Abstract
Rev Bras Ter Intensiva. 2010;22(1):19-26
DOI 10.1590/S0103-507X2010000100005
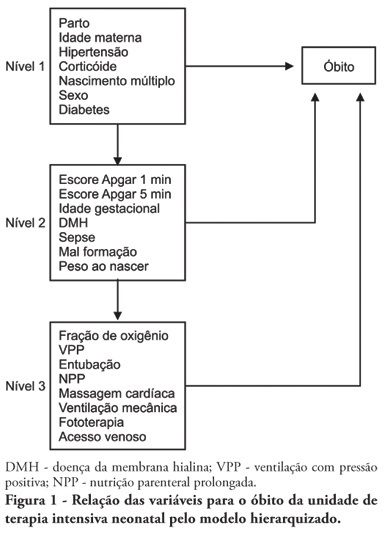
OBJECTIVE: To identify risk factors associated with death of infants admitted to neonatal intensive care unit of Taubaté University Hospital. METHODS: It is a longitudinal study with information obtained from medical records of newborns admitted to the neonatal intensive care unit of Taubaté University Hospital. Type of outcome, discharge or death, was dependent variable. The independent variables were maternal and gestational variables: maternal age, hypertension, diabetes, corticosteroid therapy and delivery; variables of the newborn: birth weight, gestation length, Apgar score in the first and fifth minutes of life, multiple birth, congenital malformations and sex; hospitalar variables: report of mechanical ventilation, positive pressure ventilation, reports of prolonged parenteral nutrition, sepsis, intubation, cardiac massage, phototherapy, hyaline membrane disease, oxygen and fraction of inspired oxygen. It was built a model in three hierarchical levels for the survival analysis by the Cox model; it was used the software Stata v9 and the final model contained variables with p <0.05. The risks were estimated by measure effect known as hazard ratio (HR) with confidence intervals of 95%. The newborns transferred during hospitalization to another service were excluded from the study. RESULTS: There were admitted during the study period 495 newborns, with 129 deaths (26.1%). In the final model, only the variables of steroid use (HR 1.64, 95% CI 1.02-2.70), malformation (HR 1.93, CI 95% 1,05-2,88), very low birth weight (HR 4.28, 95% CI 2,79-6,57) and Apgar scores lower than seven of no1 min (HR 1.87, 95% CI 1,19-2,93) and 5 min (HR 1.74, 95% CI 1,05-2,88) and the variables phototherapy (HR 0.34; 95% CI 0,22-0,53) and endotracheal intubation (HR 2.28, 95% CI 1 .41-3, 70). CONCLUSION: Factors related primarily to the newborn and the hospitalar internment (except therapy with corticosteroids) were identified as associated to mortality highlighting a possible protective factor of phototherapy and the risk of infants with very low birth weight.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):27-32
DOI 10.1590/S0103-507X2010000100006
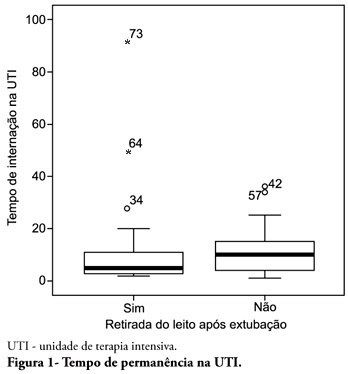
OBJECTIVE: To describe the withdrawal of the bed frequency in mechanic ventilation patients and its impact on mortality and length of stay in the intensive care unit. METHODS: This was a retrospective cohort study in mechanical ventilation patients. Clinical and epidemiological variables, withdrawal of bed related motor therapy, intensive care unit length of stay and mortality were evaluated. RESULTS: We studied 91 patients, mean age of 62.5± 18.8 years, predominantly female (52%) and mean intensive care unit length of stay of 07 days (95% CI, 8-13 days). Considering the withdrawal of the bed or not, no difference was observed between groups regarding length of stay in intensive care unit. Patients who were withdrawn of bed had a lower clinical severity. Their mortality rate was 29.7%. The not withdrawn of bed group had higher both actual and expected mortality. CONCLUSIONS: Patients withdrawn of bed following mechanical ventilation discontinuation showed lower mortality. It is suggested that early intensive care unit mobilization and withdrawal of bed should be stimulated.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):40-46
DOI 10.1590/S0103-507X2010000100008
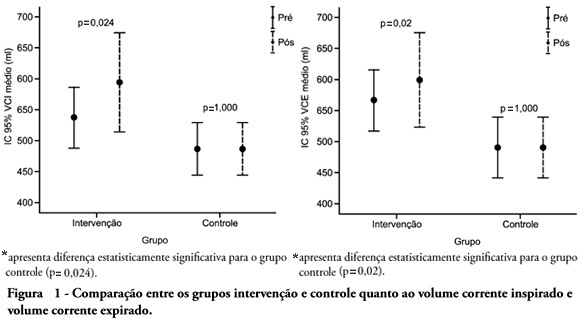
OBJECTIVE: To verify the effects of manual hyperinflation maneuver associated with positive end expiratory pressure in coronary artery bypass grafting patients. METHODS: This was a randomized trial, conducted from August 2007 to July 2008 in the intensive care unit of the Hospital Luterano (ULBRA). The patients were divided in the groups intervention - with manual hyperinflation plus positive end expiratory pressure - and controlThe ventilatory variables were measured before and after the manual hyperinflation. The t Student's test was used for independent and paired samples as well as Fisher's exact test and McNemar's Chi-square test with 0.05 significance level. RESULTS: Eighteen patients were included. The mean age was 64± 11 years and 55.6% were female. The inspired tidal volume was 594± 112ml in the intervention group and 487± 51ml in the control group (p=0.024) and the expired tidal volume was 598± 105ml in the intervention group and 490± 58ml in the control group (p=0.02). The mean pre-maneuver static pulmonary compliance in the intervention group was 41.6± 12.1 ml/cmH2O and post maneuver it was 47.4± 16.6 ml/cmH2O (p=0.03). There was no significant between groups difference in the following variables: oxygen peripheral saturation, oxygen arterial pressure, extubation time and radiological changes. CONCLUSION: The results show that the manual hyperinflation associated with positive end expiratory pressure maneuver trends to promote increased lung volumes and static compliance, however these findings require further confirmation.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):33-39
DOI 10.1590/S0103-507X2010000100007
OBJECTIVE: To verify if the maximal inspiratory pressure values with 40 seconds occlusion time are greater than with the 20 seconds occlusion time, and the impacts on the following patient's physiological variables: respiratory rate, pulse oxygen saturation, heart rate and blood pressure, before and after the measurements. METHODS: This was a transversal prospective randomized study. Fifty-one patients underwent maximal inspiratory pressure measurement, measured by one single investigator. The manometer was calibrated before each measurement, and then connected to the adapter and this to the unidirectional valve inspiratory branch for 20 or 40 seconds. RESULTS: The values with 40 seconds occlusion (57.6 ± 23.4 cmH2O) were significantly higher than the measurements taken with 20 seconds occlusion (40.5 ± 23.4 cmH2O; p=0.0001). The variables changes between the before and after measurement respiratory and hemodynamic parameters monitoring showed: heart rate variation for the 20 seconds occlusion 5.13 ± 8.56 beats per minute and after 40 seconds occlusion 7.94 ± 12.05 beats per minute (p = 0.053), versus baseline. The mean blood pressure change for 20 seconds occlusion was 9.29 ± 13.35 mmHg and for 40 seconds occlusion 15.52 ± 2.91 mmHg (p=0.021). The oxygen saturation change for 20 seconds occlusion was 1.66 ± 12.66%, and for 40 seconds 4.21 ± 5.53% (p=0.0001). The respiratory rate change for 20 seconds occlusion was 6.68 ± 12.66 movements per minute and for 40 seconds 6.94 ± 6.01 (p=0.883). CONCLUSION: The measurement of maximal inspiratory pressure using a longer occlusion (40 seconds) produced higher values, without triggering clinically significant stress according to the selected variables.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):47-52
DOI 10.1590/S0103-507X2010000100009
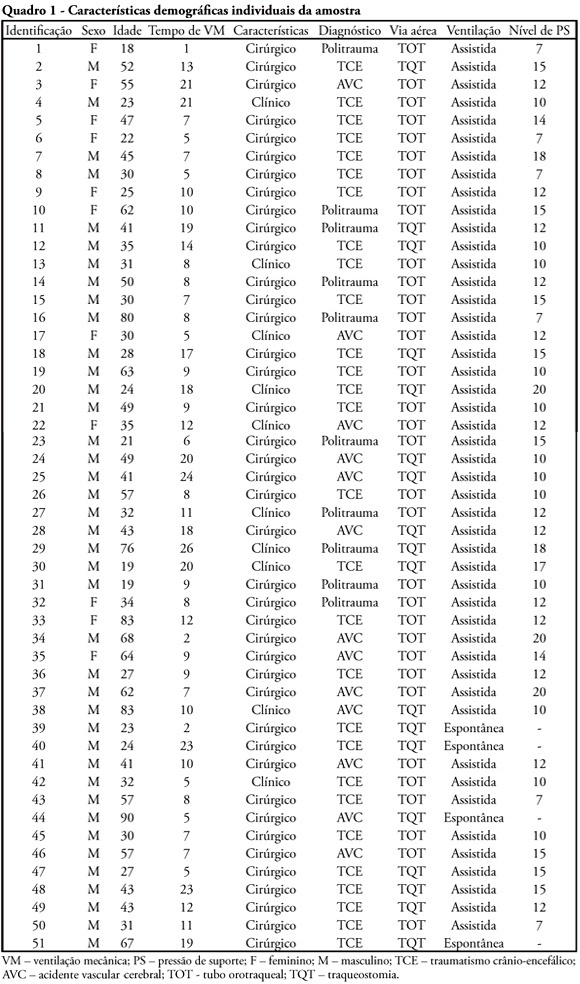
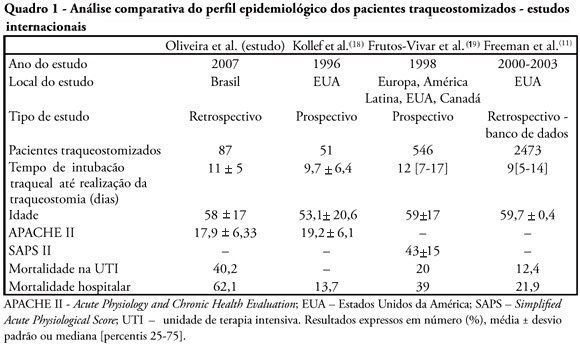
OBJECTIVES: Tracheostomy is a common procedure in intensive care unit to promote mechanical ventilation weaning. Despite tracheostomy is increasingly used there is no agreement of actual clinical practice of tracheostomy in different groups of patients in our environment. Objective of this study was to evaluate the epidemiological profile and outcomes of patients with tracheostomy at a clinical-surgical intensive care unit and compare this profile with the current literature. METHODS: Retrospective descriptive study through review of medical records and quality control database of "QuaTI" (Qualidade em Terapia Intensiva) of 87 patients with tracheostomy at Santa Casa de Belo Horizonte intensive care unit in 2007. We studied variables related to evolution aspects. RESULTS: The clinical and epidemiological analysis of the 87 patients showed: mean age 58 ± 17 years, mean Acute Physiology and Chronic Health Evaluation - APACHE II 18 ± 6, mean time of orotracheal intubation before tracheostomy of 11.17 ± 4.78 days. Intensive care unit mortality was 40.2% (35/87 patients), ward mortality was 36.5% (19/52) and overall hospital mortality 62.1% (54/87). Mean age of patients who died at intensive care unit (65 + 17 years) was greater than who were discharged to ward (53 ± 16 years) p = 0.003. Mean age of who died in hospital (intensive care unit and ward) (62 ± 17 years) was also higher than survivors (52 ± 16 years) p = 0.008. Old age (> 65 years) was related to intensive care unit mortality (OR 2.874, CI 1.165 a 7.088 p = 0.020) and also related to the overall hospital mortality (OR 3.202, CI 1.188 a 8.628 p = 0.019). There were not others variables related to mortality in this sample. CONCLUSIONS: The epidemiological profile of patients who underwent tracheotomy in the intensive care unit showed high mortality rate when compared to international series. Senility was related to worse outcome in these patients. Other issues were not related mortality in this group.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):53-63
DOI 10.1590/S0103-507X2010000100010
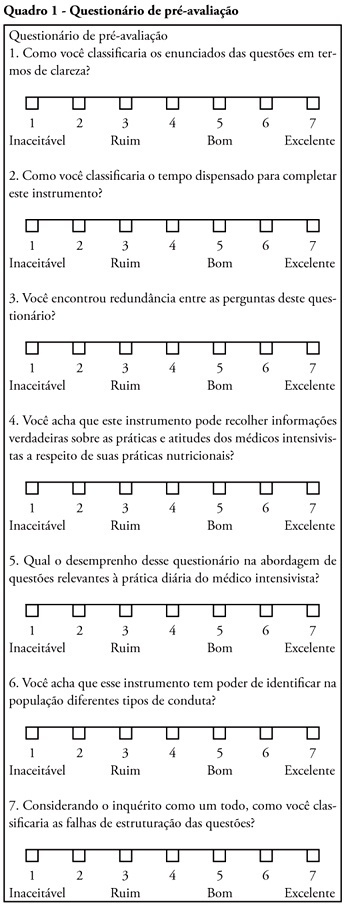
OBJECTIVE: Nutritional therapy is an important element in critical ill patient care. Although recognized as specialty, multidisciplinary teams in nutrition support are scarce in our country. Possibly, nutrition support therapy is applied by intensive care physicians and this may vary. The aim of the study is describe these specialists perceptions about theirs attitudes in enteral nutrition support. METHODS: A questionnaire was elaborated in an on-line platform. After pre-validation, it was sent by electronic mail to intensivists. In 30 days answers were collected, considering only the full-filled questionnaires. RESULTS: One hundred an fourteen forms were returned, 112 were analyzed. The responders were localized at majority in southeastern region. About beggining of nutritional support, the majority of answers reflect perceptions in accord to specialists societies recommendations. The responders' perception the frequent utilization of assistentials protocols in nutrition care. After support beginning, the responders perceptions about theirs participation in changes in therapeutic plan seems to be lower. The self-knowledge about the theme among the responders was 6.0 (arithmetic media) in a 1 to 10 scale. CONCLUSIONS: More studies are necessary to evaluate nutritional support practices among intensive care physicians. Alternatives to on-line platform should be considered. Possibly, intensive care physicians do better in the initial phases of enteral support than in continuity of care. Intensive care physicians knowledge about the issue is suboptimal.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):343-348
DOI 10.1590/S0103-507X2009000400002
OBJECTIVE: Traumatic brain injury is the major cause of death among individuals between 1-45 years-old. The outcome of traumatic brain injury may be related to brain susceptibility to the injury and genetic factors. Genes that may affect traumatic brain injury outcome are being investigated, however there is still few data concerning the association between genetic polymorphisms and traumatic brain injury outcome. The interleukin-1 beta gene (IL-1B) is one of the most studied genes, because levels of this cytokine are raised after traumatic brain injury and this can affect worsen the prognosis. The aim of this study was to test whether the -31C/T polymorphism, located at the promoter region of the IL-1B gene, is associated with primary short-term outcome (death or intensive care unit discharge) in severe traumatic brain injury patients. METHODS: Were studied 69 patients admitted with severe traumatic brain injury in three hospitals of the metropolitan region of Porto Alegre. The polymorphism was analyzed by polymerase chain reaction, followed by restriction digestion. RESULTS: Severe traumatic brain injury was associated with a 45% mortality rate. No significant differences were observed in the allele and genotype frequencies between patients stratified by traumatic brain injury outcome. CONCLUSION: Our findings suggest that -31C/T IL-1B gene polymorphism have no significant impact on the outcome of patients after acute severe traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2009;21(4):349-352
DOI 10.1590/S0103-507X2009000400003
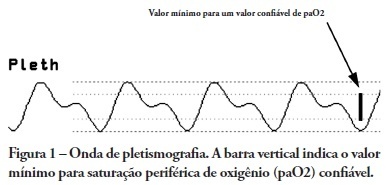
OBJECTIVES: Arterial pulse pressure respiratory variation is a good predictor of fluid response in ventilated patients. Recently, it was shown that respiratory variation in arterial pulse pressure correlates with variation in pulse oximetry plethysmographic waveform amplitude. We wanted to evaluate the correlation between respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude, and to determine whether this correlation was influenced by norepinephrine administration. METHODS: Prospective study of sixty patients with normal sinus rhythm on mechanical ventilation, profoundly sedated and with stable hemodynamics. Oxygenation index and invasive arterial pressure were monitored. Respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude were recorded simultaneously in a beat-to-beat evaluation, and were compared using the Pearson coefficient of agreement and linear regression. RESULTS: Thirty patients (50%) required norepinephrine. There was a significant correlation (K = 0.66; p < 0.001) between respiratory variation in arterial pulse pressure and respiratory variation in pulse oximetry plethysmographic waveform amplitude. Area under the ROC curve was 0.88 (range, 0.79 - 0.97), with a best cutoff value of 14% to predict a respiratory variation in arterial pulse pressure of 13. The use of norepinephrine did not influence the correlation (K = 0.63, p = 0.001, respectively). CONCLUSIONS: Respiratory variation in arterial pulse pressure above 13% can be accurately predicted by a respiratory variation in pulse oximetry plethysmographic waveform amplitude of 14%. The use of norepinephrine does not alter this relationship.