Abstract
Rev Bras Ter Intensiva. 2018;30(3):294-300
DOI 10.5935/0103-507X.20180046
To determine the risk factors for extubation failure in the intensive care unit.
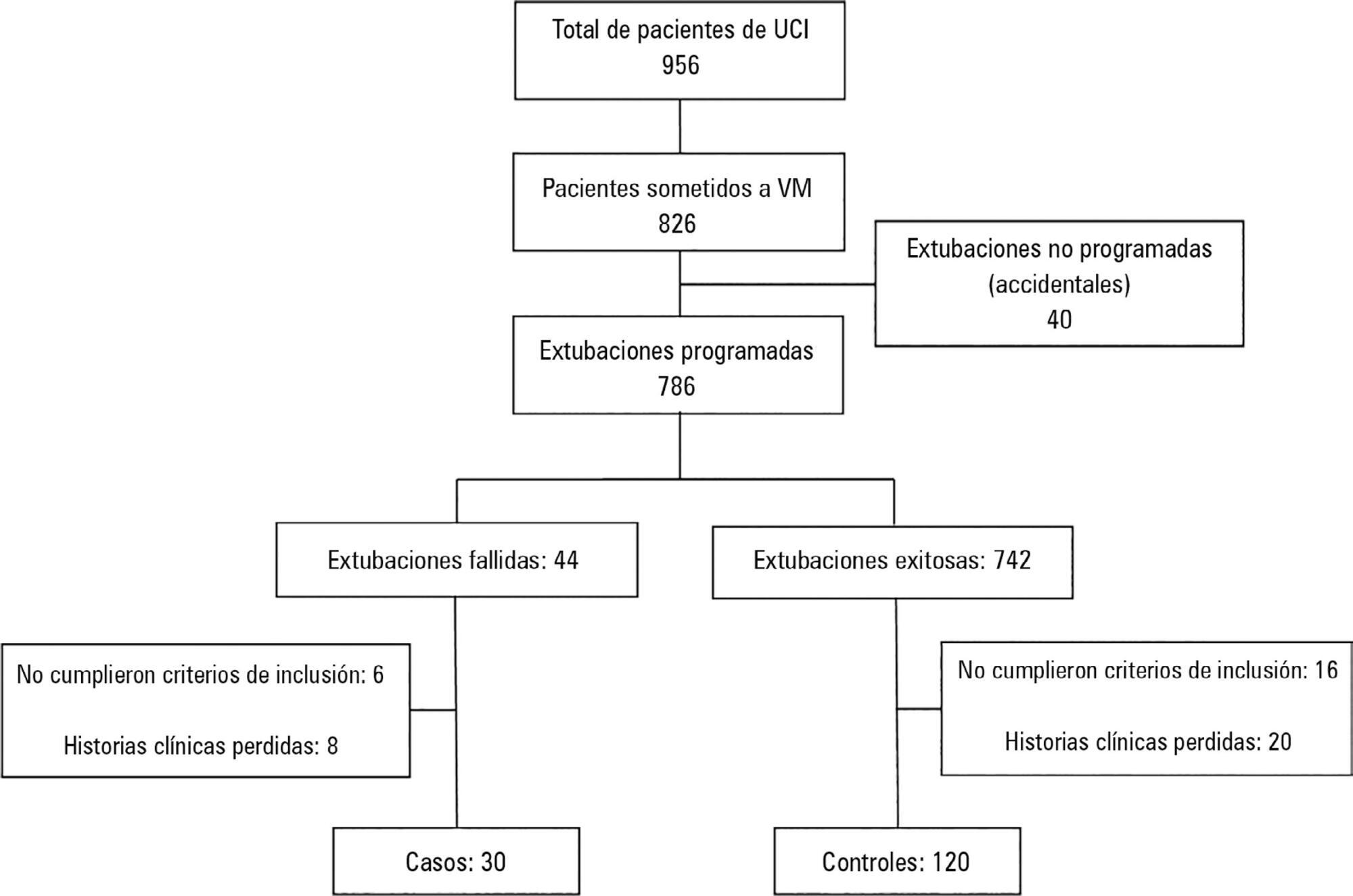
The present case-control study was conducted in an intensive care unit. Failed extubations were used as cases, while successful extubations were used as controls. Extubation failure was defined as reintubation being required within the first 48 hours of extubation.
Out of a total of 956 patients who were admitted to the intensive care unit, 826 were subjected to mechanical ventilation (86%). There were 30 failed extubations and 120 successful extubations. The proportion of failed extubations was 5.32%. The risk factors found for failed extubations were a prolonged length of mechanical ventilation of greater than 7 days (OR = 3.84, 95%CI = 1.01 - 14.56, p = 0.04), time in the intensive care unit (OR = 1.04, 95%CI = 1.00 - 1.09, p = 0.03) and the use of sedatives for longer than 5 days (OR = 4.81, 95%CI = 1.28 - 18.02; p = 0.02).
Pediatric patients on mechanical ventilation were at greater risk of failed extubation if they spent more time in the intensive care unit and if they were subjected to prolonged mechanical ventilation (longer than 7 days) or greater amounts of sedative use.
Abstract
Rev Bras Ter Intensiva. 2018;30(1):71-79
DOI 10.5935/0103-507X.20180013
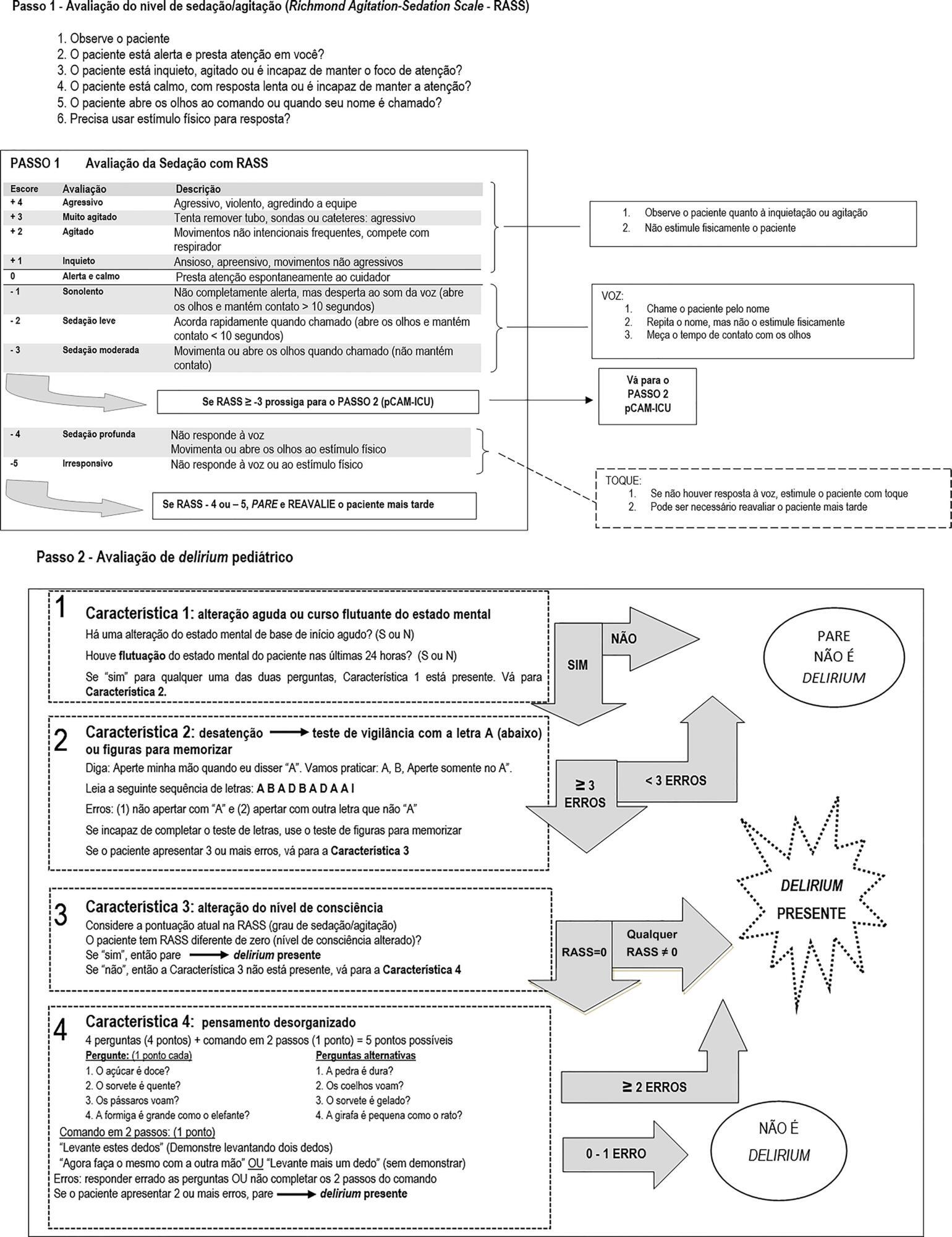
To undertake the translation and cross-cultural adaption into Brazilian Portuguese of the Pediatric Confusion Assessment Method for the Intensive Care Unit for the detection of delirium in pediatric intensive care units, including the algorithm and instructions.
A universalist approach for the translation and cross-cultural adaptation of health measurement instruments was used. A group of pediatric critical care specialists assessed conceptual and item equivalences. Semantic equivalence was evaluated by means of a translation from English to Portuguese by two independent translators; reconciliation into a single version; back-translation by a native English speaker; and consensus among six experts with respect to language and content understanding by means of Likert scale responses and the Content Validity Index. Finally, operational equivalence was assessed by applying a pre-test to 30 patients.
The back-translation was approved by the original authors. The medians of the expert consensus responses varied between good and excellent, except for the feature "acute onset" of the instructions. Items with a low Content Validity Index for the features "acute onset" and "disorganized thinking" were adapted. In the pre-test, the expression "signal with your head" was modified into "nod your head" for better understanding. No further adjustments were necessary, resulting in the final version for Brazilian Portuguese.
The Brazilian version of the Pediatric Confusion Assessment Method for the Intensive Care Unit was generated in agreement with the international recommendations and can be used in Brazil for the diagnosis of delirium in critically ill children 5 years of age or above and with no developmental cognitive disabilities.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):471-478
DOI 10.5935/0103-507X.20180068
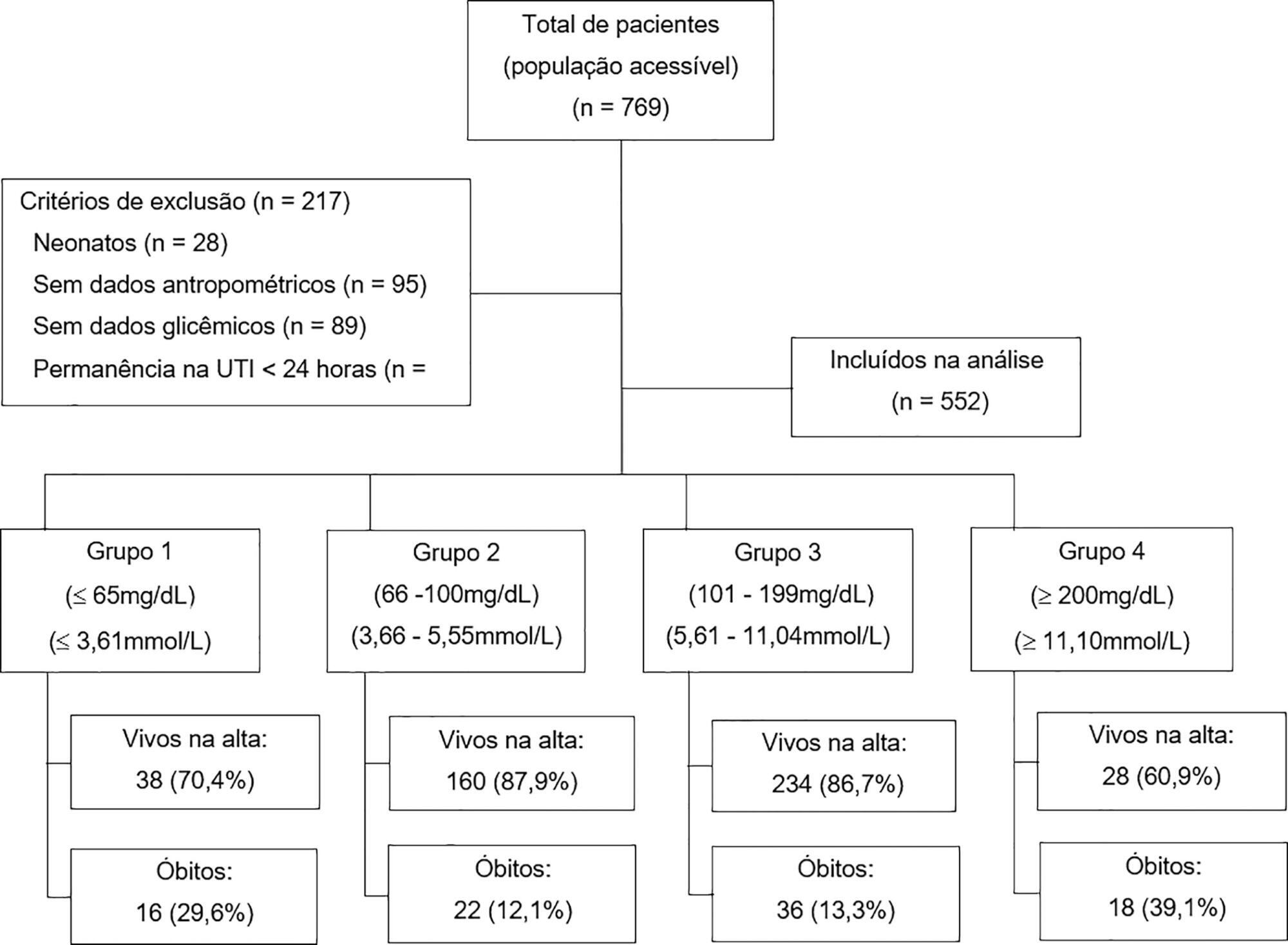
To analyze the association between glycemia levels upon pediatric intensive care unit admission and mortality in patients hospitalized.
A retrospective cohort of pediatric intensive care unit patients admitted to the Instituto Nacional de Salud del Niño between 2012 and 2013. A Poisson regression model with robust variance was used to quantify the association. Diagnostic test performance evaluation was used to describe the sensitivity, specificity, positive predictive value, negative predictive value and likelihood ratios for each range of glycemia.
In total, 552 patients were included (median age 23 months, age range 5 months to 79.8 months). The mean glycemia level upon admission was 121.3mg/dL (6.73mmol/L). Ninety-two (16.6%) patients died during hospitalization. In multivariable analyses, significant associations were found between glycemia < 65mg/dL (3.61mmol/L) (RR: 2.01, 95%CI 1.14 - 3.53), glycemia > 200mg/dL (> 11.1mmol/L) (RR: 2.91, 95%CI 1.71 - 4.55), malnutrition (RR: 1.53, 95%CI 1.04 - 2.25), mechanical ventilation (RR: 3.71, 95%CI 1.17 - 11.76) and mortality at discharge. There was low sensitivity (between 17.39% and 39.13%) and high specificity (between 49.13% and 91.74%) for different glucose cut-off levels.
There was an increased risk of death at discharge in patients who developed hypoglycemia and hyperglycemia upon admission to the pediatric intensive care unit. Certain glucose ranges (> 200mg/dL (> 11.1mmol/L) and < 65mg/dL (3.61mmol/L)) have high specificity as predictors of death at discharge.
Abstract
Rev Bras Ter Intensiva. 2017;29(4):460-465
DOI 10.5935/0103-507X.20170066
To evaluate the functional status of pediatric patients after discharge from the pediatric intensive care unit using the Functional Status Scale and to compare the time of invasive mechanical ventilation, length of stay in the pediatric intensive care unit, and Pediatric Index of Mortality 2 results among individuals with different degrees of functional impairment.
A cross-sectional study was conducted on patients who were discharged from a pediatric intensive care unit. The functional evaluation by the Functional Status Scale was performed on the first day after discharge from the unit, and the Pediatric Index of Mortality 2 was used to predict the mortality rate at the time of admission to the pediatric intensive care unit.
The sample consisted of 50 individuals, 60% of which were male, with a median age of 19 [6 - 61] months. The overall score of the Functional Status Scale was 11.5 [7 - 15], and the highest scores were observed in the "motor function" 3 [1 - 4] and "feeding" 4 [1 - 4] domains. Compared to patients who were not readmitted to the pediatric intensive care unit, patients who were readmitted presented a worse overall score (p = 0.01), worse scores in the "motor function" (p = 0.01), "feeding" (p = 0.02), and "respiratory" (p = 0.036) domains, and a higher mortality rate according to the Pediatric Index of Mortality 2 (p = 0.025).
Evaluation of the functional status using the Functional Status Scale indicated moderate impairment in patients after discharge from the pediatric intensive care unit, mainly in the "motor function" and "feeding" domains; patients who were readmitted to the pediatric intensive care unit demonstrated worse overall functional, motor function, feeding and respiratory scores. Individuals with greater functional impairment had longer times of invasive mechanical ventilation and hospitalization in the pediatric intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):335-340
DOI 10.5935/0103-507X.20160057
To evaluate the perceptions of physicians, nurses and nursing technicians of their participation in the decision-making process surrounding life support limitation in terminally ill pediatric patients, with comparisons by professional category.
A cross-sectional study was conducted in the pediatric intensive care unit of a tertiary public university hospital with the participation of physicians, nurses and nursing technicians. The MacArthur Admission Experience Survey Voice Scale was used to assess and quantify the perceptions of professionals who assisted 17 pediatric patients with life support limitation within 24 hours after the outcome of each patient was determined. All professionals working in the unit (n = 117) who were potentially eligible for the study received a free and informed consent form prior to the occurrence of the cases studied.
Study participants included 25/40 (62.5%) physicians, 10/17 (58.8%) nurses and 41/60 (68.3%) nursing technicians, representing 65% of the eligible professionals identified. The questionnaire return rate was higher for physicians than technicians (p = 0.0258). A perceived lack of voice was reported in all three professional categories at varying rates that were lower for physicians than for nurses and nursing technicians (p < 0.00001); there was no difference between the latter (p = 0.7016). In the three professional categories studied, three subscale items were reported. For two of the three statements, there were significant differences between physicians and nurses (p = 0.004) and between physicians and nursing technicians (p = 0.001). For one of the statements, there was no difference among the three professional categories.
Respondents perceived a lack of voice in the decision-making process at varying rates across the three categories of studied professionals who assisted terminally ill pediatric patients with life support limitation, with physicians expressing lowered rates of perceived coercion.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):270-277
DOI 10.5935/0103-507X.20160053
To estimate the prevalence of burnout in intensivist doctors working in adult, pediatric and neonatal intensive care units in five Brazilian capitals.
Descriptive epidemiological study with a random sample stratified by conglomerate with 180 intensivist doctors from five capitals representing the Brazilian geographic regions: Porto Alegre (RS), Sao Paulo (SP), Salvador (BA), Goiania (GO) and Belem (PA). A self-administered questionnaire examining sociodemographic data and the level of burnout was evaluated through the Maslach Burnout Inventory.
A total of 180 doctors were evaluated, of which 54.4% were female. The average age was 39 ± 8.1 years, 63.4% had specialization as the highest degree, 55.7% had up to 10 years of work experience in an intensive care unit, and 46.1% had the title intensive care specialist. Most (50.3%) had weekly workloads between 49 and 72 hours, and the most frequent employee type was salaried. High levels of emotional exhaustion, depersonalization and inefficacy were found (50.6%, 26.1% and 15.0%, respectively). The prevalence of burnout was 61.7% when considering a high level in at least one dimension and 5% with a high level in three dimensions simultaneously.
A high prevalence of burnout syndrome among intensivist doctors was observed. Strategies for the promotion and protection of health in these workers must be discussed and implemented in hospitals.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):472-482
DOI 10.5935/0103-507X.20160080
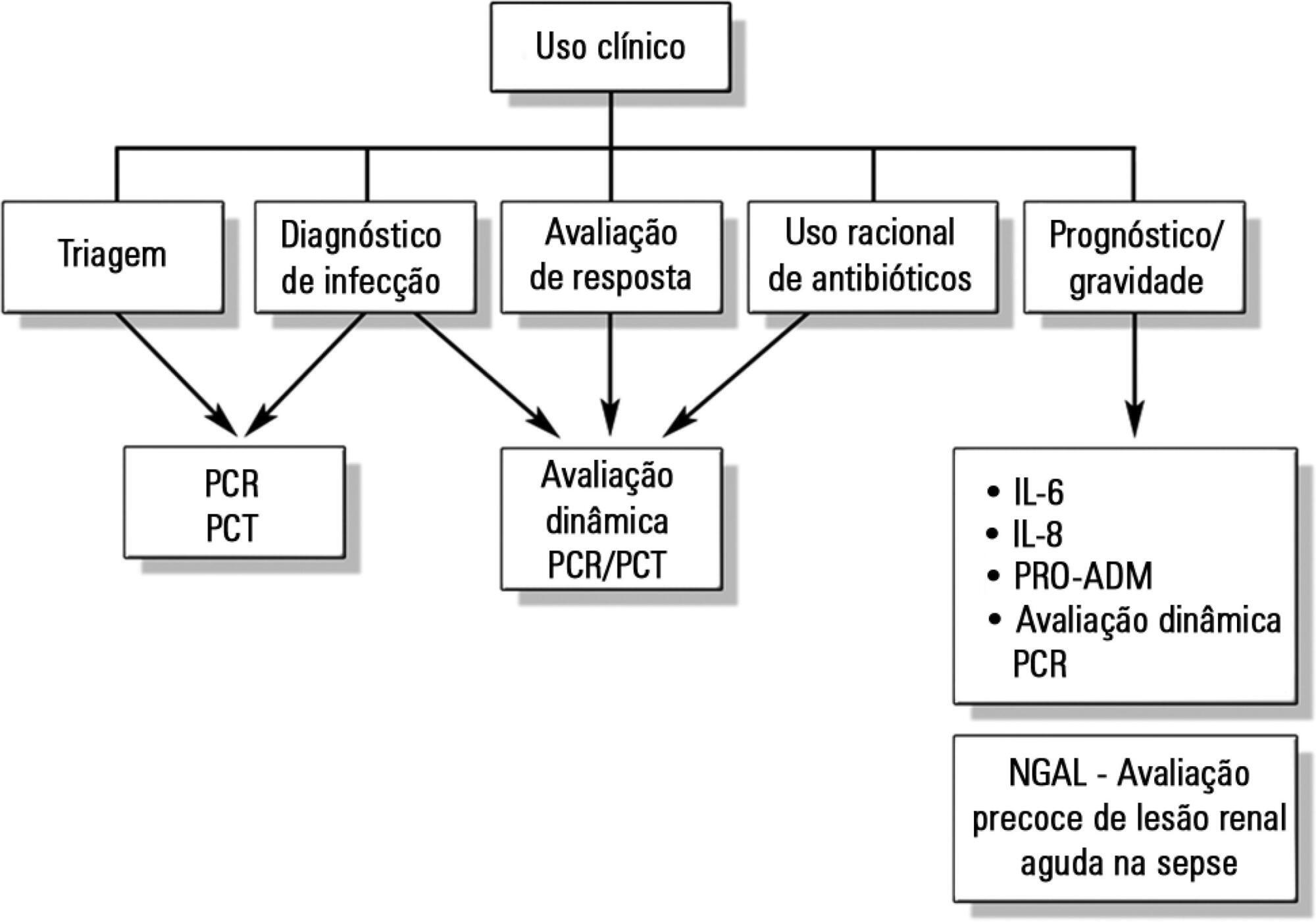
Despite advances in recent years, sepsis is still a leading cause of hospitalization and mortality in infants and children. The presence of biomarkers during the response to an infectious insult makes it possible to use such biomarkers in screening, diagnosis, prognosis (risk stratification), monitoring of therapeutic response, and rational use of antibiotics (for example, the determination of adequate treatment length). Studies of biomarkers in sepsis in children are still relatively scarce. This review addresses the use of biomarkers in sepsis in pediatric patients with emphasis on C-reactive protein, procalcitonin, interleukins 6, 8, and 18, human neutrophil gelatinase, and proadrenomedullin. Assessment of these biomarkers may be useful in the management of pediatric sepsis.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)