Abstract
Rev Bras Ter Intensiva. 2020;32(2):235-243
DOI 10.5935/0103-507X.20200038
To identify the neonatal, pediatric and mixed (neonatal and pediatric) intensive care units in Brazil that use cuffed tracheal tubes in clinical practice and to describe the characteristics related to the use of protocols and monitoring.
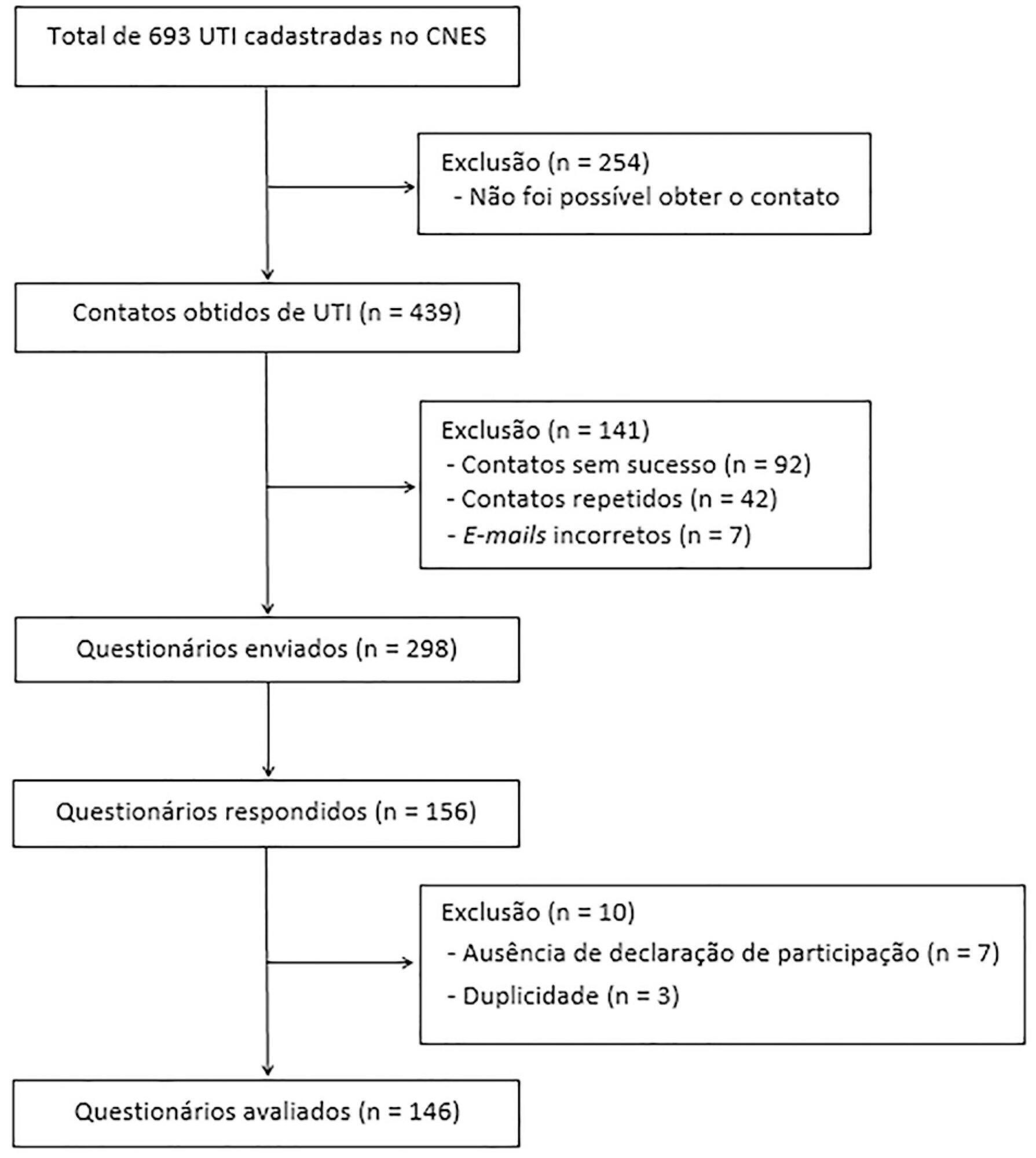
To identify the intensive care units in Brazil, the Ministry of Health’s National Registry of Health Facilities was accessed, and information was collected on 693 registered intensive care units. This was an analytical cross-sectional survey conducted through electronic questionnaires sent to 298 neonatal, pediatric and mixed intensive care units in Brazil.
This study analyzed 146 questionnaires (49.3% from neonatal intensive care units, 35.6% from pediatric intensive care units and 15.1% from mixed pediatric intensive care units). Most of the participating units (78/146) used cuffed tracheal tubes, with a predominance of use in pediatric intensive care units (52/78). Most of the units that used cuffed tracheal tubes applied a cuff pressure monitoring protocol (45/78). The use of cuff monitoring protocols was observed in intensive care units with a physical therapy service exclusive to the unit (38/61) and in those with a physical therapist present 24 hours/day (25/45). The most frequent cause of extubation failure related to the use of cuffed tracheal tubes in pediatric intensive care units was upper airway obstruction.
In this survey, the use of cuffed tracheal tubes and the application of a cuff pressure monitoring protocol was predominant in pediatric intensive care units. The use of a monitoring protocol was more common in intensive care units that had a physical therapist who was exclusive to the unit and was present 24 hours/day.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):261-267
DOI 10.5935/0103-507X.20200042
To evaluate the functional status of pediatric patients undergoing congenital heart surgery after discharge from the intensive care unit, and to evaluate the correlations among clinical variables, functional status and surgical risk.
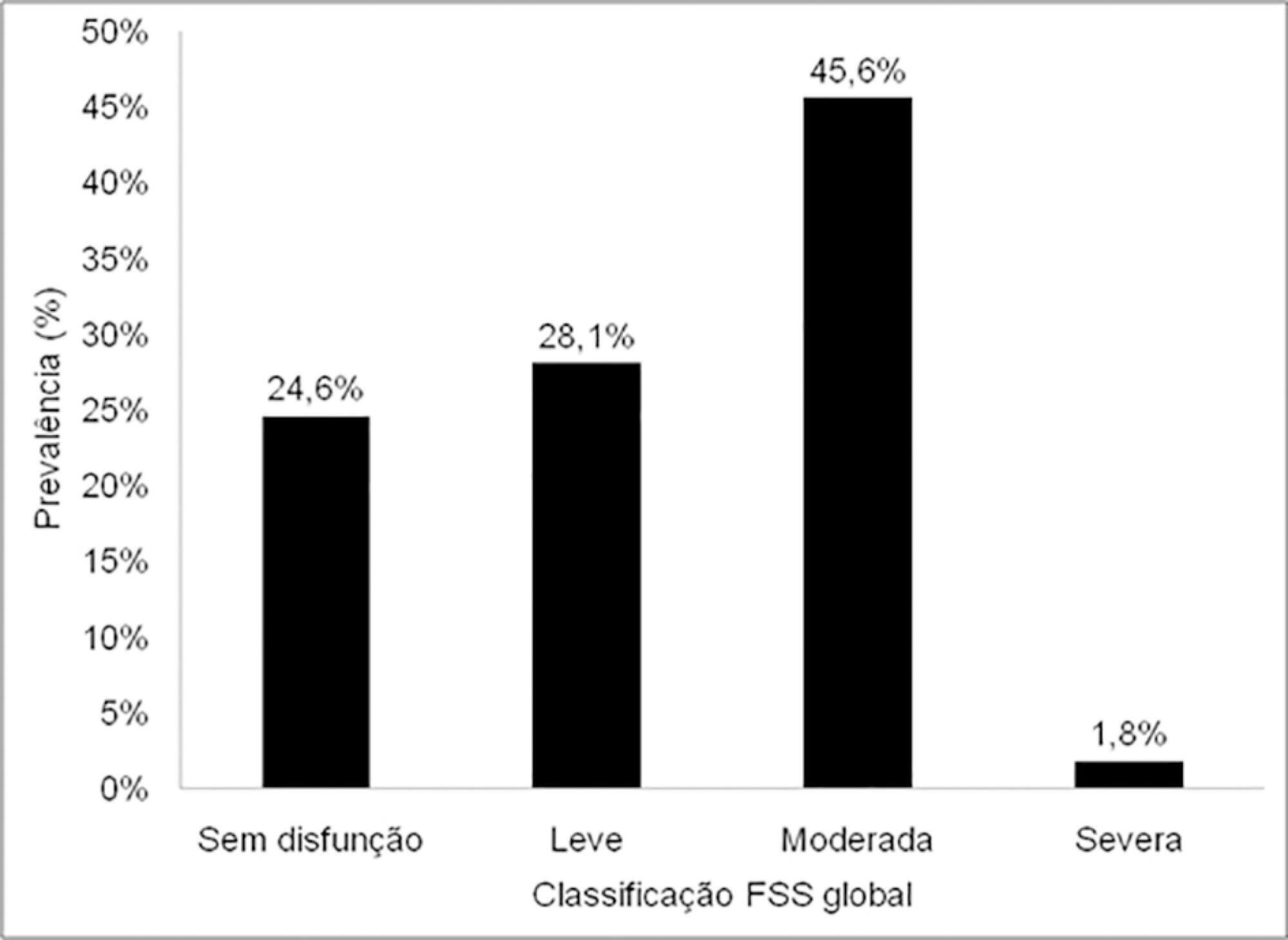
Cross-sectional study including patients aged 1 month to less than 18 years undergoing congenital heart surgery between October 2017 and May 2018. Functional outcome was assessed by the Functional Status Scale, surgical risk classification was determined using the Risk Adjustment for Congenital Heart Surgery-1 (RACHS-1), and clinical variables were collected from electronic medical records.
The sample comprised 57 patients with a median age of 7 months (2 - 17); 54.4% were male, and 75.5% showed dysfunction, which was moderate in 45.6% of the cases. RACHS-1 category > 3 was observed in 47% of the sample, indicating higher surgical risk. There was a correlation between functional deficit and younger age, longer duration of invasive mechanical ventilation and longer intensive care unit stay. Moreover, greater functional deficit was observed among patients classified as RACHS-1 category > 3.
The prevalence of functional deficit was high among children and adolescents with congenital heart disease after cardiac surgery. Higher surgical risk, longer duration of invasive mechanical ventilation, longer intensive care unit stay and younger age were correlated with worse functional status.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):295-300
DOI 10.5935/0103-507X.20200046
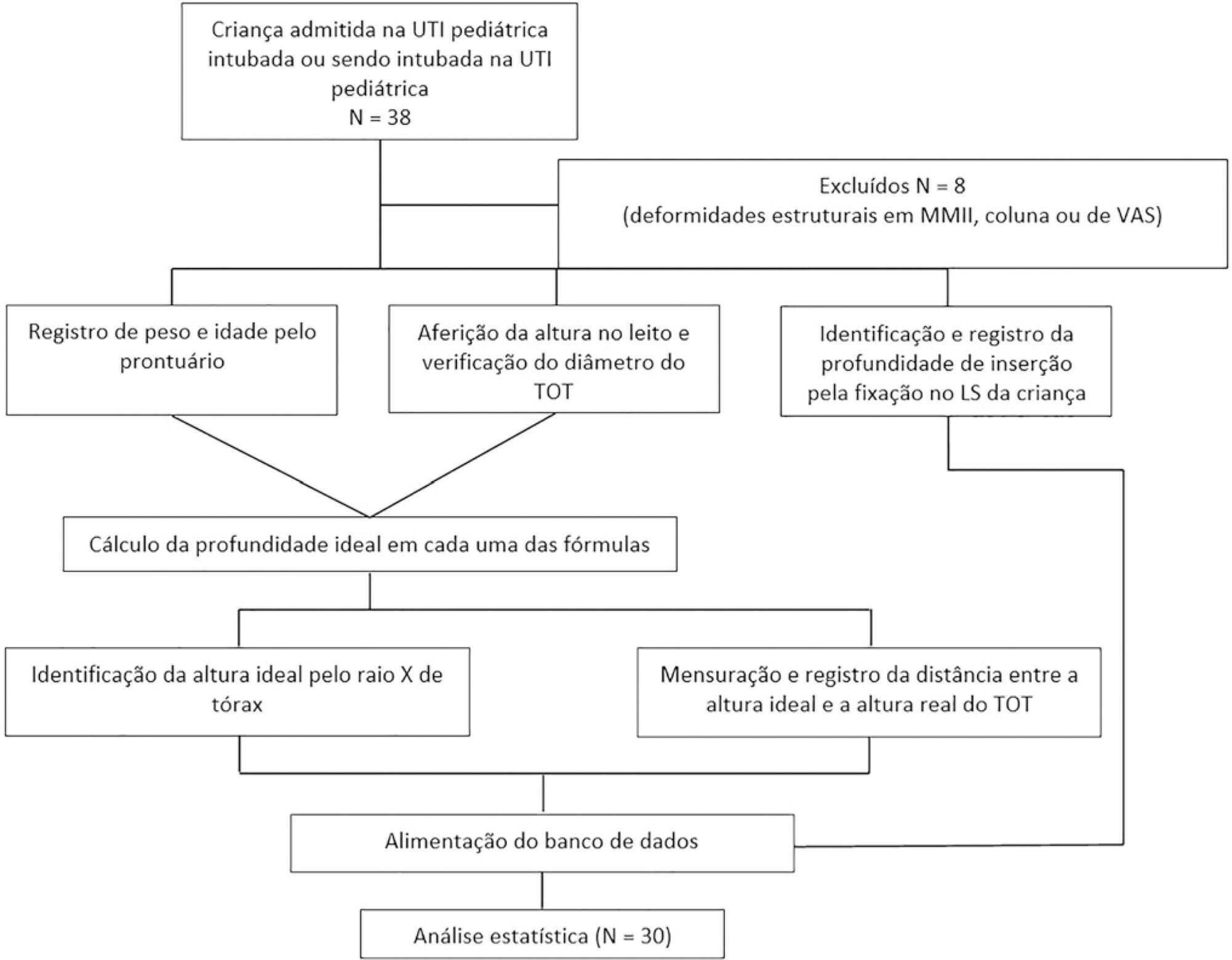
To evaluate the effectiveness of the different formulas for estimating the insertion depth of an endotracheal tube in children.
This was an observational and cross-sectional study that included children between 29 days and 2 years of age who were hospitalized in a pediatric intensive care unit and mechanically ventilated. The formulas based on height [(height/10) + 5], the inner diameter of the tube (endotracheal tube × 3), and weight (weight + 6) were evaluated to determine which of them showed better concordance with the ideal insertion depth of the endotracheal tube as evaluated by X-ray.
The correlation between the height-based calculation and the ideal depth observed on X-ray was strong, with r = 0.88, p < 0.05, and a concordance correlation coefficient of 0.88; the correlation between the weight-based calculation and depth on X-ray was r = 0.75, p < 0.05, and concordance correlation coefficient 0.43; and the correlation between endotracheal tube diameter-based calculation and depth on X-ray was r = 0.80, p < 0.05, and concordance correlation coefficient 0.78. Lin’s concordance correlation analysis indicated that the measurements showed weak concordance (< 0.90).
The formulas that estimate the insertion depth of the endotracheal tube in children were not accurate and were discordant with the gold-standard method of X-ray evaluation. There is a need for a new method based on anthropometric variables (weight and height) and age that is effective in guiding health professionals of pediatric intensive care units at the time of intubation.
Abstract
Rev Bras Ter Intensiva. 2019;31(4):586-591
DOI 10.5935/0103-507X.20190068
Among the infections caused by Streptococcus β hemolyticus from the Lancefield serogroup A, toxic shock syndrome is perhaps the most severe, and its mortality rate is high. Its clinical similarity to other forms of shock, especially septic shock, can often confuse the evaluator and interfere with the selection of the most appropriate therapy. This report aims to inform readers of the need to add this syndrome as a differential diagnosis in cases of shock, especially those with no well-defined clinical manifestations. For this purpose, we present the case of an infant with common flu-like symptoms who progressed rapidly with a rash, a reduced level of consciousness and clinical and laboratory signs of shock that required intensive support. In addition to cultures indicating the etiological agent, the appearance of exanthema and necrotizing fasciitis led to the diagnosis. However, less than 50% of cases present classic clinical signs of this entity. Penicillins combined with aminoglycosides are still the therapy of choice and are supported by a high level of evidence. Despite the severity of this patient's presentation, the progression was satisfactory.

Abstract
Rev Bras Ter Intensiva. 2019;31(3):333-339
DOI 10.5935/0103-507X.20190045
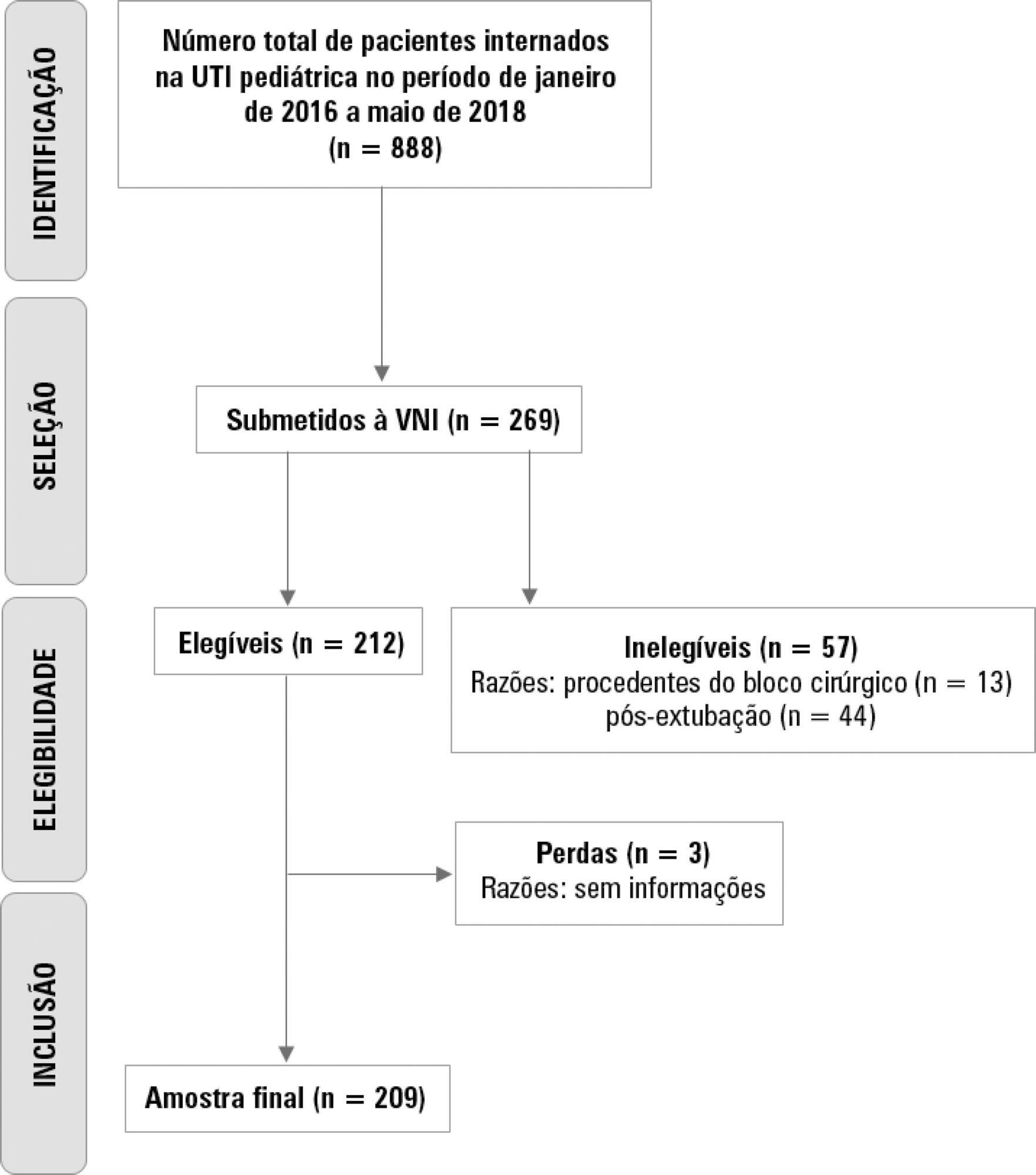
To describe the use of noninvasive ventilation to prevent tracheal intubation in children in a pediatric intensive care unit and to analyze the factors related to respiratory failure.
A retrospective cohort study was performed from January 2016 to May 2018. The study population included children aged 1 to 14 years who were subjected to noninvasive ventilation as the first therapeutic choice for acute respiratory failure. Biological, clinical and managerial data were analyzed by applying a model with the variables that obtained significance ≤ 0.20 in a bivariate analysis. Logistic regression was performed using the ENTER method. The level of significance was set at 5%.
The children had a mean age of 68.7 ± 42.3 months, 96.6% had respiratory disease as a primary diagnosis, and 15.8% had comorbidities. Of the 209 patients, noninvasive ventilation was the first option for ventilatory support in 86.6% of the patients, and the fraction of inspired oxygen was ≥ 0.40 in 47% of the cases. The lethality rate was 1.4%. The data for the use of noninvasive ventilation showed a high success rate of 95.3% (84.32 - 106). The Pediatric Risk of Mortality (PRISM) score and the length of stay in the intensive care unit were the significant clinical variables for the success or failure of noninvasive ventilation.
A high rate of effectiveness was found for the use of noninvasive ventilation for acute episodes of respiratory failure. A higher PRISM score on admission, comorbidities associated with respiratory symptoms and oxygen use ≥ 40% were independent factors related to noninvasive ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):248-257
DOI 10.5935/0103-507X.20190038
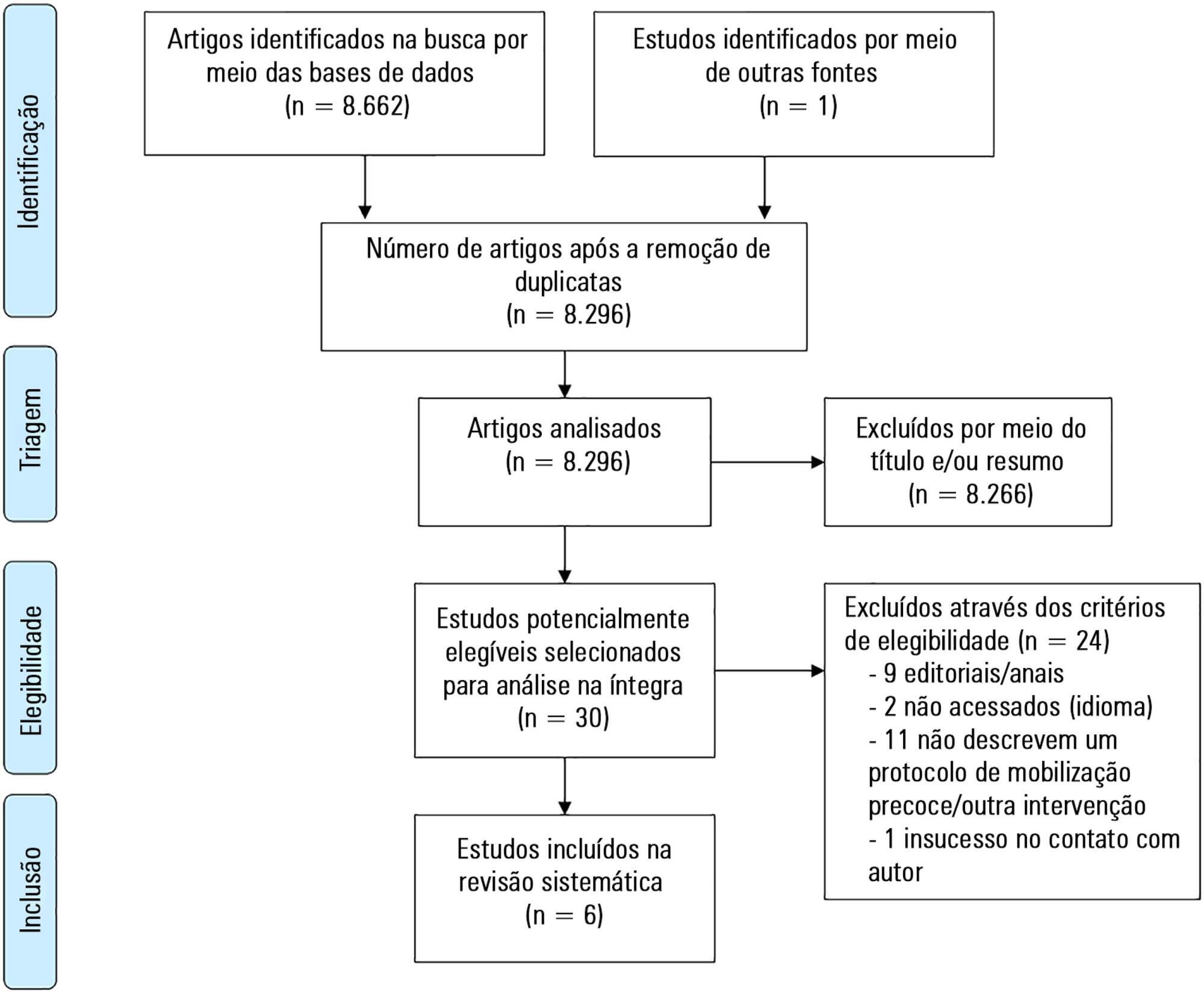
To describe the existing early mobilization protocols in pediatric intensive care units.
A systematic literature review was performed using the databases MEDLINE®, Embase, SciELO, LILACS and PeDRO, without restrictions of date and language. Observational and randomized and nonrandomized clinical trials that described an early mobilization program in patients aged between 29 days and 18 years admitted to the pediatric intensive care unit were included. The methodological quality of the studies was evaluated using the Newcastle-Ottawa Scale, Methodological Index for Non-Randomized Studies and the Cochrane Collaboration.
A total of 8,663 studies were identified, of which 6 were included in this review. Three studies described the implementation of an early mobilization program, including activities such as progressive passive mobilization, positioning, and discussion of mobilization goals with the team, in addition to contraindications and interruption criteria. Cycle ergometer and virtual reality games were also used as resources for mobilization. Four studies considered the importance of the participation of the multidisciplinary team in the implementation of early mobilization protocols.
In general, early mobilization protocols are based on individualized interventions, depending on the child's development. In addition, the use of a cycle ergometer may be feasible and safe in this population. The implementation of institutional and multidisciplinary protocols may contribute to the use of early mobilization in pediatric intensive care units; however, studies demonstrating the efficacy of such intervention are needed.
Abstract
Rev Bras Ter Intensiva. 2018;30(4):429-435
DOI 10.5935/0103-507X.20180065
To evaluate the association between acute kidney injury through the pediatric Risk, Injury, Failure, Loss and End Stage Renal Disease score and mortality in a pediatric intensive care unit.
This retrospective cohort study assessed all children admitted to the pediatric intensive care unit of a reference hospital in Brazil from January to December 2016. Patients were screened for the presence of acute kidney injury through the pediatric Risk, Injury, Failure, Loss and End Stage Renal Disease score. Patients were subdivided into the stages of Risk, Injury and Kidney Failure.
The sample comprised 192 children, of whom 45.8% developed acute kidney injury, with 79.5% of the cases identified up to 72 hours after admission. Patients with acute kidney injury showed a 3.74 increase risk of death (p = 0.01) than the control group. Patients with kidney failure had a mortality rate that was 8.56 times greater than that of the remaining sample (p < 0.001). The variables that were associated with the stages of acute kidney injury were nephrotoxic drugs (p = 0.025), renal replacement therapy (p < 0.001), vasoactive drugs (p < 0.001), pediatric risk of mortality 2 score (p = 0.023), fluid overload (p = 0.005), pediatric intensive care unit length of stay (p = 0.001) and death (p < 0.001).
In this study, the pediatric Risk, Injury, Failure, Loss and End Stage Renal Disease score proved to be a useful tool for the early identification of severely ill children with acute kidney injury, showing an association with mortality. We thus suggest its use for pediatric intensive care unit patient admission.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):333-337
DOI 10.5935/0103-507X.20180045
To analyze the characteristics and outcomes of children hospitalized for burns in a pediatric trauma intensive care unit for burn patients.
An observational study was conducted through the retrospective analysis of children (< 16 years) admitted to the pediatric trauma intensive care unit for burn victims between January 2013 and December 2015. Sociodemographic and clinical variables were analyzed including the causal agent, burned body surface, presence of inhalation injury, length of hospital stay and mortality.
The study analyzed a sum of 140 patients; 61.8% were male, with a median age of 24 months and an overall mortality of 5%. The main cause of burns was scalding (51.4%), followed by accidents involving fire (38.6%) and electric shock (6.4%). Mechanical ventilation was used in 20.7% of the cases. Associated inhalation injury presented a relative risk of 6.1 (3.5 - 10.7) of needing ventilatory support and a relative risk of mortality of 14.1 (2.9 - 68.3) compared to patients without this associated injury. A significant connection was found between burned body surface and mortality (p < 0.002), reaching 80% in patients with a burned area greater than 50%. Patients who died had a significantly higher Tobiasen Abbreviated Burn Severity Index than survivors (9.6 ± 2.2 versus 4.4 ± 1.1; p < 0.001). A Tobiasen Abbreviated Burn Severity Index ≥ 7 represented a relative risk of death of 68.4 (95%CI 9.1 - 513.5).
Scalding burns are quite frequent and are associated with high morbidity. Mortality is associated with the amount of burned body surface and the presence of inhalation injury. Special emphasis should be given to accidents involving fire, reinforcing proper diagnosis and treatment of inhalation injury.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)