Abstract
Rev Bras Ter Intensiva. 2010;22(3):270-273
DOI 10.1590/S0103-507X2010000300009
OBJECTIVE: To evaluate the prevalence of gastrointestinal complications and protein-calorie adequacy in critical patients using enteral nutrition therapy. METHODS: This was a retrospective study in the intensive care unit of the Hospital das Clinicas of the Universidade Federal de Pernambuco involving analysis of nutritional records evaluating the most frequent gastrointestinal complications during the patients' hospitalization and protein-calorie supply requirements. It was considered offered, the volume and formula effectively received by the patient on the last hospitalization day. The SPSS version 13 software was used for statistical analysis. RESULTS: The sample consisted of 77 patients aged in average 54.7 ± 18.1 years who were predominantly female (54.5%). The diet offered was appropriate and all patients had some type of gastrointestinal complications, being high gastric residuals the most prevalent (39%), followed by constipation (36.4%). CONCLUSION: Despite the high prevalence of gastrointestinal complications, no mismatches were observed in protein-calorie intake. Multidisciplinary approaches to these complications should be standardized in order to provide their early resolution.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):144-152
DOI 10.1590/S0103-507X2010000200008
OBJECTIVE: To know and compare the patterns of antimicrobials use in intensive care units (ICUs) based on the Anatomical Therapeutic Chemical/Defined Daily Dose (ATC/DDD) system. METHODS: a prospective cohort study was conducted in three medical-surgical intensive care units, two of them in public hospitals and one in a private hospital. Simple random, independent samples of patients admitted from 10/2004 to 09/2005 to the selected intensive care units were used. The antibiotics use was assessed using the ATC/DDD system. The amount of antibacterials used in each intensive care unit, in grams, was transformed in daily defined dose (DDD). The number of DDDs was divided by the number of patient-days, multiplied by one thousand, to obtain the average density of consumption (DC) per thousand patient-days (DDD1000). RESULTS: 1,728 patients-days and 2,918.6 DDDs were examined in the three intensive care units, corresponding to an average density of consumption of 1,689.0 DDD1000. The median number of DDDs of antibiotics use in the public hospitals’ intensive care units was significantly higher (p=0.002) versus the private hospital’s intensive care unit. The consumption of antibiotics in the private hospital’s intensive care unit (DC=2,191.7 DDD1000) was significantly higher (p<0.001) versus the intensive care units of public hospitals (1,499.5 DDD1000). The most used antibiotics groups in the three intensive care units were 3rd generation cephalosporins, penicillins/betalactamases inhibitors, carbapenems and fluorquinolones. CONCLUSION: The pattern of antibiotics use in the three examined intensive care units was not uniform. The private hospital’s intensive care unit used a significantly larger amount versus the public hospitals’ intensive care units. Nevertheless, the most used antibiotics groups were similar in the three intensive care units.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):175-185
DOI 10.1590/S0103-507X2010000200012
OBJECTIVE: The avoidance of pressure ulcers development in critically ill patients is a major nursing challenge. Prevention is thus relevant for assurance of high quality care. This study aimed to evaluate the applicability of the Braden scale in intensive care unit patients. METHODS: This was a prospective study based which evaluated all adult patients staying in the intensive care unit from July 14 to August 10, 2009. The data were collected using the Braden's scale by three examiners who identified the pressure ulcer development risk. The data were analyzed using the SAS Statistical Software. For determination of the examiners' rates degree of coincidence, the Kappa value was used (95%CI). RESULTS: Regarding the related risk factors: 36.4% had mild sensory perception impairment; 50.9% had occasionally moist skin; 97.3% bedfast; 39.1% had very limited mobility; 45% probably had inappropriate nutrition; 61.8% had friction and shear problems. An agreement between the examiners was identified for nutrition and physical activity (38.1% to 100.0%); the Kappa population zero hypothesis was rejected; a paired examiners agreement (41.7% to 100.0%) was identified for the items humidity and physical activity, and the Kappa values ranged from 0.13 to 1. CONCLUSIONS: These intensive care patients were identified to have increased risk of developing pressure ulcers. This tool was considered appropriate to support the implementation of preventive measures.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):103-111
DOI 10.1590/S0103-507X2010000200002
OBJECTIVES: To assess the physician’s knowledge on intubation techniques and to identify the common practices. METHODS: This was a prospective study, involving three different intensive care units within a University hospital: Anesthesiology (ANEST), Pulmonology (PULMO) and Emergency Department (ED). All physicians working in these units and consenting to participate in the study completed a questionnaire with their demographic data and questions on orotracheal intubation. RESULTS: 85 completed questionnaires were retrieved (90.42% of the physicians). ANEST had the higher mean age (p=0.001), being 43.5% of them intensivists. The use of hypnotic and opioid association was reported by 97.6%, and pre-oxygenation by 91.8%, but only 44.6% reported sub-occipital pad use, with no difference between the ICUs. On ANEST an increased neuromuscular blockade use was reported (p<0.000) as well as increased caution with full stomach (p=0.002). The rapid sequence knowledge was restricted (mean 2.20 ± 0.89), p=0.06 between the different units. The Sellick maneuver was known by 97.6%, but 72% used it inappropriately. CONCLUSIONS: Physicians knowledge on orotracheal intubation in the intensive care unit is unsatisfactory, even among qualified professionals. It is necessary to check if the responses to the questionnaire and actual clinical practices agree.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):112-117
DOI 10.1590/S0103-507X2010000200003
OBJECTIVES: Communication issues between healthcare professionals in intensive care units may be related to critically ill patients’ increased mortality. This study aimed to evaluate if communication issues involving assistant physicians and routine intensive care unit physicians would impact critically ill patients’ morbidity and mortality. METHODS: This was a cohort study that included non-consecutive patients admitted to the intensive care unit for 18 months. The patients were categorized in 3 groups according to their assistant doctors’ versus routine doctors communication uses: DC - daily communication during the stay (>75% of the days); EC - eventual communication (25 to 75% of the days); RC - rare communication (< 25% of the days). Demographic data, severity scores, reason for admission to the intensive care unit and interventions were recorded. The consequences of the medical professionals communication failures (delayed procedures, diagnostic tests, antibiotics, ventilatory weaning, vasopressors) and medical prescriptions inadequacies (no bed head elevation, no stress ulceration and deep venous thrombosis drug prophylaxis), and their relationship with the patients outcomes were analyzed. RESULTS: 792 patients were included, and categorized as follows: DC (n=529); EC (n=187) and RC (n=76). The mortality was increased in the RC patients group (26.3%) versus the remainder groups (DC = 13.6% and EC = 17.1%; p<0.05). A multivariate analysis showed that delayed antibiotics [RR 1.83 (CI95%: 1.36 -2.25)], delayed ventilatory weaning [RR 1.63 (CI95%: 1.25-2.04)] and no deep venous thrombosis prophylaxis [RR 1.98 (CI95%: 1.43 - 3.12)] contributed independently for the increased mortality. CONCLUSION: The failure in the assistant and routine intensive care doctors communication may increase the patients’ mortality, particularly due to delayed antibiotics and ventilation weaning, and lack of deep venous thrombosis prophylaxis prescription.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):118-124
DOI 10.1590/S0103-507X2010000200004
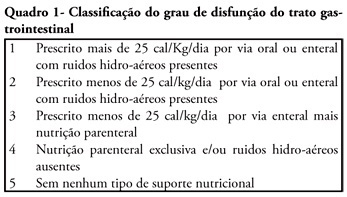
OBJECTIVE: We aimed to investigate the prevalence and independent predictors of prolonged gastrointestinal dysfunction in critically ill patients admitted to the intensive care unit. METHODS: Retrospective and observational cohort study performed in a mixed 24 beds intensive care unit in a tertiary center. Patients admitted in the intensive care unit between August 2003 and January 2004, who had a length of stay in the intensive care unit greater than 4 days were enrolled. Gastrointestinal function was evaluated daily according to a classification that considered physical examination (bowel sounds or distension) and the nutritional support progress. RESULTS: Were included 128 patients. The mean age was 56 ± 19 years, 63.3% were male and 77.3% were surgical patients. Prolonged gastrointestinal dysfunction occurred in 35% of patients, with prevalence 3.3 times higher in surgical patients (27%) than in medical patients (8%). Endoscopies were performed in 38 patients (29.7%), and in three quarters of them erosive lesions and or bleeding were observed. Gastrointestinal dysfunction was more frequent in patients presenting moderate or severe edema (51%) than in patients without edema (22.5%) (p<0.05). In the logistic regression analysis, a serum lactate level higher than 5.2 mEq/L (RR 6.69 95%CI 15-38.7, P = 0.034) and the presence of a low oxygenation index (RR 12.4 95%CI 2.18-70.8, p = 0.005) were predictive of gastrointestinal dysfunction. CONCLUSION: Prolonged gastrointestinal dysfunction was highly prevalent in this heterogeneous population of critically ill patients. Admission high serum lactate levels and a low oxygenation index were predictive of prolonged gastrointestinal dysfunction.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):125-132
DOI 10.1590/S0103-507X2010000200005
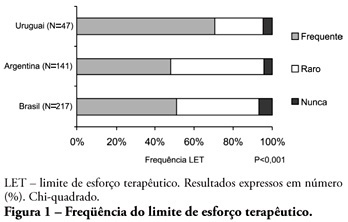
ABSTRACT OBJECTIVE: To evaluate end-of-life procedures in intensive care units. METHODS: A questionnaire was prepared by the End-of-Life Study Group of the Argentinean, Brazilian and Uruguayan Intensive Care societies, collecting data on the participants’ demographics, institutions and limit therapeutic effort (LTE) decision making process. During this cross sectional study, the societies’ multidisciplinary teams members completed the questionnaire either during scientific meetings or online. The variables were analyzed with the Chi-square test, with a p<0.05 significance level. RESULTS: 420 professionals completed the questionnaire. The Brazilian units had more beds, unrestricted visit was less frequent, their professionals were younger and worked more recently in intensive care units, and more non-medical professionals completed the questionnaire. Three visits daily was the more usual number of visits for the three countries. The most influencing LTE factors were prognosis, co-morbidities, and therapeutic futility. In the three countries, more than 90% of the completers had already made LTE decisions. Cardiopulmonary resuscitation, vasoactive drugs administration, dialysis and parenteral nutrition were the most suspended/refused therapies in the three countries. Suspension of mechanic ventilation was more frequent in Argentina, followed by Uruguay. Sedation and analgesia were the less suspended therapies in the three countries. Legal definement and ethical issues were mentioned as the main barriers for the LTE decision making process. CONCLUSION: LTE decisions are frequent among the professionals working in the three countries’ intensive care units. We found a more proactive LTE decision making trend In Argentina, and more equity for decisions distribution in Uruguay. This difference appears to be related to the participants’ different ages, experiences, professional types and genders.
Abstract
Rev Bras Ter Intensiva. 2010;22(2):133-137
DOI 10.1590/S0103-507X2010000200006
STUDY OBJECTIVE: Obese patients seem to have worse outcomes and more complications during intensive care unit (ICU) stay. This study describes the clinical course, complications and prognostic factors of obese patients admitted to an intensive care unit compared to a control group of nonobese patients. DESIGN: Retrospective observational study. SETTING: A 10-bed adult intensive care unit in a university-affiliated hospital. METHODS: All patients admitted to the intensive care unit over 52 months (April 01/2005 to November 30/2008) were included. Obese patients were defined as those with a body mass index (BMI) ≥ 30 Kg/M2. Demographic and intensive care unit related data were also collected. An clinical and demographical matching group of eutrophic patients selected from the data base as comparator for mortality and morbidity outcomes. The Mann-Whitney test was used for numeric data comparisons and the Chi Square test for categorical data comparisons. RESULTS: Two hundred nineteen patients were included. The obese group (n=73) was compared to the eutrophic group (n= 146). Most of this group BMI ranged between 30 - 35 Kg/M2. Only ten patients had body mass index ≥40 Kg/M2. Significant differences between the obese and eutrophic groups were observed in median APACHE II score (16 versus 12, respectively; p<0.05) and median intensive care unit length of stay (7 versus 5 days respectively; p<0,05). No significant differences were seen regarding risk of death, mortality rate, mechanical ventilation needs, days free of mechanical ventilation and tracheostomy rates. The observed mortality was higher than the APACHE II-predicted for both groups, but the larger differences were seen for morbid obese patients (BMI ≥40 Kg/M2). CONCLUSIONS: Obesity did not increase the mortality rate, but improved intensive care unit length of stay. The current prognostic scoring systems do not include BMI, possibly underestimating the risk of death, and other quality of care indexes in obese patients. New studies could be useful to clarify how body mass index impacts the mortality rate.