Abstract
Rev Bras Ter Intensiva. 2009;21(4):353-358
DOI 10.1590/S0103-507X2009000400004
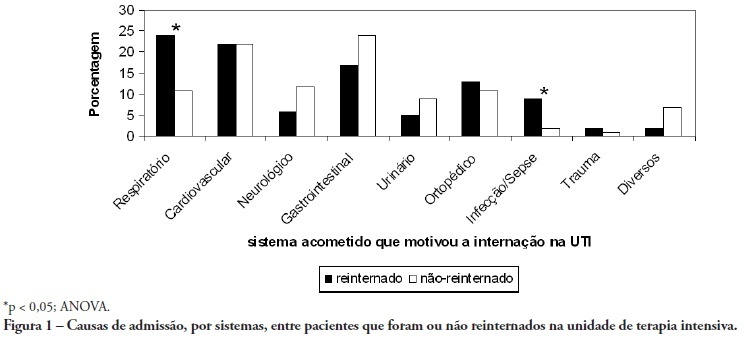
OBJECTIVE: To predict readmission in intensive care unit analyzing the first 24 hours data after intensive care unit admission. METHODS: The first intensive care unit admission of patients was analyzed from January to May 2009 in a mixed unit. Readmission to the unit was considered those during the same hospital stay or within 3 months after intensive care unit discharge. Deaths during the first admission were excluded. Demographic data, use of mechanical ventilation, and report of stay longer than 3 days were submitted to uni and multivariate analysis for readmission. RESULTS: Five hundred seventy-seven patients were included (33 excluded deaths). The readmission group had 59 patients, while 518 patients were not readmitted. The lead time between the index admission and readmission was 9 (3-28) days (18 were readmitted in less than 3 days), and 10 died. Patients readmitted at least once to the intensive care unit had the differences below in comparison to the control group: older age: 75 (67-81) versus 67 (56-78) years, P<0.01; admission for respiratory insufficiency or sepsis: 33 versus 13%, P<0.01; medical admission: 49 versus 32%, P<0.05; higher SAPS II score: 27 (21-35) versus 23 (18-29) points, P<0.01; Charlson index: 2 (1-2) versus 1 (0-2) points, P<0.01; first ICU stay longer than 3 days: 35 versus 23%, P<0.01. After logistic regression, higher age, Charlson index and admission for respiratory and sepsis were independently associated to readmissions in intensive care unit. CONCLUSION: Age, comorbidities and respiratory- and/or sepsis-related admission are associated with increased readmission risk in the studied sample.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):359-368
DOI 10.1590/S0103-507X2009000400005
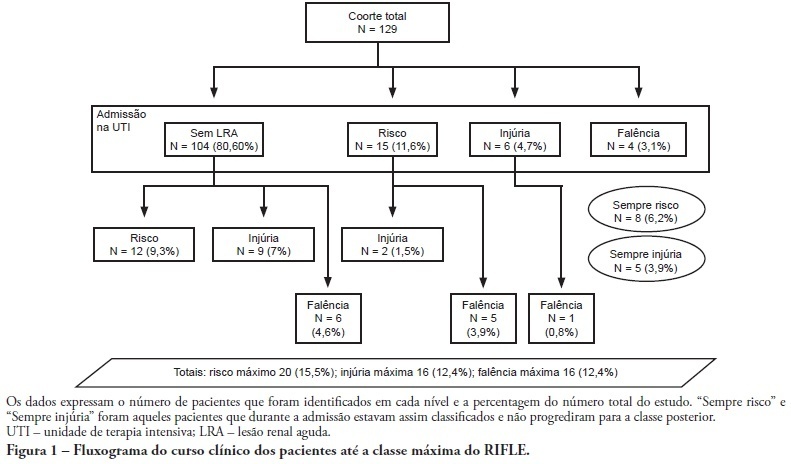
OBJECTIVE: To correlate the RIFLE classification with mortality and length of stay both in the intensive care unit and hospital. METHODS: A prospective, observational, longitudinal cohort study, approved by the Institution's Ethics Committee. Data were collected for all patients staying longer than 24 hours in the intensive care unit of Hospital Universitário Polydoro Ernani de São Thiago - Universidade Federal de Santa Catarina from September 2007 to March 2008, followed-up either until discharge or death. Patients were divided in two groups: with or without acute kidney injury. The acute kidney injury group was additionally divided according to the RIFLE and sub-divided according to the maximal score in Risk, Injury of Failure. Loss and End-stage classes were not included in the study. APACHE II and SOFA were also evaluated. The t Student and Chi-Square tests were used. A P<0.05 was considered statistically significant. RESULTS: The sample included 129 patients, 52 (40.3%) with acute kidney injury according to RIFLE. Patients were more severely ill in this group, with higher APACHE and SOFA scores (P<0.05). Compared to the without kidney injury group, the kidney injury severity caused increased intensive care unity (Risk 25%; Injury 37.5%; Failure 62.5%) and in-hospital (Risk 50%; Injury 37.5%; Failure 62.5%) mortality, and longer intensive care unit stay (P<0.05). CONCLUSION: The RIFLE system, according to the severity class, was a marker for risk of increased intensive care unit and in-hospital mortality, and longer intensive care unit stay. No relationship with in-hospital length of stay was found.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):369-375
DOI 10.1590/S0103-507X2009000400006
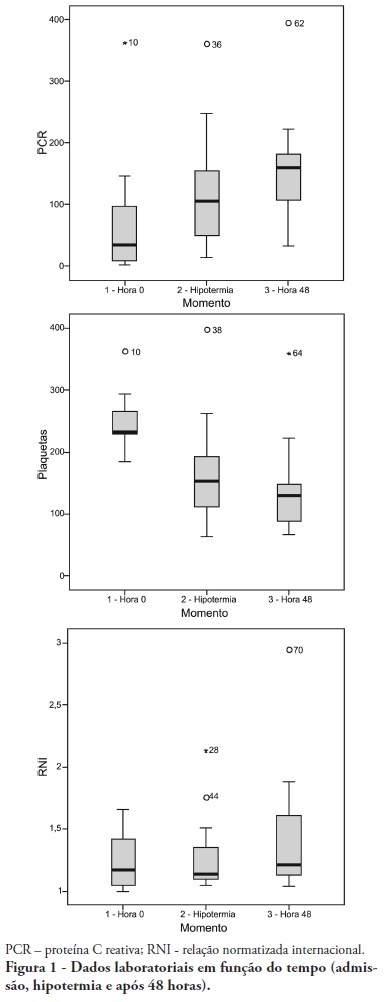
OBJECTIVE: To determine the characteristics of patients undergoing standard institutional protocol for management of resuscitated patients after a cardiac arrest episode, including therapeutic hypothermia. METHODS: This was a retrospective analysis of 26 consecutive patients admitted following cardiac arrest, between January 2007 and November 2008. RESULTS: All cases underwent therapeutic hypothermia. Average age was 63 years, and the patients were predominantly male. Cardiac arrest event was out-of-hospital in 8 cases, in the emergency room in 3 cases, in the wards in 13 cases and in the operation room in 2 cases. The cardiac arrest rhythm was ventricular fibrillation in seven patients, asystolia in 11, pulseless electrical activity in 5 cases, and was undetermined in 3 patients. The interval between the cardiac arrest and return of spontaneous circulation was 12 minutes (SD ± 5 min). The time to reach the target temperature was 5 ± 4 hours, the hypothermia time was 22 ± 6 hours and time to rewarming 9 ± 5.9 hours. Fourteen patients died in the intensive care unit, a 54% mortality, and three patients died during the in-hospital stay, a 66% in-hospital mortality. There was statistically significant reduction in hemoglobin (p<0.001), leukocytes (p=0.001), platelets (p<0.001), lactate (p<0.001) and potassium (p=0.009), values and increased C reactive protein (p=0.001) and INR (p=0.004) after hypothermia. CONCLUSIONS: The creation of a standard operative protocol for therapeutic hypothermia in post cardiac arrest patients management resulted in a high use of therapeutic hypothermia. The clinical results of this protocol adapted from randomized studies are similar to the literature.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):376-383
DOI 10.1590/S0103-507X2009000400007
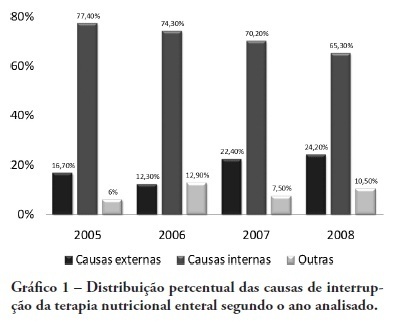
OBJECTIVE: Monitor the adequacy of enteral nutritional therapy at the intensive care unit aiming to improve the quality of nutritional assistance. METHODS: Prospective and observational study developed at the adult intensive care unit from 2005 to 2008. Patients over 18 years of age with exclusive enteral nutritional therapy for over 72h participated in the sample. The average values and the percentile adequacy of energy and proteins calculated, prescribed and administered in each year were analyzed. The factors responsible for the non-conformity of the administration planned were classified into intensive care unit extrinsic or intrinsic causes. The quality indicators proposed by the ILSI Brazil were applied, and expressed into percentile goals. In the statistic analyses, confidence interval and the t Student e Mann-Whitney (p<0.05) tests were used, according to the Epi Info program. RESULTS: One hundred and sixteen patients were followed up. There were statically difference in values of energy and protein administered in 2005 and in 2006, when compared to those in 2008. The adequacy calculated/prescribed remained close to 100% in all the surveys and the adequacy administered/prescribed increased from 74% in 2005, to 89% in 2008. An increase in interruptions of enteral nutritional therapy for external factors and the decrease in interruptions for intensive care unit internal factors were verified. The quality indicators equally reflect the evolution of the patient care. CONCLUSION: In the four yearly surveys, a progressive enhancement of nutritional support was verified. Quality indicators allow nutritional care evolution monitoring, the comparison to other services data, and are a new perspective for enteral nutritional therapy assessment.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):384-390
DOI 10.1590/S0103-507X2009000400008
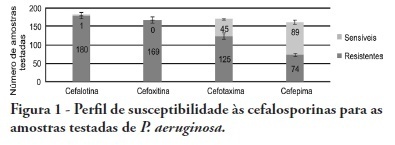
OBJECTIVES: Pseudomonas aeruginosa is an increasingly prevalent opportunistic pathogen in hospital infection cases. Its high resistance rates to many antimicrobials has given this microorganism a relevant role among other highly prevalent bacteria involved in nosocomial infections. This study aimed to analyze epidemiologic characteristics of P. aeruginosa and to evaluate its susceptibility to antimicrobial agents at Hospital das Clínicas of the Universidade Federal de Pernambuco METHODS: A retrospective study was performed based on the registry book of miscellaneous secretions from the bacteriology laboratory of the Hospital das Clínicas involving the period between January and June 2008. Among the secretions registered, were identified the positives samples for P. aeruginosa, whose origin was analyzed, as well as its susceptibility profile to routinely used in our laboratory antimicrobials. RESULTS: The bacteria most frequently isolated from miscellaneous secretions bacteria were P. aeruginosa (26%) and S. aureus (25%). P. aeruginosa was mainly isolated from respiratory infections, with 33% of positive samples for this organism from tracheal secretions and 21% from nasal. The most effective antimicrobials against P. aeruginosa were: amikacin, imipenem, meropenem and aztreonam. CONCLUSIONS: These results show a high prevalence of P. aeruginosa in the Hospital das Clínicas of the Universidade Federal de Pernambuco. Despite featuring high resistance rates to older antimicrobials, as cephalosporins first and second generations and chloramphenicol, this pathogen showed good susceptibility to agents routinely used in this hospital.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):391-397
DOI 10.1590/S0103-507X2009000400009
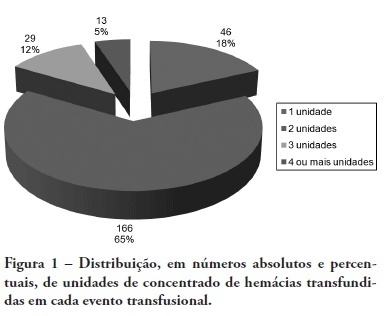
BACKGROUND: The anemia is a common problem upon admission of the patients in the intensive care unit being the red blood cell transfusion a frequent therapeutic. The causes of anemia in critical patients who under go red blood cell transfusion are several: acute loss of blood after trauma, gastrointestinal hemorrhage, surgery amongst others. Currently, few studies are available regarding the use of blood components in patients at intensive care unit. Although blood transfusions are frequent in intensive care unit, the optimized criteria for handling are not clearly defined, with no available guidelines. OBJECTIVES: To analyze the clinical indications of the use of the red blood cell in the intensive care unit. METHODS: The clinical history of the patients admitted in the intensive care unit were analyzed, revisiting which had have red blood cell transfusion in the period between January 1st 2005 and December 31 2005. The study was accepted by the Research Ethics Committee - Comitê de Ética em Pesquisa (CEP) - of the University of South of Santa Catarina (UNISUL). RESULTS: The transfusion rate was 19,33, and the majority of the patients were of the male gender. Their age prevalence was of 60 years old or older. The mortality rate among patients who under went red blood cell transfusion died was of 38,22%. The transfusions criterias were low serum hemoglobin (78%) and the hemoglobin pre - transfusion was 8,11 g/dL. CONCLUSIONS: Politrauma and sepsis/sepsis chock were the pre diagnosis criteria. A low hemoglobin level is the main clinical criteria with average hemoglobin pre - transfusion was 8,11 g/dL.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):398-403
DOI 10.1590/S0103-507X2009000400010
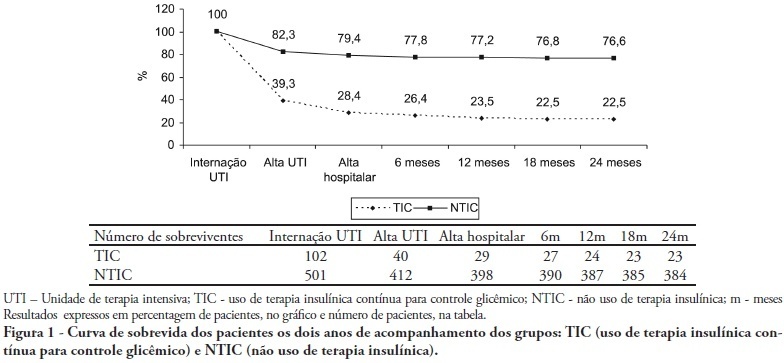
OBJECTIVES: Stress-induced hyperglycemia is frequent in critically ill patients and has been associated with increased mortality and morbidity (both in diabetic and non-diabetic patients). This study objective was to evaluate the profile and long-term prognosis of critically ill patients undergoing tight glucose-control. METHODS: Prospective cohort. All patients admitted to the intensive care unit over 1-year were enrolled. We analyzed demographic data, therapeutic intervention, and short- (during the stay) and long-term (2 years after discharge) mortality. The patients were categorized in 2 groups: tight glucose control and non-tight glucose-control, based on the unit staff decision. RESULTS: From the 603 enrolled patients, 102 (16.9%) underwent tight control (glucose <150 mg/dL) while 501 patients (83.1%) non-tight control. Patients in the TGC-group were more severely ill than those in the non-tight control group [APACHE II score (14 ± 3 versus 11 ± 4, P=0.04), SOFA (4.9 ± 3.2 versus 3.5 ± 3.4, P<0.001) and TISS-24h (25.7 ± 6.9 versus 21.1 ± 7.2, P< 0.001)]. The tight control group patients also had worse prognosis: [acute renal failure (51% versus 18.5%, P<0.001), critical illness neuropathy (16.7% versus 5.6%, P<0.001)] and increased mortality (during the ICU-stay [60.7% versus 17.7%, P<0.001] and within 2-years of the discharge [77.5% versus 23.4%; P<0.001]). CONCLUSION: Critically ill patients needing tight glucose control during the unit stay have more severe disease and have worse short and long-term prognosis.
Abstract
Rev Bras Ter Intensiva. 2009;21(2):148-154
DOI 10.1590/S0103-507X2009000200006
PURPOSE: Identify and evaluate the perception of Intensivist Nurses in a University Hospital in Londrina, of dysthanasia in terminal patients at the Intensive Care Unit. METHODS: Qualitative study. Data were collected by semi-structured recorded interview involving nine nurses working in a university hospital intensive care units, during January 2009. A thematic analysis was used to evaluate subjects' speech and identify discussion categories. RESULTS: Five categories were identified, discussed based on the authors' experience and literature, namely: measures prolonging life of patients with no chance of cure in the intensive care unit; nurses' actions/reactions when facing dysthanasia; reasons leading to prolonging life of patients with no chance of cure; nurses' feelings about dysthanasia and life prolongation; care measures as opposed to dysthanasia. CONCLUSION: Experiencing of nurses when facing dysthanasia actions was shown to be complex, a factor of suffering, frustration and discomfort for these professionals. In the nurses' view, lack of communication stands out as an important factor for dysthanasia, and measures to replace dysthanasia are those relieving suffering.