Abstract
Rev Bras Ter Intensiva. 2010;22(3):213-219
DOI 10.1590/S0103-507X2010000300001
OBJECTIVE: To analyze the economic impact of an early sepsis detection protocol in two general hospitals. METHODS: We analyzed data collected from a prospective study of septic patients before and after the implementation of a protocol for early diagnosis of severe sepsis. We conducted a cost-effectiveness analysis comparing: mortality rate, cost of sepsis treatment and indirect costs attributed to years of productive life lost to premature death in both phases. RESULTS: Two hundred seventeen patients were included, 102 in phase I and 115 in phase II. After protocol implementation, in private and public hospital, mortality rates decreased from 50% to 32.2% and from 67.6% to 41% (p < 0.05). The mean years of productive life lost due to sepsis decreased from 3.18 to 0.80 and 9.81 to 4.65 (p < 0.05), with a mean gain of 2.38 and 5.16 years of productive life, for each septic patient. Considering Brazilian gross domestic product per capita, estimated productivity loss due to sepsis decreased between 3.2 and 9.7 billion US dollars, varying based on the incidence of sepsis. Hospital costs were similar in both phases. CONCLUSION: A protocol for early detection and treatment of in-hospital septic patients is highly cost-effective from a societal perspective.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):220-228
DOI 10.1590/S0103-507X2010000300002
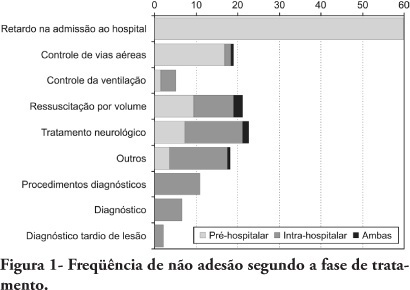
OBJECTIVES: To evaluate patients treated for traumatic injuries and to identify adherence to guidelines recommendations of treatment and association with death. The recommendations adopted were defined by the committee on trauma of the American College of Surgeons in advanced trauma life support. METHODS: Retrospective cohort study conducted at a teaching hospital. The study population was victims of trauma > 12 years of age with injury severity scores > 16 who were treated between January 1997 and December 2001. Data collection was divided into three phases: pre-hospital, in-hospital, and post-mortem. The data collected were analyzed using EPI INFO. RESULTS: We analyzed 207 patients, 147 blunt trauma victims (71%) and 60 (29%) penetrating trauma victims. Trauma victims had a 40.1% mortality rate. We identified 221 non adherence events that occurred in 137 patients. We found a mean of 1.61 non adherence per patient, and it occurred less frequently in survivors (1.4) than in non-survivors (1.9; p=0.033). According to the trauma score and injury severity score methodology, 54.2% of deaths were considered potentially preventable. Non adherence occurred 1.77 times more frequently in those considered potentially preventable deaths compared to other non-survivors (95% CI: 1.12-2.77; p=0.012), and 92.9% of the multiple non adherence occurred in the first group (p=0.029). CONCLUSIONS: Non adherence occurred more frequently in patients with potentially preventable deaths. Non adherence to guidelines recommendations can be considered a contributing factor to death in trauma victims and can lead to an increase in the number of potentially preventable deaths.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):229-235
DOI 10.1590/S0103-507X2010000300003
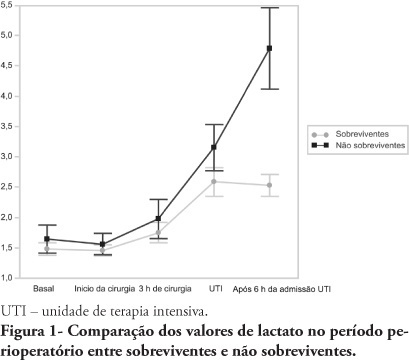
OBJECTIVES: An increased lactate level is classically considered a marker for poorer prognosis, however little information is available on intraoperative lactate's kinetics and its connection with prognosis. This study aimed to evaluate the time when perioperative lactate is most relevant for prognosis. METHODS: This was an observational prospective study conducted in a tertiary hospital. Patients with requested intensive care unit postoperative stay, aged > 18 years, undergoing major surgery were included. Palliative surgery patients and those with heart and/or severe liver failure were excluded. Arterial lactate levels were measured immediately before the surgery start (T0), after anesthesia induction (T1), 3 hours after the surgery start (T2), intensive care unit admission (T3) and 6 hours after the intensive care unit admission (T4). RESULTS: Sixty seven patients were included. The mean lactate values for the patients' T0, T1, T2 and T4 were 1.5 ± 0.8 mmol/L, 1.5 ± 0.7 mmol/L, 1.8 ± 1.2 mmol/L, 2.7 ± 1.7 mmol/L and 3.1 ± 2.0 mmol/L, respectively. The hospital mortality rate was 25.8%, and surviving and non-surviving patients lactate values in the intensive care unit were 2.5 ± 1. and 4.8 ± 2.8 mmol/L (P < 0.0001), respectively. The other times measurements showed no statistically significant differences between the groups. CONCLUSIONS: In surgical patients, intraoperative arterial lactate levels failed to show a predictive value; however during the postoperative period, this assessment was shown to be useful for hospital mortality prediction.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):236-244
DOI 10.1590/S0103-507X2010000300004
OBJECTIVES: Critically ill cancer patients are at increased risk for acute kidney injury, but studies on these patients are scarce and were all single centered conducted in specialized intensive care units. The objective was to evaluate the characteristics and outcomes in a prospective cohort of cancer patients admitted to several intensive care units with acute kidney injury. METHODS: Prospective multicenter cohort study conducted in intensive care units from 28 hospitals in Brazil over a two-month period. Univariate and multivariate logistic regression were used to identify factors associated with hospital mortality. RESULTS: Out of all 717 intensive care unit admissions, 87 (12%) had acute kidney injury and 36% of them received renal replacement therapy. Kidney injury developed more frequently in patients with hematological malignancies than in patients with solid tumors (26% vs. 11%, P=0.003). Ischemia/shock (76%) and sepsis (67%) were the main contributing factor for and kidney injury was multifactorial in 79% of the patients. Hospital mortality was 71%. General and renal-specific severity-of-illness scores were inaccurate in predicting outcomes for these patients. In a multivariate analysis, length of hospital stay prior to intensive care unit, acute organ dysfunctions, need for mechanical ventilation and a poor performance status were associated with increased mortality. Moreover, cancer-related characteristics were not associated with outcomes. CONCLUSIONS: The present study demonstrates that intensive care units admission and advanced life-support should be considered in selected critically ill cancer patients with kidney injury.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):245-249
DOI 10.1590/S0103-507X2010000300005
OBJECTIVE: Ischemic acute kidney injury (iLRA), with multifatorial cause, presents alarming morbidity and mortality. Statin, HMG-CoA inhibition reductase has shown a renoprotective effect, with antioxidant, antiinflamatory and vascular actions. The heme oxygenase-1 (HO-1) can be involved in these pleitropic effects of statin on the renal function. This study was performed in order to evaluate if the renoprotective effect of the statin is a heme mechanism of protection in rats. METHODS: The ischemic model was reproduced by through clamping the bilateral renal pedicles for 30 minutes followed by reperfusion. Adult Wistar rats, weighting from 250-300g, were divided into the following groups: SHAM (control); Ischemia (30 minutes renal ischemia); Ischemia+Statin (sinvastatin 0.5mg/kg,orally (v.o.) for 3 days); Ischemia+Hemin (Hemin, 1.0mg/100g, intraperitoneal (i.p.), 24 hours before surgery); Ischemia+SnPP (SnPP 2μmol/kg, i.p., 24 hours before surgery ); Ischemia+Statin+Hemin; Ischemia+Statin+SnPP. RF (clearance of creatinine, Jaffé method), urinary peroxides (UP), urinary osmolality (UO) and immunohistochemical for ED-1 were evaluated. RESULTS: Results showed that sinvastatin ameliorated RF, urinary osmolality, reduced the UP excrection and the macrophage infiltration in rats submitted to renal ischemia. The inducer of HO-1 and its association with sinvastatin induced a similar pattern of improvement of renal function. CONCLUSION: the study confirmed the renoprotective effect of the statins on renal function, with antioxidant and antiinflamatory actions, and it suggests that this effect can have an interface with the heme system of renal protection.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):250-256
DOI 10.1590/S0103-507X2010000300006
OBJECTIVE: The intensive care unit is synonymous of high severity, and its mortality rates are between 5.4 and 33%. With the development of new technologies, a patient can be maintained for long time in the unit, causing high costs, psychological and moral for all involved. This study aimed to evaluate the risk factors for mortality and prolonged length of stay in an adult intensive care unit. METHODS: The study included all patients consecutively admitted to the adult medical/surgical intensive care unit of Hospital das Clínicas da Universidade Estadual de Campinas, for six months. We collected data such as sex, age, diagnosis, personal history, APACHE II score, days of invasive mechanical ventilation orotracheal reintubation, tracheostomy, days of hospitalization in the intensive care unit and discharge or death in the intensive care unit. RESULTS: Were included in the study 401 patients; 59.6% men and 40.4% women, age 53.8±18.0. The mean intensive care unit stay was 8.2±10.8 days, with a mortality rate of 13.5%. Significant data for mortality and prolonged length of stay in intensive care unit (p <0.0001), were: APACHE II>11, OT-Re and tracheostomy. CONCLUSION: The mortality and prolonged length of stay in intensive care unit intensive care unit as risk factors were: APACHE>11, orotracheal reintubation and tracheostomy.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):257-263
DOI 10.1590/S0103-507X2010000300007
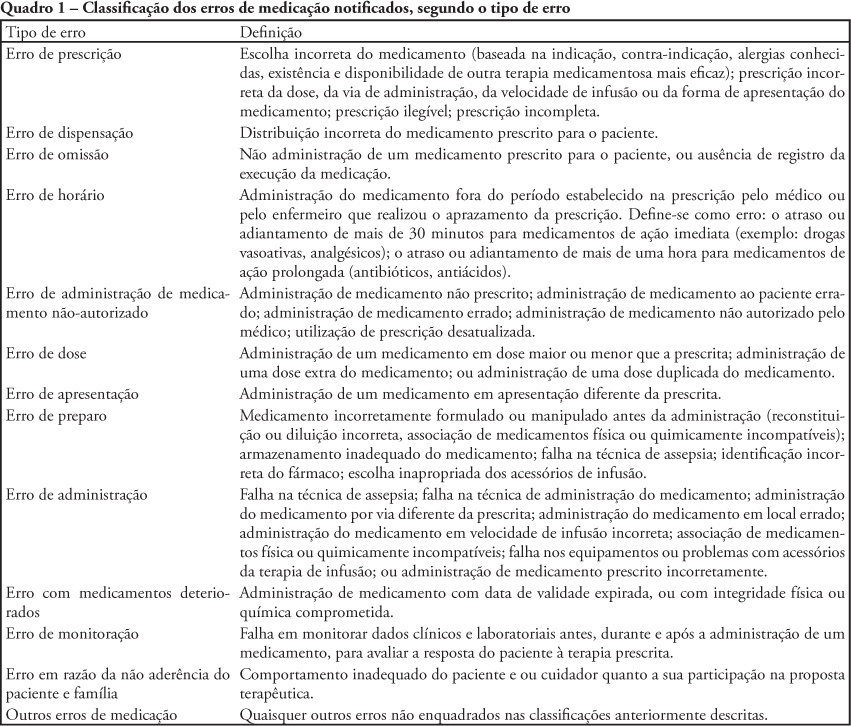
OBJECTIVE: To describe the frequency medication error disclosure to the team and to the family in an oncology pediatric patients' intensive care unit. METHODS: This was a descriptive and exploratory study performed between March 1 and May 31, 2008. A medication error report form was developed and implemented, to be completed by the professionals involved in the unit's medication process. RESULTS: The sample consisted of 71 forms collected over the 92 collection days. After medication error detection, the event was not reported to the pediatric intensive care unit's team in 34 (47.9%) cases. In the 37 reported to the team cases, for most of them (48.7%) the physician was the professional communicated. The event was not disclosed to the patient/family in 95.8% of medication error reports. CONCLUSIONS: Although the literature recommends disclosing the errors, this is not done in the studied pediatric intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2010;22(3):264-269
DOI 10.1590/S0103-507X2010000300008
OBJECTIVES: In mechanically ventilated patients, humidifier devices are used to heat and moisturize the inspired gas. Heating and humidifying inspired gas may prevent complications associated with the respiratory mucosa dryness such as mucus plugging and endotracheal tube occlusion. Two devices have been commonly used to this, either heated humidifier or the heat moisture exchange filter. This study aimed to compare the effects of the heated humidifier and a model of heat moisture exchange filter on respiratory mechanics in mechanically ventilated neurological patients. METHODS: This was a randomized crossover trial, involving 31 neurological patients under mechanical ventilation randomly assigned to the humidification devices. Expired tidal volume, peak inspiratory flow, peak expiratory flow, static compliance, dynamic compliance and respiratory system resistance were evaluated. Statistical analysis used the Kolmogorov-Smirnov test and Student's t test for paired samples, in which P values < 0.05 were considered significant. RESULTS: The heat moisture exchanger filter decreased expired tidal volume, peak inspiratory flow, peak expiratory flow (p < 0.001) and dynamic compliance (p = 0.002), and increased respiratory system resistance (p < 0.001). CONCLUSION: In the studied population, the use of a heat moisture exchange filter model leaded to several changes on respiratory mechanics parameters.