Abstract
Rev Bras Ter Intensiva. 2012;24(2):143-150
DOI 10.1590/S0103-507X2012000200008
OBJECTIVE: To determine the prevalence of infections in Brazilian intensive care units and the associated mortality by analyzing the data obtained in the Extended Prevalence of Infection in Intensive Care (EPIC II) study. METHODS: EPIC II was a multicenter, international, cross-sectional prospective study of infection prevalence. It described the demographic, physiological, bacteriological, and therapeutic characteristics, outcome up to the 60th day, prevalence of infection, and mortality of all the patients admitted to the participating ICUs between zero hour and midnight on May 8, 2007. A total of 14,414 patients were included in the original study. Of these 14,414 patients, 1,235 were Brazilian and were hospitalized in 90 Brazilian ICUs. They represent the focus of this study. RESULTS: Among these 1,235 Brazilian patients, 61,6% had an infection on the day of the trial, and the lungs were the main site of infection (71.2%). Half of the patients had positive cultures, predominantly gram-negative bacilli (72%). On the day of the study, the median SOFA score was 5 (3-8) and the median SAPS II score was 36 (26-47). The infected patients had SOFA scores significantly higher than those of the non-infected patients 6 (4-9) and 3 (2-6), respectively). The overall ICU mortality rate was 28.4%: 37.6% in the infected patients, and 13.2% in the non-infected patients (p<0.001). Similarly, the in-hospital mortality rate was 34.2%, with a higher rate in the infected than in the non-infected patients (44.2% vs. 17.7%) (p<0.001). In the multivariate analysis, the main factors associated with infection incidence were emergency surgery (OR 2.89, 95%CI [1.72-4.86], p<0.001), mechanical ventilation (OR 2.06, 95% CI [1.5-2.82], p<0.001), and the SAPS II score (OR 1.04, 95% CI [1.03-1.06], p<0.001). The main factors related to mortality were ICC functional class III/ IV (OR 3.0, 95% CI [1.51-5.98], p<0.01), diabetes mellitus (OR 0.48, 95% CI [0.25-0.95], p<0.03), cirrhosis (OR 4.62, 95% CI [1.47-14,5], p<0.01), male gender (OR 0.68, 95% CI [0.46-1.0], p<0.05), mechanical ventilation (OR 1.87, 95% CI [1.19-2.95], p<0.01), hemodialysis (OR 1.98, 95% CI [1.05-3.75], p<0.03), and the SAPS II score (OR 1.08, 95% CI [1.06-1.10], p<0.001). CONCLUSION: The present study revealed a higher prevalence of infections in Brazilian ICUs than has been previously reported. There was a clear association between infection and mortality.
Abstract
Rev Bras Ter Intensiva. 2012;24(2):173-178
DOI 10.1590/S0103-507X2012000200013
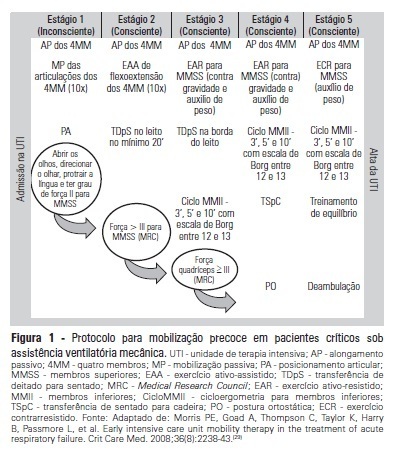
OBJECTIVE:To evaluate the effects of an early mobilization protocol on respiratory and peripheral muscles in critically ill patients. METHODS: A randomized controlled clinical trial was conducted with 59 male and female patients on mechanical ventilation. The patients were divided into a conventional physical therapy group (control group, n=14) that received the sector's standard physical therapy program and an early mobilization group (n=14) that received a systematic early mobilization protocol. Peripheral muscle strength was assessed with the Medical Research Council score, and respiratory muscle strength (determined by the maximal inspiratory and expiratory pressures) was measured using a vacuum manometer with a unidirectional valve. Systematic early mobilization was performed on five levels. RESULTS: Significant increases were observed for values for maximal inspiratory pressure and the Medical Research Council score in the early mobilization group. However, no statistically significant improvement was observed for maximal expiratory pressure or MV duration (days), length of stay in the intensive care unit (days), and length of hospital stay (days). CONCLUSION: The early mobilization group showed gains in inspiratory and peripheral muscle strength.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):72-78
DOI 10.1590/S0103-507X2012000100011
OBJECTIVE: To assess the effects of passive mobilization on acute hemodynamic responses in mechanically ventilated patients. METHODS: This cross-sectional, quantitative, observational study enrolled patients who were admitted to the intensive care unit, sedated and mechanically ventilated. The infusion of sedative and analgesic drugs aimed to maintain a Ramsay scale sedation level of 4 to 6. Passive mobilization consisted of hip and knee flexion-extension movements for five minutes. After 10 minutes of rest, an additional five minutes of flexion-extension passive movements was performed for the shoulders. Hemodynamic assessments (heart rate and systolic, diastolic and mean blood pressure) were performed one minute before the mobilization protocol and one minute after each phase. The double product and myocardial oxygen consumption were calculated using appropriate formulas. RESULTS: A total of 13 patients (69.2% male, with a mean age of 69.1 ± 15.8 years) were admitted from June to December, 2011. Passive mobilization led to statistically significant increases in heart rate, double product and myocardial oxygen consumption. However, mean blood pressure was not significantly altered. CONCLUSIONS: Our results suggest that passive mobilization of mechanically ventilated and sedated patients is safe and provides beneficial effects on acute hemodynamic parameters, particularly heart rate, although mean blood pressure is not significantly altered
Abstract
Rev Bras Ter Intensiva. 2012;24(1):52-57
DOI 10.1590/S0103-507X2012000100008
OBJECTIVE: To determine the association between the preoperative administration of statins and postoperative delirium in a prospective cohort of patients undergoing cardiac surgery. METHODS: All adult patients who were admitted to the intensive care unit following cardiac surgery between January and June 2011 were included. Delirium was screened during the postoperative period using the Confusion Assessment Method for Intensive Care Unit (CAM-ICU) and Intensive Care Delirium Screening Checklist (ICDSC). RESULTS: A total of 169 patients underwent elective cardiac surgery, and 40.2% of the patients were treated preoperatively with statins. Delirium was identified using the CAM-ICU in 14.9% of patients not taking preoperative statins in comparison with 11.8% of the patients taking statins (p = 0.817). Using the ICDSC, delirium was identified in 18.8% of patients not taking statins in comparison with 10.3% of the patients taking statins (p = 0.191). CONCLUSION: The use of preoperative statins is not correlated with postoperative delirium in patients undergoing cardiac surgery.
Abstract
Rev Bras Ter Intensiva. 2012;24(1):64-70
DOI 10.1590/S0103-507X2012000100010
OBJECTIVE: To assess the consciousness level, pulmonary and hemodynamic effects of orthostatic position in intensive care patients. METHODS: This study was conducted from April 2008 to July 2009 in the Adult Intensive Care Unit, Hospital das Clínicas, Universidade Estadual de Campinas, São Paulo, Brazil. Fifteen patients were included who were mechanically ventilated for more than seven days and had the following characteristics: tracheotomized; receiving intermittent nebulization; maximal inspiratory pressure of less than -25 cm H2O; Tobin score less than 105; preserved respiratory drive; not sedated; partial arterial oxygen pressure greater than 70 mm Hg; oxygen saturation greater than 90%; and hemodynamically stable. With inclinations of 0º, 30º and 50º, the following parameters were recorded: consciousness level; blinking reflex; thoracoabdominal cirtometry; vital capacity; tidal volume; minute volume; respiratory muscle strength; and vital signs. RESULTS: No neurological level changes were observed. Respiratory rate and minute volume (V E) decreased at 30% and later increased at 50%; however, these changes were not statistically significant. Abdominal cirtometry and maximal expiratory pressure increased, but again, the changes were not statistically significant. Regarding maximal inspiratory pressure and vital capacity, statistically significant increases were seen in the comparison between the 50º and 0º inclinations. However, tidal volume increased with time in the comparisons between 30º and 0º and between 50º and 0º. Mean blood pressure increased only for the comparison of 50º versus 0º. Heart rate increased with time for the comparisons between 30º and 0º, between 50º and 0º and between 50º and 30º. CONCLUSION: Passive orthostatism resulted in improved tidal volume and vital capacity, maximal inspiratory pressure and increased heart rate and mean blood pressure in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(4):470-477
DOI 10.1590/S0103-507X2011000400012
OBJECTIVE: This study assessed the role of the nursing staff in pain management and verified the pain experiences of patients undergoing major surgery and receiving postoperative care in the intensive care unit. METHOD: This was a prospective, observational study of postoperative patients who were admitted to the intensive care unit and later discharged to one of the hospital's regular wards. Patients with impaired communication were excluded. All patients signed an informed consent form. Data were collected using a questionnaire of 13 pain-related questions. RESULTS: A total of 167 patients were included, and 69.5% were male. Patient age ranged from 50-59 years, and the intensive care unit stay was one to three days. The majority of the patients (85%) reported no difficulties in expressing their painful symptoms, and the nursing approach in 54.5% of patients was only to recognize the presence or absence of pain. No pain scale was used. The most painful conditions included the surgical wound and bed positioning. CONCLUSION: The nursing team was apparently more concerned with the presence of pain than with its quality, severity or possible painful stimuli. Pain scales were not used, which suggests the need for continued education of the nursing professionals on the manner of approaching their patients and assessing their patients' pain.