Abstract
Revista brasileira de terapia intensiva. 2013;25(4):306-311
DOI 10.5935/0103-507X.20130052
Compare the scores resulting from the Comfort-B scale with the bispectral index in children in an intensive care unit.
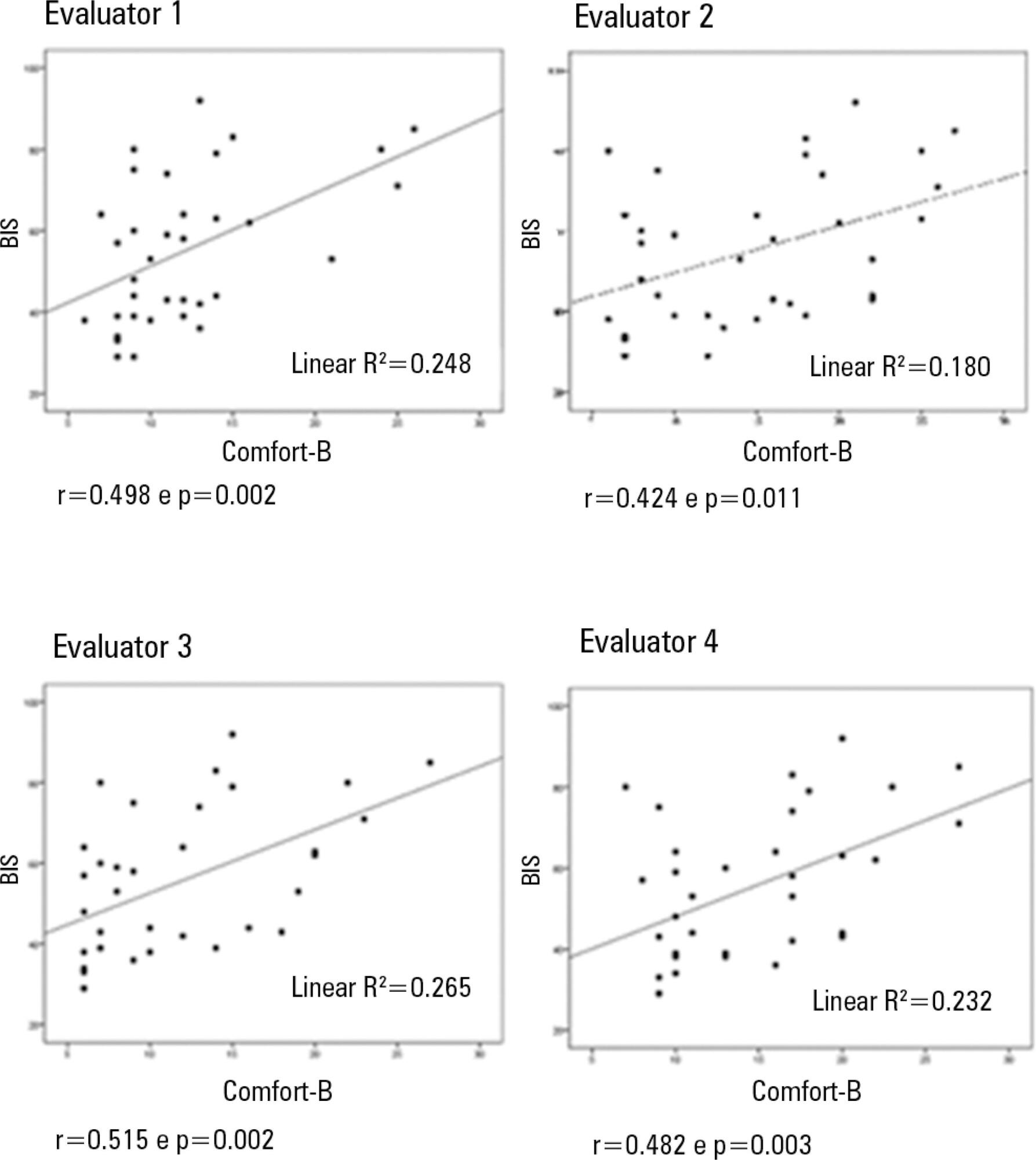
Eleven children between the ages of 1 month and 16 years requiring mechanical ventilation and sedation were simultaneously classified based on the bispectral index and the Comfort-B scale. Their behavior was recorded using digital photography, and the record was later evaluated by three independent evaluators. Agreement tests (Bland-Altman and Kappa) were then performed. The correlation between the two methods (Pearson correlation) was tested.
In total, 35 observations were performed on 11 patients. Based on the Kappa coefficient, the agreement among evaluators ranged from 0.56 to 0.75 (p<0.001). There was a positive and consistent association between the bispectral index and the Comfort-B scale [r=0.424 (p=0.011) to r=0.498 (p=0.002)].
Due to the strong correlation between the independent evaluators and the consistent correlation between the two methods, the results suggest that the Comfort-B scale is reproducible and useful in classifying the level of sedation in children requiring mechanical ventilation.
Abstract
Revista Brasileira de Terapia Intensiva. 2011;23(4):462-469
DOI 10.1590/S0103-507X2011000400011
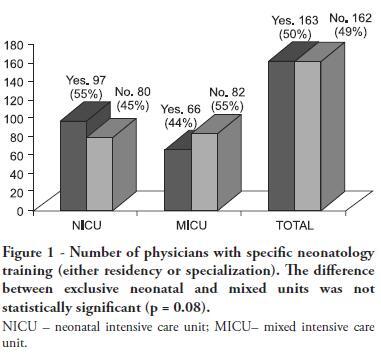
OBJECTIVE: This study described the sociodemographic profile and professional qualifications of pediatric intensive care physicians in the State of Rio de Janeiro (RJ), southeastern Brazil. METHODS: This investigation was an observational, cross-sectional and descriptive study that was conducted in neonatal, pediatric and mixed intensive care units in the State of Rio de Janeiro. Physicians working in the participating intensive care units voluntarily completed a semistructured and anonymous questionnaire. Questionnaires that were not returned within 30 days were considered lost, and questionnaires with less than 75% questions completed were excluded. The differences in neonatal and pediatric intensive care physicians' medical training were compared using the Chi-squared test with a 5% significance level. RESULTS: A total of 410 physicians were included in this study: 84% female, 48% between 30 and 39 years old and 45% with monthly incomes between US $1,700 to 2,700. Forty percent of these physicians worked exclusively in this specialty, and 72% worked in more than one intensive care unit. Only 50% of the participants had received specific training (either medical residency or specialization) in neonatology, and only 33% were board-certified specialists in this area. Only 27% of the physicians had received specific training in pediatric intensive care medicine, and only 17% were board-certified specialists (p < 0.0005 for both comparisons). Most (87%) physicians had participated in scientific events within the past 5 years, and 55% used the internet for continued medical education. However, only 25% had participated in any research. Most (63%) physicians were dissatisfied with their professional activity; 49% were dissatisfied due to working conditions, 23% due to low incomes and 18% due to training-related issues. CONCLUSION: These results suggested that the medical qualifications of neonatal and pediatric intensive care physicians in the State of Rio de Janeiro, Brazil are inadequate, especially in pediatric intensive care medicine. A high level of dissatisfaction was reported, which may jeopardize the quality of medical assistance that is provided by these professionals.
Abstract
Revista Brasileira de Terapia Intensiva. 2009;21(3):299-305
DOI 10.1590/S0103-507X2009000300010
OBJECTIVE: To investigate the relationship between work and quality of life of doctors and nurses in pediatric intensive care units and neonatal. METHODS: Cross-sectional study with 37 doctors and 20 nurses. The Job Content Questionnarie (JCQ) e Effort-Reward Imbalance (ERI), and World Health Organization Quality of Life (WHOQOL-100) were used. The correlation was estimated by Spearman correlation coefficient. RESULTS: The effort is inversely correlated with the areas physical, psychological, level of independence, environment (p<0.01) and social relationship (p<0.05). The reward is inversely correlated with the areas and psychological (p<0.05) level of independence (p<0.01). Control over the work is directly correlated with the physical domain (p<0.05). The psychological demands are inversely correlated with the areas physical (p<0.05), psychological (p<0.01) and level of independence (p<0.01). The physical demand is inversely correlated with physical areas, level of independence, environmental (p<0.01) and psychological (p<0.05). Job insecurity is inversely correlated with the psychological fields, level of independence (p<0.05) and the environment (p<0.01). Support the supervisor is directly correlated with degree of independence (p <0.05). CONCLUSION: Doctors and nurses showed high efforts, demands psychological, physical and job insecurity that impact on quality of life.
Abstract
Revista Brasileira de Terapia Intensiva. 2008;20(4):325-330
DOI 10.1590/S0103-507X2008000400002
OBJECTIVES: Sedation scores are important tools for use in pediatric intensive care units. The Comfort-Behavior scale is a valid method for the assessment of children although it is considered an extensive scale. The motor activity assessment scale is validated for an adult population. We considered it simpler then the one above and suitable for application in children. None of these scores had been translated into Portuguese. Our objective was to apply both scales in Portuguese to a pediatric population under mechanical ventilation. Secondary objectives were to evaluate the sedation level of children on mechanical ventilation in tertiary pediatric intensive care units and to compare the Comfort- Behavior and motor activity assessment scales in this population. METHODS: After translating the scales into Portuguese, both were simultaneously applied to 26 patients by 2 pediatricians. Each scale was applied 116 times in total. RESULTS: The intraclass correlation coefficient was 0.90 (0.85 - 0.93 CI 95%) for the Comfort-Behavior and 0.94 (0.92 - 0.96 CI 95%) for the motor activity assessment scale. When applying the Comfort-Behavior scale, the Crombach's alpha was 0.81 for observer A and 0.92 for observer B. The Spearman coefficient was 0.86 for observer A and 0.91 for observer B. These patients were found to be deeply sedated, showing low values in both scales. CONCLUSIONS: The scales were successfully translated into Portuguese and both were adequate to assess pain and sedation in the pediatric population under mechanical ventilation. Sedation level was high in this sample of applications.