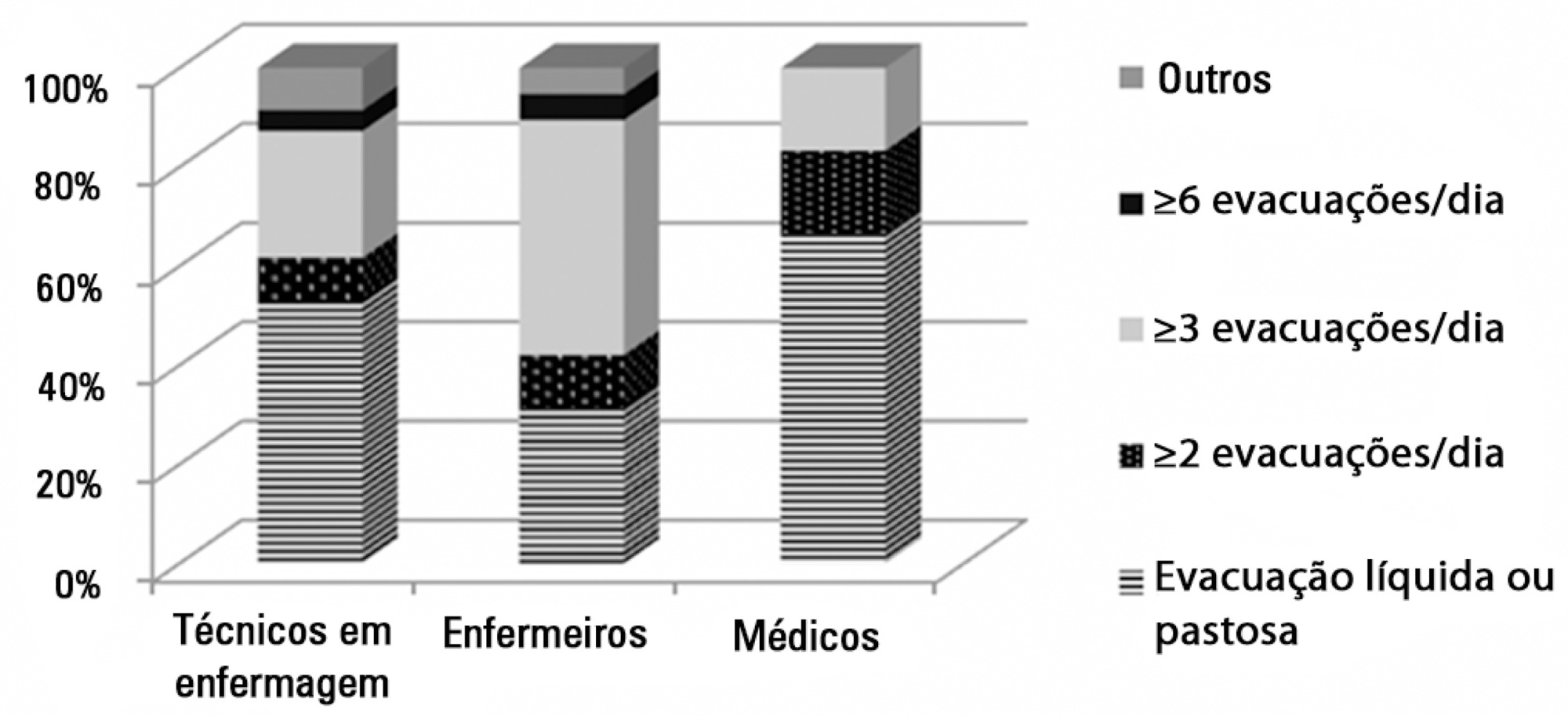
A total of 78 professionals participated in this study, of whom 59.0% were nurse technicians, 25.7% were nurses, and 15.3% were physicians; 77.0% of them had worked in intensive care for over 1 year. Only 37.2% had received training on this topic. Half of the interviewees defined diarrhea as "liquid and/or pasty stools" regardless of frequency, while the other 50.0% defined diarrhea based on the increased number of daily bowel movements. The majority of them mentioned diet as the main cause of diarrhea, followed by "use of medications" (p<0.001). Distinct nutritional practices were observed among the analyzed professionals regarding episodes of diarrhea, such as discontinuing, maintaining, or reducing the volume of enteral nutrition; physicians reported that they do not routinely communicate the problem to other professionals (for example, to a nutritionist) and do not routinely record and quantify diarrhea events in patients' medical records.
Different opinions and practices were observed in intensive care professionals with regard to diarrhea.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):87-92
DOI 10.5935/0103-507X.20130018
OBJECTIVES: To evaluate the incidence of constipation in critical patients on enteral nutrition in a hospital intensive care unit and to correlate this incidence with the variables found for critical patients. METHODS: The present investigation was a retrospective analytical study conducted in the intensive care unit of Hospital Regional da Asa Norte (DF) via the analysis of medical records of patients admitted during the period from January to December 2011. Data on the incidence of constipation and enteral nutritional support, gastrointestinal changes, stool frequency, ventilatory support, and outcomes were collected and analyzed. RESULTS: The initial sample consisted of 127 patients admitted to the unit during the period from January to December 2011. Eighty-four patients were excluded, and the final sample consisted of 43 patients. The incidence of constipation, defined as no bowel movement during the first 4 days of hospitalization, was 72% (n=31). The patients were divided into a control group and a constipated group. The group of constipated patients reached the caloric target, on average, at 6.5 days, and the control group reached the caloric target in 5.6 days (p=0.51). Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization. There was an association between evacuation during hospitalization and a longer duration of hospitalization for a subgroup of patients who did not evacuate during the entire period (p=0.009). CONCLUSION: The incidence of constipation in the unit studied was 72%. Only the absence of evacuation during hospitalization was associated with longer hospital stays. Constipation was not associated with the length of hospital stay, suspension of nutritional support, or outcome of hospitalization.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):93-98
DOI 10.5935/0103-507X.20130019
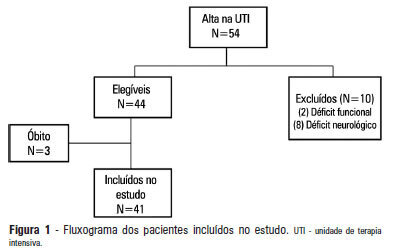
OBJECTIVE: 1) To evaluate the functional independence measures immediately after discharge from an intensive care unit and to compare these values with the FIMs 30 days after that period. 2) To evaluate the possible associated risk factors. METHODS: The present investigation was a prospective cohort study that included individuals who were discharged from the intensive care unit and underwent physiotherapy in the unit. Functional independence was evaluated using the functional independence measure immediately upon discharge from the intensive care unit and 30 days thereafter via a phone call. The patients were admitted to the Hospital Santa Clara intensive care unit during the period from May 2011 to August 2011. RESULTS: During the predetermined period of data collection, 44 patients met the criteria for inclusion in the study. The mean age of the patients was 55.4±10.5 years. Twenty-seven of the subjects were female, and 15 patients were admitted due to pulmonary disease. The patients exhibited an functional independence measure of 84.1±24.2. When this measure was compared to the measure at 30 days after discharge, there was improvement across the functional independence variables except for that concerned with sphincter control. There were no significant differences when comparing the gender, age, clinical diagnosis, length of stay in the intensive care unit, duration of mechanical ventilation, and the presence of sepsis during this period. CONCLUSION: Functional independence, as evaluated by the functional independence measure scale, was improved at 30 days after discharge from the intensive care unit, but it was not possible to define the potentially related factors.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):115-122
DOI 10.5935/0103-507X.20130022
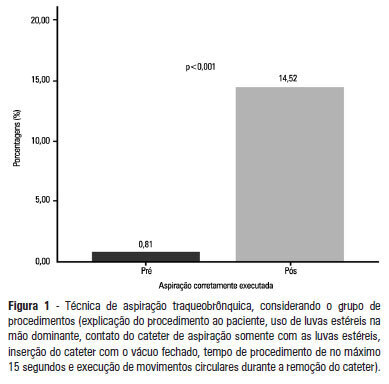
OBJECTIVE: To evaluate the effectiveness of an educational intervention on healthcare professionals' adherence to the technical recommendations for tracheobronchial aspiration in intensive care unit patients. METHODS: A quasi-experimental study was performed to evaluate intensive care unit professionals' adherence to the tracheobronchial aspiration technical recommendations in intensive care unit patients both before and after a theoretical and practical educational intervention. Comparisons were performed using the chi-square test, and the significance level was set to p<0.05. RESULTS: A total of 124 procedures, pre- and post-intervention, were observed. Increased adherence was observed in the following actions: the use of personal protective equipment (p=0.01); precaution when opening the catheter package (p<0.001); the use of a sterile glove on the dominant hand to remove the catheter (p=0.003); the contact of the sterile glove with the catheter only (p<0.001); the execution of circular movements during the catheter removal (p<0.001); wrapping the catheter in the sterile glove at the end of the procedure (p=0.003); the use of distilled water, opened at the start of the procedure, to wash the connection latex (p=0.002); the disposal of the leftover distilled water at the end of the procedure (p<0.001); and the performance of the aspiration technique procedures (p<0.001). CONCLUSION: There was a low adherence by health professionals to the preventive measures against hospital infection, indicating the need to implement educational strategies. The educational intervention used was shown to be effective in increasing adherence to the technical recommendations for tracheobronchial aspiration.
Abstract
Rev Bras Ter Intensiva. 2013;25(2):148-154
DOI 10.5935/0103-507X.20130026
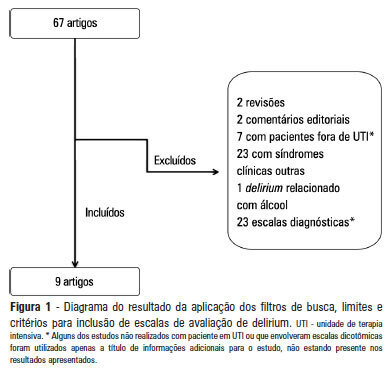
OBJECTIVE: To identify scales that can establish a quantitative assessment of delirium symptoms in critically ill patients through a systematic review. METHODS: Studies that evaluated delirium stratification scales in patients hospitalized in intensive care units were selected in a search performed in the MedLine database. Validation studies of these scales and their target patient populations were analyzed, and we identified the examiner and the signs and symptoms evaluated. In addition, the duration of the application and the sensitivity and specificity of each scale were assessed. RESULTS: Six scales were identified: the Delirium Detection Score, the Cognitive Test of Delirium, the Memorial Delirium Assessment Scale, the Intensive Care Delirium Screening Checklist, The Neelon and Champagne Confusion Scale and the Delirium Rating Scale-Revised-98. CONCLUSION: The scales identified allow the stratification and monitoring of critically ill patients with delirium. Among the six scales, the most studied and best suited for use in the intensive care units was the Intensive Care Delirium Screening
Abstract
Rev Bras Ter Intensiva. 2013;25(1):17-24
DOI 10.1590/S0103-507X2013000100005
OBJECTIVE: Evaluate the compliance of septic patients' nutritional management with enteral nutrition guidelines for critically ill patients. METHODS: Prospective cohort study with 92 septic patients, age ≥18 years, hospitalized in an intensive care unit, under enteral nutrition, evaluated according to enteral nutrition guidelines for critically ill patients, compliance with caloric and protein goals, and reasons for not starting enteral nutrition early or for discontinuing it. Prognostic scores, length of intensive care unit stay, clinical progression, and nutritional status were also analyzed. RESULTS: The patients had a mean age of 63.4±15.1 years, were predominantly male, were diagnosed predominantly with septic shock (56.5%), had a mean intensive care unit stay of 11 (7.2 to 18.0) days, had 8.2±4.2 SOFA and 24.1±9.6 APACHE II scores, and had 39.1% mortality. Enteral nutrition was initiated early in 63% of patients. Approximately 50% met the caloric and protein goals on the third day of intensive care unit stay, a percentage that decreased to 30% at day 7. Reasons for the late start of enteral nutrition included gastrointestinal tract complications (35.3%) and hemodynamic instability (32.3%). Clinical procedures were the most frequent reason to discontinue enteral nutrition (44.1%). There was no association between compliance with the guidelines and nutritional status, length of intensive care unit stay, severity, or progression. CONCLUSION: Although the number of septic patients under early enteral nutrition was significant, caloric and protein goals at day 3 of intensive care unit stay were met by only half of them, a percentage that decreased at day 7.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):25-31
DOI 10.1590/S0103-507X2013000100006
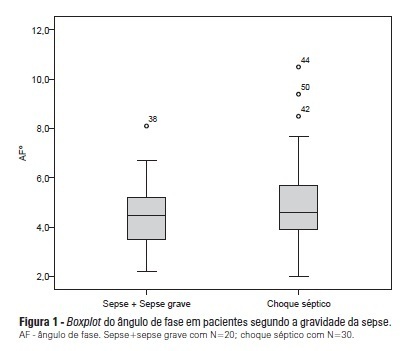
OBJECTIVE: To calculate the values of the phase angle of septic patients using bioelectrical impedance analysis, correlate the values with clinical and biochemical variables, and compare them to reference values. METHODS: Cohort study conducted with 50 septic patients aged ≥18 years old, admitted to intensive care units, and assessed according to prognostic indexes (APACHE II and SOFA), clinical progression (mortality, severity of sepsis, length of stay in intensive care unit), biochemical parameters (albumin and C-reactive protein), and the phase angle. RESULTS: The average age of the sample was 65.6±16.5 years. Most patients were male (58%) and suffering from septic shock (60%). The average APACHE II and SOFA scores were 22.98±7.1 and 7.5±3.4, respectively. The patients who survived stayed nine days on average (five to 13) in the intensive care unit, and the mortality rate was 30%. The average value of the phase angle was 5.4±2.6° in the total sample and was smaller among the females compared with the males (p=0.01). The phase angle measures did not exhibit an association with the severity of the sepsis, mortality, gender, and age or correlate with the length of hospitalization or the biochemical parameters. The participants' phase angle values adjusted per gender and age were 1.1 to 1.9 times lower compared with the values for a normal population. CONCLUSION: The average value of the phase angle of septic patients was lower compared with the reference values for a healthy population. The phase angle measures did not exhibit association with the clinical and biochemical variables, which might be explained by the sample homogeneity.
Abstract
Rev Bras Ter Intensiva. 2013;25(1):32-38
DOI 10.1590/S0103-507X2013000100007
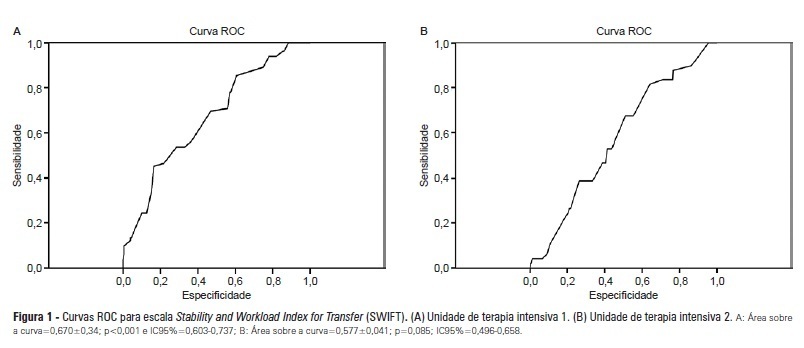
OBJECTIVES: Identify patients at risk for intensive care unit readmission, the reasons for and rates of readmission, and mortality after their stay in the intensive care unit; describe the sensitivity and specificity of the Stability and Workload Index for Transfer scale as a criterion for discharge from the intensive care unit. METHODS: Adult, critical patients from intensive care units from two public hospitals in Porto Alegre, Brazil, comprised the sample. The patients' clinical and demographic characteristics were collected within 24 hours of admission. They were monitored until their final outcome on the intensive care unit (death or discharge) to apply the Stability and Workload Index for Transfer. The deaths during the first intensive care unit admission were disregarded, and we continued monitoring the other patients using the hospitals' electronic systems to identify the discharges, deaths, and readmissions. RESULTS: Readmission rates were 13.7% in intensive care unit 1 (medical-surgical, ICU1) and 9.3% in intensive care unit 2 (trauma and neurosurgery, ICU2). The death rate following discharge was 12.5% from ICU1 and 4.2% from ICU2. There was a statistically significant difference in Stability and Workload Index for Transfer (p<0.05) regarding the ICU1 patients' outcome, which was not found in the ICU2 patients. In ICU1, 46.5% (N=20) of patients were readmitted very early (within 48 hours of discharge). Mortality was high among those readmitted: 69.7% in ICU1 and 48.5% in ICU2. CONCLUSIONS: The Stability and Workload Index for Transfer scale showed greater efficacy in identifying patients more prone to readmission and death following discharge from a medical-surgical intensive care unit. The patients' intensive care unit readmission during the same hospitalization resulted in increased morbidity, mortality, length of stay, and total costs.