Abstract
Rev Bras Ter Intensiva. 2011;23(2):164-169
DOI 10.1590/S0103-507X2011000200008
OBJECTIVE: To evaluate the effects of hemodynamic, respiratory and metabolic changes on intracranial pressure in a model of acute lung injury and abdominal compartment syndrome. METHODS: Eight Agroceres pigs were submitted to five different clinical scenarios after instrumentation: 1) a baseline condition with low intra-abdominal pressure and healthy lungs; 2) pneumoperitoneum with 20 mmHg intra-abdominal pressure; 3) acute lung injury induced by pulmonary lavage with surfactant deactivation; 4) pneumoperitoneum with 20 mmHg intra-abdominal pressure with lung pulmonary injury and low positive end-expiratory pressure; and 5) 27 cmH2O positive end-expiratory pressure with pneumoperitoneum and acute lung injury. Respiratory and hemodynamic variables were collected. A multivariate analysis was conducted to search for variables associated with increased intracranial pressure in the five scenarios. RESULTS: Only plateau airway pressure showed a positive correlation with intracranial pressure in the multivariate analysis. In the models with acute lung injury, plateau airway pressure, CO2 arterial pressure, end tidal CO2 and central venous pressure were positively correlated with increased intracranial pressure. CONCLUSION: In a model of multiple organ dysfunction with associated clinical conditions causing increased intra-thoracic and abdominal pressure, increased intracranial pressure triggered by elevated intra-abdominal pressure is apparently caused by worsened respiratory system compliance and a reduced brain venous drainage gradient due to increased central venous pressure.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):176-182
DOI 10.1590/S0103-507X2011000200010
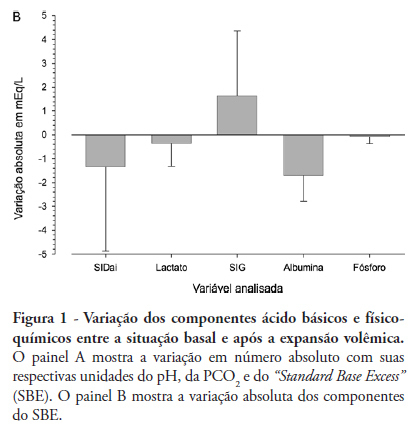
OBJECTIVE: The aim of this study was to characterize and quantify metabolic acidosis that was caused by initial volume expansion during the reanimation of patients with severe sepsis and septic shock. METHODS: A blood sample was drawn for physicochemical characterization of the patient's acid-base equilibrium both before and after volume expansion using 30 mL/kg 0.9% saline solution. The diagnosis and quantification of metabolic acidosis were based on the standard base excess (SBE). RESULTS: Eight patients with a mean age of 58 ± 13 years and mean APACHE II scores of 20 ± 4 were expanded using 2,000 ± 370 mL of 0.9% saline solution. Blood pH dropped from 7.404 ± 0.080 to 7.367 ± 0.086 (p=0.018), and PC O2 increased from 30 ± 5 to 32 ± 2 mmHg (p=0.215); SBE dropped from -4.4 ± 5.6 to -6.0 ± 5.7 mEq/L (p=0.039). The drop in SBE was associated with the acidifying power of two factors, namely, a significant increase in the strong ion gap (SIG) from 6.1 ± 3.4 to 7.7 ± 4.0 mEq/L (p = 0.134) and a non-significant drop in the apparent inorganic strong ion differences (SIDai) from 40 ± 5 to 38 ± 4 mEq/L (p = 0.318). Conversely, the serum albumin levels decreased from 3.1 ± 1.0 to 2.6 ± 0.8 mEq/L (p = 0.003) with an alkalinizing effect on SBE. Increased serum chloride levels from 103 ± 10 to 106 ± 7 mEq/L (p < 0.001) led to a drop in SIDai. CONCLUSION: Initial resuscitation using 30 mL/kg of 0.9% saline solution for patients with severe sepsis and septic shock is associated with worsened metabolic acidosis, as measured by SBE. This worsened SBE can be ascribed to a serum increase in the levels of unmeasurable anions and chloride.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):183-189
DOI 10.1590/S0103-507X2011000200011
OBJECTIVE: To investigate the relationship between adequacy of energy intake and intensive care unit mortality in patients receiving exclusive enteral nutrition therapy. METHODS: Observational and prospective study conducted during 2008 and 2009. Patients above 18 years with exclusive enteral nutrition therapy for at least 72 hours were included. The adequacy of energy intake was estimated by the administered/prescribed ratio. Non-conditional logistic regression was used to assess the relationship between predictive variables (adequacy of energy intake, APACHE II, gender, age, and intensive care unit length of stay) and intensive care unit mortality. RESULTS: Sixty-three patients (mean 58 years, 27% mortality) were included, 47.6% of whom received more than 90% of the energy prescribed (mean adequacy 88.2%). Mean energy balance was -190 kcal/day. Significant associations between death in the intensive care unit and the variables age and intensive care unit length of stay were observed, after removing the variables adequacy of energy intake, APACHE II, gender and age during the modeling process. CONCLUSION: In our study, adequacy of energy intake did not affect intensive care unit mortality. Carefully followed enteral nutrition protocols, resulting in an administered/prescribed ratio above 70%, are apparently not sufficient to impact the mortality rates in the intensive care unit. Therefore, it may not be necessary to achieve 100% of the targeted energy, considering the high frequency of enteral feeding interruptions due to gastrointestinal intolerance and fasting for tests and procedures. Additional research is needed to identify the optimal energy intake for improved outcomes and reduced costs.
Abstract
Rev Bras Ter Intensiva. 2011;23(2):217-221
DOI 10.1590/S0103-507X2011000200015
In recent years, international health quality assurance organizations have been recommending ultrasound guidance for central venous punctures. This article reviews the evidence behind these recommendations. The MEDLINE, PubMed and SCIELO databases were searched for the following MeSH terms: central venous access, ultrasonography, and adults. The search was conducted on September 24, 2010, and selected meta-analyses, randomized clinical trials and reviews, retrieving 291 papers. The 21 most important papers were analyzed in this review. The internal jugular vein is the most studied ultrasound-guided puncture site, with meta-analysis showing lower relative risks of failure and complications. In addition, the largest available randomized clinical trial demonstrated a reduced central venous catheter-associated blood stream infection rate. There are few studies involving subclavian vein puncture; however, ultrasound was shown to be beneficial in two meta-analyses (however, with small numbers of patients). Regarding the femoral venous site, only one randomized clinical trial (20 patients) was identified, showing positive findings. In a British cost-effectiveness study, ultrasound use lead to resource savings for different sites of venous puncture. There is strong evidence for ultrasound benefit for internal jugular vein puncture. Although the method appears attractive for the other sites, the data are not sufficient to support any recommendation.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):78-86
DOI 10.1590/S0103-507X2011000100013
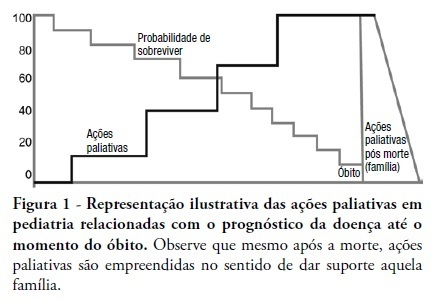
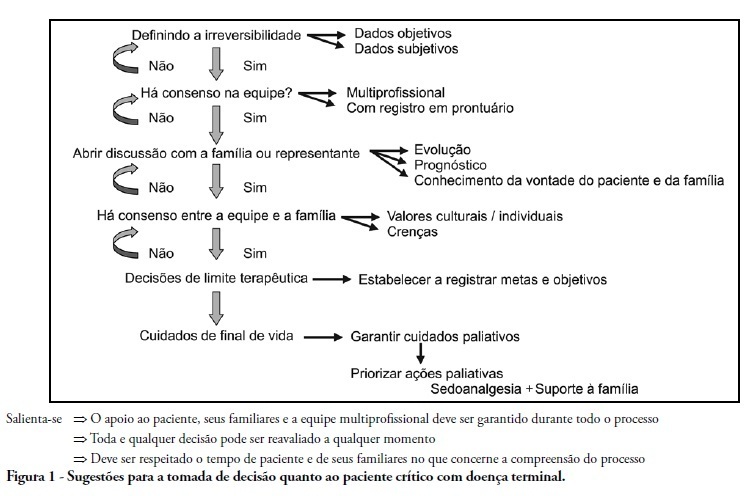
This review discusses the main dilemmas and difficulties related to end-of-life decision's in children with terminal and irreversible diseases and propose a rational sequence for delivering palliative care to this patients' group. The Medline and Lilacs databases were searched using the terms 'end of life', 'palliative care', 'death' and 'terminal disease' for articles published in recent years. The most relevant articles and those enrolling pediatric patients were selected and compared to previous authors' studies in this field. The current Brazilian Medical Ethics Code (2010) was analyzed regarding end-oflife practices and palliative care for terminal patients. Lack of knowledge, insufficient specific training, and legal concerns are the main reasons why end-of-life decisions in terminal children are based on medical opinion with scarce family participation. The current Brazilian Medical Ethics Code (2010) fully supports end-of-life decisions made consensually with active family participation. Honest dialogue with the family regarding diagnostic, prognostic, therapeutic and palliative care measures should be established gradually to identify the best strategy to meet the child's end-of-life needs. Treatment focused on the child's welfare combined with the family's participation is the basis for successful palliative care of children with terminal diseases.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):24-29
DOI 10.1590/S0103-507X2011000100005
Palliative care is aimed to improve the quality of life of both patients and their family members during the course of life-threatening diseases through the prevention, early identification and treatment of the symptoms of physical, psychological, spiritual and social suffering. Palliative care should be provided to every critically ill patient; this requirement renders the training of intensive care practitioners and education initiatives fundamental. Continuing the Technical Council on End of Life and Palliative Care of the Brazilian Association of Intensive Medicine activities and considering previously established concepts, the II Forum of the End of Life Study Group of the Southern Cone of America was conducted in October 2010. The forum aimed to develop palliative care recommendations for critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):30-35
DOI 10.1590/S0103-507X2011000100006
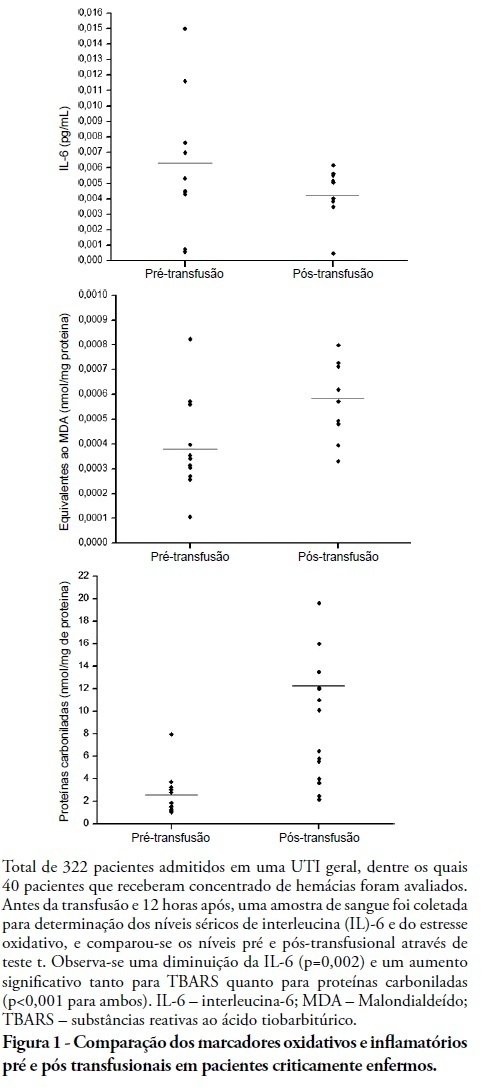
INTRODUCTION: Red blood cell transfusions are common in intensive care units. For many years, transfusions of red blood were thought to have obvious clinical benefits. However, in recent years, the risks and benefits of blood transfusions have been examined more carefully, including the risk of increased morbidity and mortality due to transfusion-related immunomodulation effects. OBJECTIVES: To evaluate red blood cell transfusion effects and the relationship of this procedure to the production of inflammatory cytokines and oxidative damage in critically ill patients admitted to an intensive care unit. METHODS: For 6 months in 2008, we evaluated patients admitted to an intensive care unit who underwent packed red blood cell transfusions. Pre- and post-transfusion levels of interleukin-6, carbonylated proteins and thiobarbituric acid reactive substances were assessed. RESULTS: Serum post-transfusion interleukin-6 levels were reduced, and thiobarbituric acid reactive substances and carbonylated proteins were significantly increased. No statistically significant relationship was found between the levels of pre- and post-transfusion interleukin-6 and thiobarbituric acid reactive substances and the mortality rate. However, there was a significant relationship between levels of post-transfusion carbonylated proteins and mortality. CONCLUSION: Red blood cell transfusion is associated with increased oxidative damage markers and reduced interleukin-6 levels in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2011;23(1):62-67
DOI 10.1590/S0103-507X2011000100011
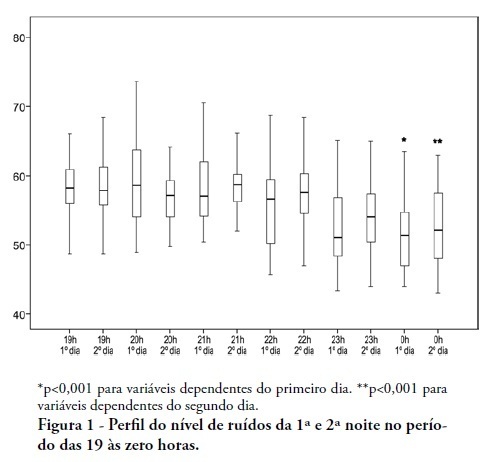
OBJECTIVES: To identify the main causes of stress in patients staying in a coronary unit and to assess the influence of noise levels on their perception of stress. METHODS: This was a prospective, descriptive and quantitative study conducted between June and November 2009 in the Coronary Unit of the Hospital de Clínicas da Universidade Estadual de Campinas. The Intensive Care Unit Environmental Stressor Scale was used on the first, second and third days of hospitalization to identify stressors. The noise level was measured on the first and second nights using an Instrutherm DEC-460 decibel meter. RESULTS: Overall, 32 clinical heart disease patients were included. The median Intensive Care Unit Environmental Stressor Scale scores were 67.5, 60.5 and 59.5 for the first, second and third days, respectively. The differences were not statistically significant. The highest noise level (a median of 58.7 dB) was detected on the second night at 9:00 pm; the lowest level (51.5 dB) was measured on the first night at 12:00 am. In a multiple linear regression model, the first-night noise level had a 33% correlation with the second-day stress scale score, and for the second night, the correlation with the third-day stress scale score was 32.8% (p = 0.001). CONCLUSION: Patients admitted into a coronary unit have an increased perception of stress. Higher noise levels are also responsible for the perception of stress in these patients.