Abstract
Rev Bras Ter Intensiva. 2010;22(2):138-143
DOI 10.1590/S0103-507X2010000200007
BACKGROUND: The elderly population is increasing all over the world. The need of intensive care by the elderly is also increasing. There is a lack of studies investigating the risk factors for death among critically ill elderly patients. This study aims to investigate the factors associated with death in a population of critically ill elderly patients admitted to an intensive care unit in Brazil. METHODS: This is a retrospective cohort study including all elderly patients (>60 years) admitted to an intensive care unit in Fortaleza, Brazil, from January to December 2007. A comparison between survivors and nonsurvivors was done and the risk factors for death were investigated through univariate and multivariate analysis. RESULTS: A total of 84 patients were included, with an average age of 73 ± 7.6 years; 59% were female. Mortality was 62.8%. The main cause of death was multiple organ dysfunction (42.3%), followed by septic shock (36.5%) and cardiogenic shock (9.7%). Complications during intensive care unit ICU stay associated with death were respiratory failure (OR=61, p<0.001), acute kidney injury (OR=23, p<0.001), sepsis (OR=12, p<0.001), metabolic acidosis (OR=17, p<0.001), anemia (OR=8.6, p<0.005), coagulation disturbance (OR=5.9, p<0.001) and atrial fibrillation (OR=4.8, p<0.041). Independent risk factors for death were age (OR=1.15, p<0.005), coma (OR=7.51, p<0.003), hypotension (OR=21.75, p=0.003), respiratory failure (OR=9.93, p<0.0001) and acute kidney injury (OR=16.28, p<0.014). CONCLUSION: Mortality is high among critically ill elderly patients. Factors associated with death were age, coma, hypotension, respiratory failure and acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):153-158
DOI 10.1590/S0103-507X2010000200009
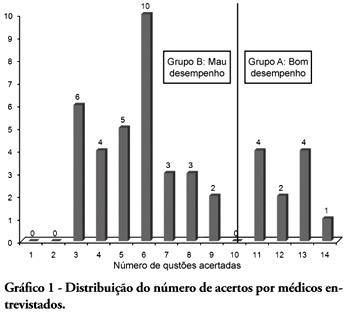
BACKGROUND: The main causes of cardiopulmonary arrest are endemic, and require constant medical improvement on cardiopulmonary resuscitation techniques. Training and continued education are essential to skilled management of cardiopulmonary resuscitation. OBJECTIVE: This study aimed to evaluate the physicians' theoretical knowledge on diagnosis and treatment of cardiopulmonary arrest. METHODS: This was a cross-sectional descriptive research conducted in a general hospital in Roraima, Brazil. The study population consisted of physicians who worked in the emergency department and intensive care units. The data were collected using a questionnaire addressing the subject. RESULTS: Forty four physicians answered the questionnaire. The mean score was 50% right answers. Most (88.5%) respondents committed "fatal errors". Half of the sample was never trained in advanced life support skills. No correlation was found between the number of right answers and attendance to advanced life support training courses. An inverse correlation was found between performance and age, but no statistically significant correlation was seen regarding performance and time from medical graduation. CONCLUSION: The physicians' theoretical knowledge on this field is worrisome. The results point to the importance of professional advanced life support training in order to assure quality standards for cardiac arrest management in this general hospital.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):159-165
DOI 10.1590/S0103-507X2010000200010
OBJECTIVE: Neonates mechanic ventilation weaning has become a major clinical challenge, and constitutes a large portion of neonatal intensive care units workload. The spontaneous breathing trial (SBT), performed immediately before extubation, can provide useful information on the patient's spontaneous breathing ability. This study aimed to assess the SBT effectiveness for extubation success prediction in mechanically ventilated preterm infants. METHODS: After Ethics Committee approval, an observational, longitudinal, prospective study was conducted. A sample of 60 preterm infants compliant with the weaning criteria was categorized in two groups: 'SBT' group (n=30), with the patients who underwent 30 minutes spontaneous breathing trial (SBT) with continuous positive pressure airway (CPAP), and the control group (n=30) where the extubation was performed without spontaneous breathing trial. The heart rate (HR), respiratory rate (RR), pulse oxymetry oxygen saturation (SpO2) and the Silverman-Andersen score were recorded before and 10, 20 and 30 minutes after the spontaneous breathing trial. Were also assessed for both groups, and versus extubation success or failure, the weight, gestational age, Apgar score, mean airway pressure, inspired oxygen concentration, and tracheal tube time. The Chi-square test was used for categorical variables and the Mann-Whitney test for non-normal distribution. Extubation success was defined as a 48 hours period with no reintubation requirement. RESULTS: No significant differences were identified between the groups for the analyzed variables, except for the mean airway pressure. A significant association was shown between spontaneous breathing trial and successful extubation. CONCLUSION: The significant association between SBT and extubation success may contribute for prediction of successful weaning in preterm infants.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):166-174
DOI 10.1590/S0103-507X2010000200011
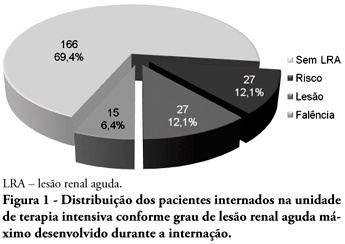
OBJECTIVES: Acute kidney injury is characterized by sudden and generally revertible renal function impairment involving inability to maintain homeostasis. In pediatrics, the main causes of acute kidney injury are sepsis, use of nephrotoxic drugs and renal ischemia in critically ill patients. The incidence of acute kidney injury in these patients ranges from 20 to 30%, resulting in increased morbid-mortality, a 40 to 90% rate. This study aimed to evaluate the incidence of acute kidney injury in intensive care unit patients, to categorize the severity of the acute kidney injury according to the Pediatric Risk, Injury, Failure, Loss, End-Stage (pRIFLE), examine the relationship between the acute kidney injury and severity using the Pediatric Index of Mortality (PIM) and to analyze outcome predictors. METHODS: A prospective study of the patients admitted to the intensive care unit of Hospital Infantil Joana de Gusmão - Florianópolis / SC - Brazil was conducted between July 2008 and January 2009. Were evaluated daily the urine output and serum creatinine, and the patients were categorized according to the pRIFLE criteria. RESULTS: During the follow-up period, 235 children were admitted. The incidence of acute kidney injury was 30.6%, and the maximal pRIFLE score during hospitalization was 12.1% for R, 12.1% for I and 6.4% for F. The mortality rate was 12.3%. The patients who developed acute kidney injury had a ten times bigger risk of death versus the not exposed patients. CONCLUSIONS: Acute kidney injury is frequent in critically ill patients. Early diagnosis and prompt and appropriate therapy for each clinical aspect may change this condition's course and severity, and reduce the patients' morbidity and mortality.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):192-195
DOI 10.1590/S0103-507X2010000200014
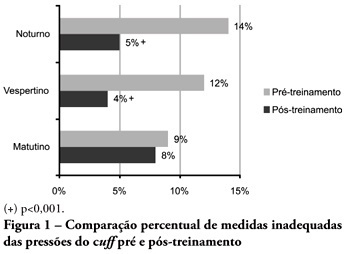
OBJECTIVES: Direct cuff pressure to the tracheal wall can cause damage. This paper aimed to verify the effectiveness of nursing team training on cuff pressure control. METHODS: A retrospective survey was initially made on the records of cuff pressure measurements from January 2007 to June 2008 and the inadequacy percent was verified. Next, a nursing team training program was provided involving all nursing shift teams during June 2008, and after the training the appropriate cuff pressures proportion was prospectively recorded between June and December 2008. The proportion of inappropriate cuff pressure was compared between the work shifts (morning, afternoon and evening-night) and between pre- and post-training, using the qualitative Chi-square test. The 5% limit (p<0.05) was considered for significant differences. RESULTS: For the pre-training period, inappropriate cuff pressure measures (over 30cmH2O) during morning, afternoon and evening-night shifts were 9.2%, 11.9% and 13.7%, respectively. For the post-training phase, 7.6%, 4.1% and 5.2% inappropriate cuff-pressures were identified for the morning, afternoon and evening-night shifts, respectively, with a significant reduction for the afternoon and evening-night shifts, respectively (p<0.001). CONCLUSION: Nursing team training was effective for inadequate cuff pressure harms awareness improvement, and resulted in safer pressure levels.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):186-191
DOI 10.1590/S0103-507X2010000200013
OBJECTIVES: To evaluate the applicability of the bag squeezing and zeep maneuvers in mechanically ventilated patients. METHODS: Twenty stable mechanically ventilated patients were studied. All patients were randomly allocated to either bag squeezing techinique followed by zeep maneuver, or the reversed sequence. Each group crossed to the other sequence four hours later. Heart rate, respiratory rate, peripheral oxygen saturation and blood pressure were measured before, during and after each technique use. The suctioned secretions were collected and measured. The data were analyzed by pairwise statistical analysis for inter-group comparisons, and ANOVA for each group results analysis. RESULTS: The heart rate was significantly increased, from 92.6 ± 18.3 bpm to 99.8 ± 18.5 bpm and the peripheral oxygen saturation significantly decreased from 96.9 ± 3.0% to 94.5 ± 4.3% during the bag squeezing maneuver, although the values remained within the normal range. No significant changes were seen for the zeep maneuver. Peripheral oxygen saturation during the maneuvers was found to change when the techniques were compared. No differences were found for the suctionedsecretions amounts. CONCLUSION: The results suggest that both techniques are feasible as they cause few hemodynamic changes, and both are effective for bronchial secretions removal.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):5-10
DOI 10.1590/S0103-507X2010000100003
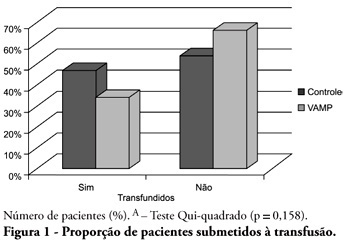
OBJECTIVE: Anemia is common in severely ill patients, and blood sampling plays a relevant causative role. Consequently, blood transfusions are frequent an related to several complications. Trying to reduce the transfusion-related risk, minimizing blood loss is mandatory. Thus, this work aimed to evaluate a closed blood sampling system as a strategy to spare unnecessary blood losses and transfusions. METHODS: This was a prospective, randomized, controlled, multicenter, 6 months, clinical trial. The patients were assigned to either VAMP (Venous Arterial Blood Management Protection) group, using a closed blood sampling system, or control group. The groups' transfusion rate, as well as hemoglobin (Hb) and Hematocrit (Ht) changes were compared for 14 days. RESULTS: Were included 127 patients, 65 assigned to the control group, and 62 to VAMP. During the intensive care unit stay, both groups experienced both hemoglobin and hematocrit drops. However, when the final Ht and Hb were compared between the groups, a difference was identified with higher values in the VAMP group (p=0.03; p=0.006, respectively). No statistical difference was found for both groups transfusion rates, although the VAMP group had an absolute 12% blood transfusion reduction. CONCLUSION: The use of a closed blood sampling system was able to minimize blood count values changes, however failed to reduce transfusions rate.
Abstract
Rev Bras Ter Intensiva. 2010;22(1):11-18
DOI 10.1590/S0103-507X2010000100004
OBJECTIVE: This study aimed to evaluate the outcome of cirrhotic patients admitted to Intensive Care Unit. METHODS: We conducted a prospective cohort of cirrhotic patients admitted to two intensive care unit between June 1999 to September 2004. We collected demographic, comorbid conditions, diagnosis, vital signs, laboratory data, prognostic scores and evolution in intensive care unit and hospital. The patients were divided in groups: non surgical, non liver surgery, surgery for portal hypertension, liver surgery, liver transplantation, and urgent surgery. RESULTS: We studied 304 patients, which 190 (62.5%) were male. The median of age was 54 (47-61) years. The mortality rate in intensive care unit and hospital were 29.3 and 39.8%, respectively, more elevated than in the other patients admitted critically ill patients (19.6 and 28.3%; p<0.001). Non surgical patients and those submitted to urgent surgery presented high mortality rate in the intensive care unit (64.3 and 65.4%) and in the hospital (80.4 and 76.9%). The variables related to hospital mortality were [Odds ratio (confidence interval 95%)]: mean arterial pressure [0.985 (0.974-0.997)]; mechanical ventilation in the first 24 h [4.080 (1.990-8.364)]; confirmed infection in the first 24 h [7.899 (2.814-22.175)]; acute renal failure [5.509 (1.708-17.766)] and APACHE II score (points) [1.078 (1.017-1.143)]. CONCLUSIONS: Cirrhotic patients had higher mortality rate compared to non cirrhotic critically ill patients. Those admitted after urgent surgery and non surgical had higher mortality rate.