You searched for:"Arnaldo Prata Barbosa"
We found (3) results for your search.-
Review Articles
Use of biomarkers in pediatric sepsis: literature review
Rev Bras Ter Intensiva. 2016;28(4):472-482
Abstract
Review ArticlesUse of biomarkers in pediatric sepsis: literature review
Rev Bras Ter Intensiva. 2016;28(4):472-482
DOI 10.5935/0103-507X.20160080
Views0See moreABSTRACT
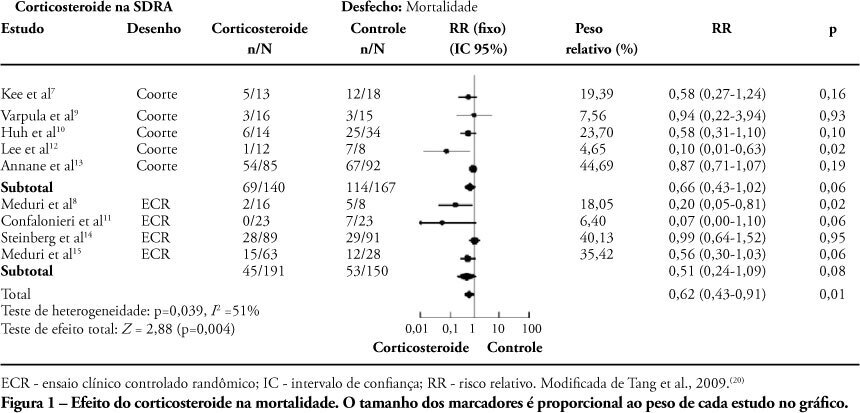
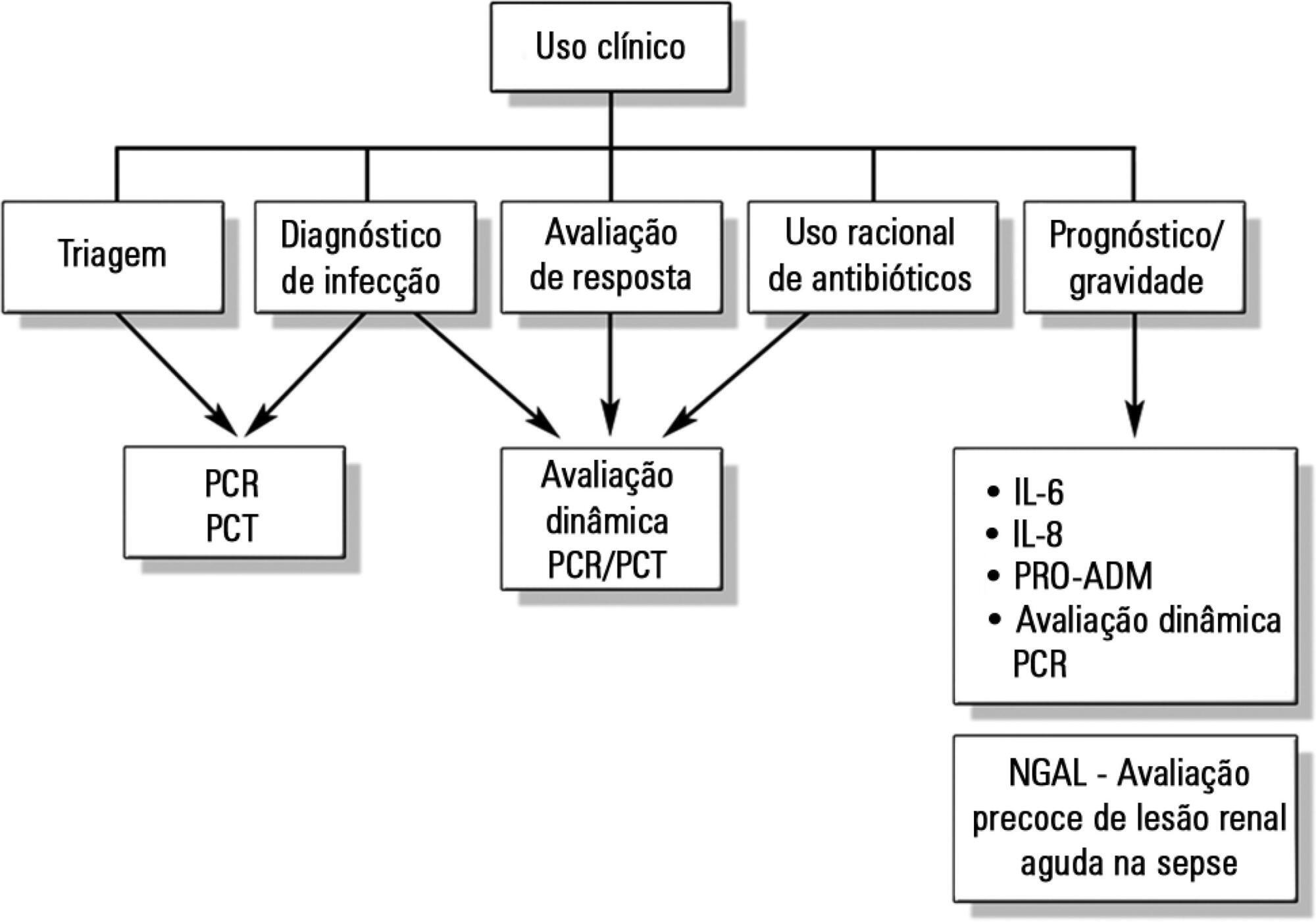
Despite advances in recent years, sepsis is still a leading cause of hospitalization and mortality in infants and children. The presence of biomarkers during the response to an infectious insult makes it possible to use such biomarkers in screening, diagnosis, prognosis (risk stratification), monitoring of therapeutic response, and rational use of antibiotics (for example, the determination of adequate treatment length). Studies of biomarkers in sepsis in children are still relatively scarce. This review addresses the use of biomarkers in sepsis in pediatric patients with emphasis on C-reactive protein, procalcitonin, interleukins 6, 8, and 18, human neutrophil gelatinase, and proadrenomedullin. Assessment of these biomarkers may be useful in the management of pediatric sepsis.
-
Original Articles – Clinical Research
Professional profile of pediatric intensivists in Rio de Janeiro, southeastern Brazil
Rev Bras Ter Intensiva. 2011;23(4):462-469
Abstract
Original Articles – Clinical ResearchProfessional profile of pediatric intensivists in Rio de Janeiro, southeastern Brazil
Rev Bras Ter Intensiva. 2011;23(4):462-469
DOI 10.1590/S0103-507X2011000400011
Views0OBJECTIVE: This study described the sociodemographic profile and professional qualifications of pediatric intensive care physicians in the State of Rio de Janeiro (RJ), southeastern Brazil. METHODS: This investigation was an observational, cross-sectional and descriptive study that was conducted in neonatal, pediatric and mixed intensive care units in the State of Rio de Janeiro. Physicians working in the participating intensive care units voluntarily completed a semistructured and anonymous questionnaire. Questionnaires that were not returned within 30 days were considered lost, and questionnaires with less than 75% questions completed were excluded. The differences in neonatal and pediatric intensive care physicians’ medical training were compared using the Chi-squared test with a 5% significance level. RESULTS: A total of 410 physicians were included in this study: 84% female, 48% between 30 and 39 years old and 45% with monthly incomes between US $1,700 to 2,700. Forty percent of these physicians worked exclusively in this specialty, and 72% worked in more than one intensive care unit. Only 50% of the participants had received specific training (either medical residency or specialization) in neonatology, and only 33% were board-certified specialists in this area. Only 27% of the physicians had received specific training in pediatric intensive care medicine, and only 17% were board-certified specialists (p < 0.0005 for both comparisons). Most (87%) physicians had participated in scientific events within the past 5 years, and 55% used the internet for continued medical education. However, only 25% had participated in any research. Most (63%) physicians were dissatisfied with their professional activity; 49% were dissatisfied due to working conditions, 23% due to low incomes and 18% due to training-related issues. CONCLUSION: These results suggested that the medical qualifications of neonatal and pediatric intensive care physicians in the State of Rio de Janeiro, Brazil are inadequate, especially in pediatric intensive care medicine. A high level of dissatisfaction was reported, which may jeopardize the quality of medical assistance that is provided by these professionals.
Keywords:BrazilEducation, medicalIntensive careIntensive care units, neonatalIntensive care units, pediatricProfessional practiceSee more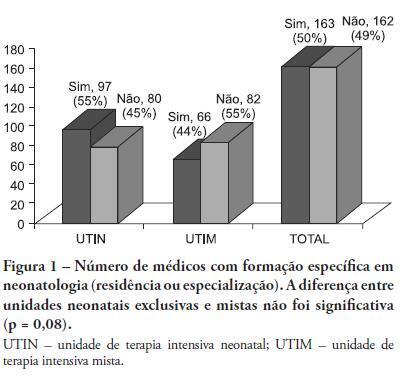
Search
Search in:
KEY WORDS
Case reports Child Coronavirus infections COVID-19 Critical care Critical illness Extracorporeal membrane oxygenation Infant, newborn Intensive care Intensive care units Intensive care units, pediatric mechanical ventilation Mortality Physical therapy modalities Prognosis Respiration, artificial Respiratory insufficiency risk factors SARS-CoV-2 Sepsis