Abstract
Rev Bras Ter Intensiva. 2021;33(4):549-556
DOI 10.5935/0103-507X.20210083
To analyze the correlation between glycocalyx disruption measured via the serum syndecan-1 level and organ dysfunctions assessed by the PELOD-2 score and to evaluate its association with mortality in pediatric sepsis.
We performed a prospective observational study in a tertiary public hospital. Sixty-eight pediatric patients diagnosed with sepsis according to International Pediatric Sepsis Consensus Conference criteria were consecutively recruited. We performed measurements of day 1 and day 5 serum syndecan-1 levels and PELOD-2 score components. Patients were followed up to 28 days following sepsis diagnosis.
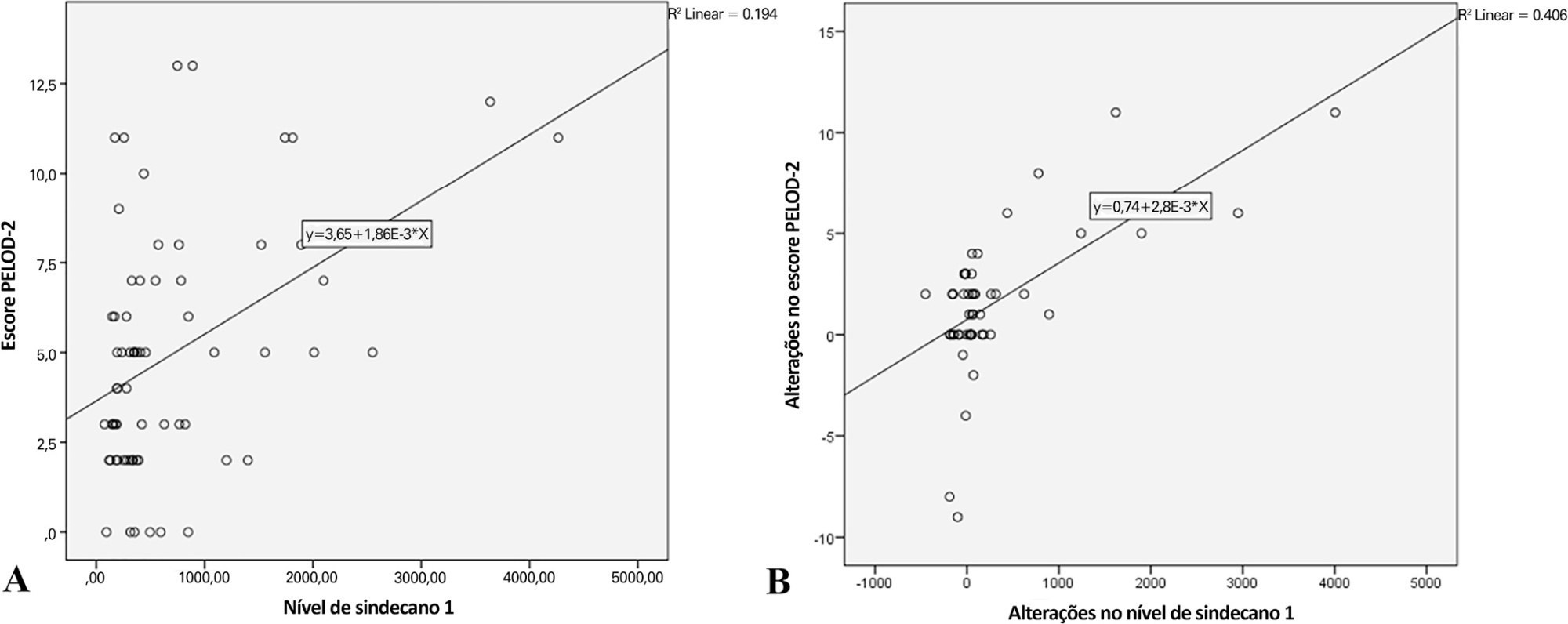
Overall, the syndecan-1 level was increased in all subjects, with a significantly higher level among septic shock patients (p = 0.01). The day 1 syndecan-1 level was positively correlated with the day 1 PELOD-2 score with a correlation coefficient of 0.35 (p = 0.003). Changes in syndecan-1 were positively correlated with changes in the PELOD-2 score, with a correlation coefficient of 0.499 (p < 0.001) during the first five days. Using the cutoff point of day 1 syndecan-1 ≥ 430ng/mL, organ dysfunction (PELOD-2 score of ≥ 8) could be predicted with an AUC of 74.3%, sensitivity of 78.6%, and specificity of 68.5% (p = 0.001).
The day 1 syndecan-1 level was correlated with the day 1 PELOD-2 score but not 28-day mortality. Organ dysfunction (PELOD-2 ≥ 8) could be predicted by the syndecan-1 level in the first 24 hours of sepsis, suggesting its significant pathophysiological involvement in sepsis-associated organ dysfunction.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):592-599
DOI 10.5935/0103-507X.20210086
To translate and culturally adapt the Pediatric Intensive Care Unit-Quality of Dying and Death questionnaire into Brazilian Portuguese.
This was a cross-cultural adaptation process including conceptual, cultural, and semantic equivalence steps comprising three stages. Stage 1 involved authorization to perform the translation and cultural adaptation. Stage 2 entailed independent translation from English into Brazilian Portuguese, a synthesis of the translation, back-translation, and an expert panel. Stage 3 involved a pretest conducted with family caregivers and a multidisciplinary team.
The evaluation by the expert panel resulted in an average agreement of 0.8 in relation to semantic, cultural, and conceptual equivalence. The pretests of both versions of the questionnaire showed that the participants had adequate comprehension regarding the ease of understanding the items and response options.
After going through the process of translation and cultural adaptation, the Pediatric Intensive Care Unit-Quality of Dying and Death caregiver and multidisciplinary team versions were considered culturally adapted, with both groups having a good understanding of the items. The questionnaires include relevant items to evaluate the process of death and dying in the intensive care setting, and suggest changes in care centered on patients and especially family caregivers, given the finitude of their children.
Abstract
Rev Bras Ter Intensiva. 2021;33(4):616-623
DOI 10.5935/0103-507X.20210071
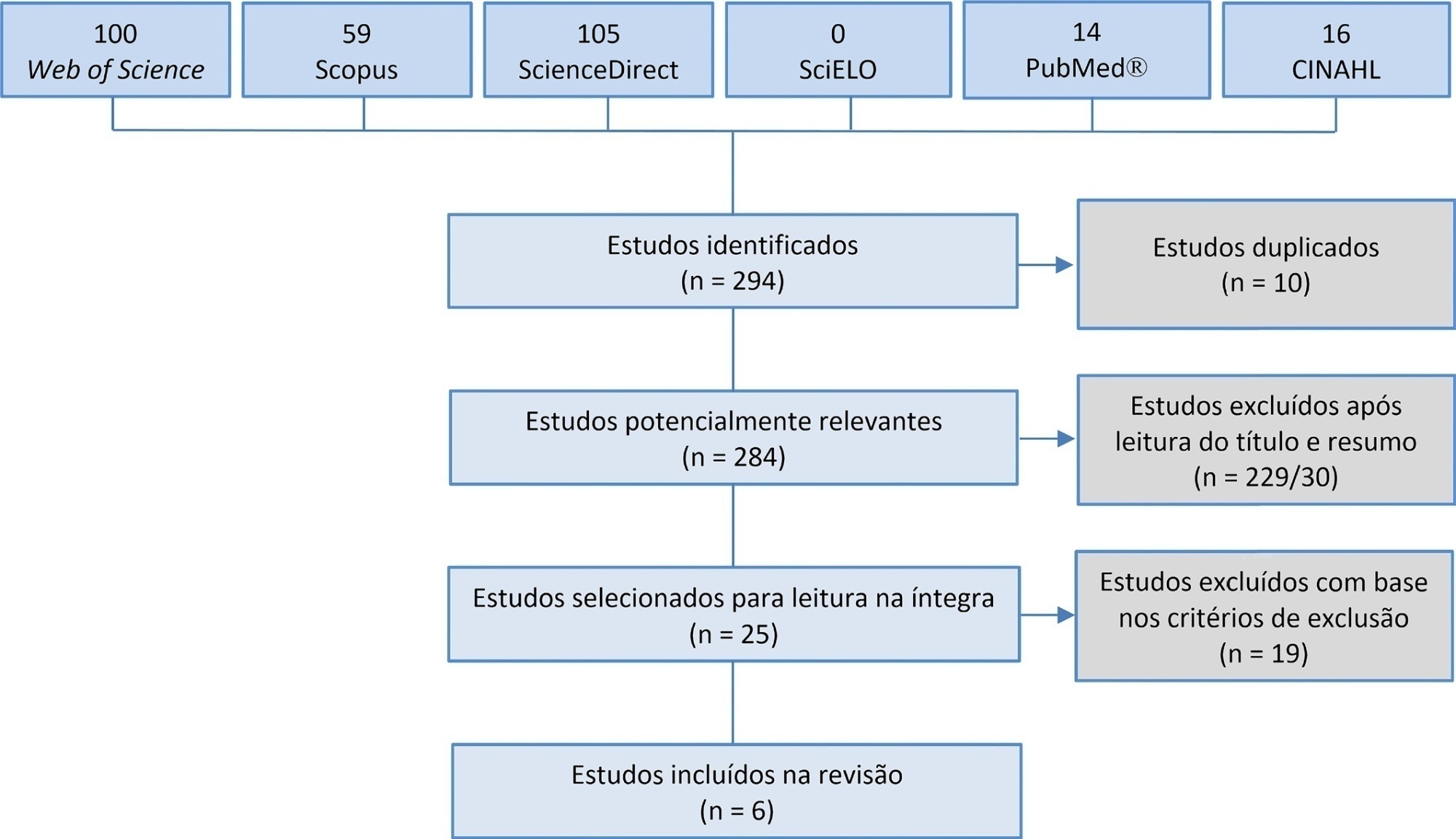
Manual hyperinflation is used in neonatal and pediatric intensive care units to promote expiratory flow bias, but there is no consensus on the benefits of the technique. Thus, a review that presents supporting evidence is necessary. This study aims to review the literature on the manual hyperinflation maneuver in neonatal and pediatric intensive care units to analyze the evidence for this technique in terms of the forms of application (associated with other techniques or not), its safety, the performance of manual resuscitators and the influence of the physical therapist’s experience, in addition to evaluating the methodological quality of the identified articles. A search was performed in the following databases: Web of Science, ScienceDirect, PubMedⓇ, Scopus, CINAHL and SciELO. Two researchers independently selected the articles. Duplicate studies were assessed, evaluated by title and abstract and then read in full. The quality of the articles was analyzed using the PEDro scale. Six articles were included, two of which had high methodological quality. The main results provided information on the contribution of the positive end-expiratory pressure valve to increasing lung volumes and the use of chest compressions to optimize expiratory flow bias, the negative influence of operator experience on the increase in peak inspiratory flow, the performance of different manual resuscitators when used with the technique and the safety of application in terms of maintaining hemodynamic stability and increasing peripheral oxygen saturation. The available studies point to a positive effect of the manual hyperinflation maneuver in children who are admitted to intensive care units.
Registration PROSPERO: CRD42018108056.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):231-242
DOI 10.5935/0103-507X.20210030
To report the prevalence and outcomes of sepsis in children admitted to public and private hospitals.
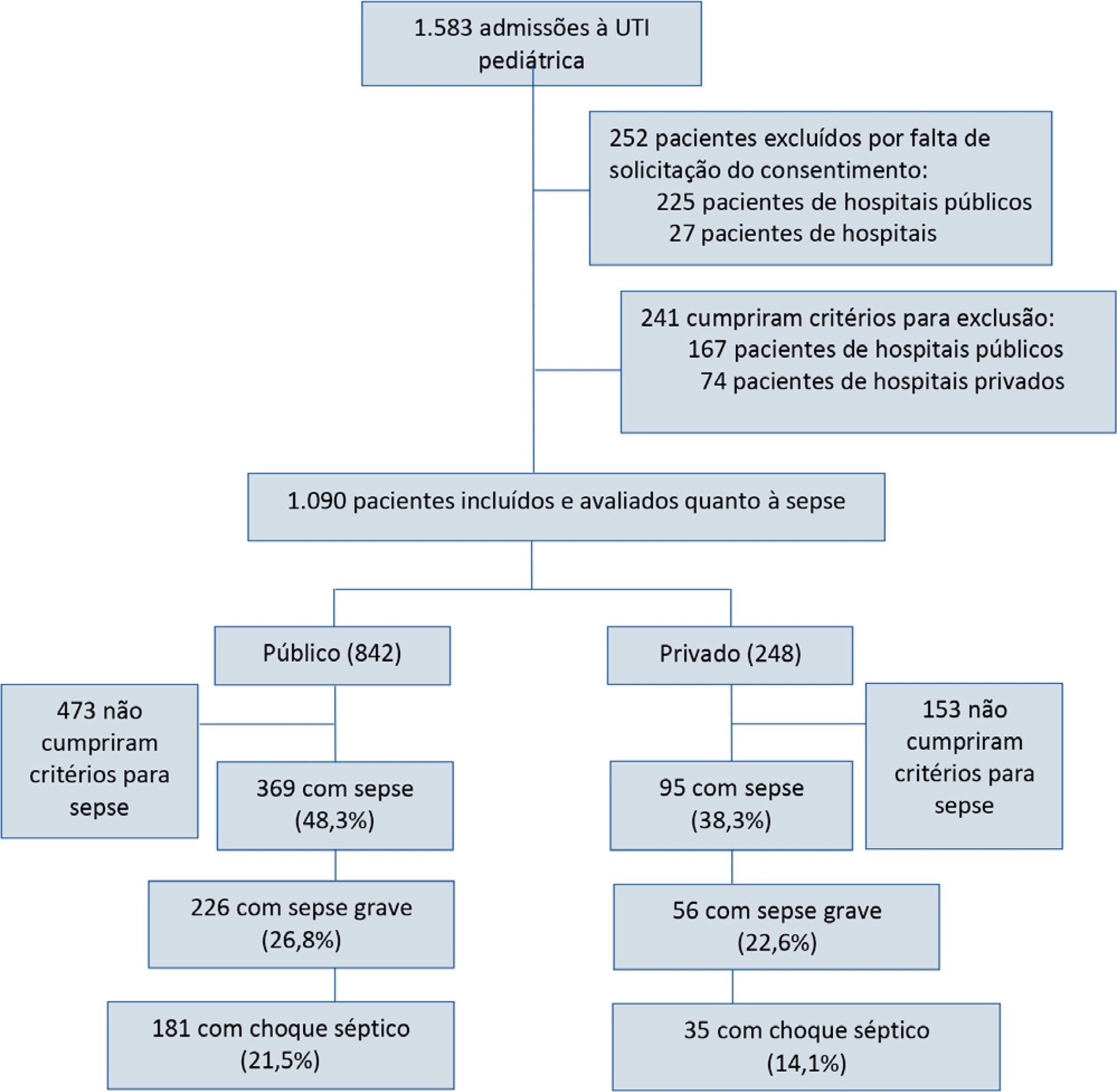
Post hoc analysis of the Latin American Pediatric Sepsis Study (LAPSES) data, a cohort study that analyzed the prevalence and outcomes of sepsis in critically ill children with sepsis on admission at 21 pediatric intensive care units in five Latin American countries.
Of the 464 sepsis patients, 369 (79.5%) were admitted to public hospitals and 95 (20.5%) to private hospitals. Compared to those admitted to private hospitals, sepsis patients admitted to public hospitals did not differ in age, sex, immunization status, hospital length of stay or type of admission but had higher rates of septic shock, higher Pediatric Risk of Mortality (PRISM), Pediatric Index of Mortality 2 (PIM 2), and Pediatric Logistic Organ Dysfunction (PELOD) scores, and higher rates of underlying diseases and maternal illiteracy. The proportion of patients admitted from pediatric wards and sepsis-related mortality were higher in public hospitals. Multivariate analysis did not show any correlation between mortality and the type of hospital, but mortality was associated with greater severity on pediatric intensive care unit admission in patients from public hospitals.
In this sample of critically ill children from five countries in Latin America, the prevalence of septic shock within the first 24 hours at admission and sepsis-related mortality were higher in public hospitals than in private hospitals. Higher sepsis-related mortality in children admitted to public pediatric intensive care units was associated with greater severity on pediatric intensive care unit admission but not with the type of hospital. New studies will be necessary to elucidate the causes of the higher prevalence and mortality of pediatric sepsis in public hospitals.
Abstract
Rev Bras Ter Intensiva. 2021;33(2):304-311
DOI 10.5935/0103-507X.20210039
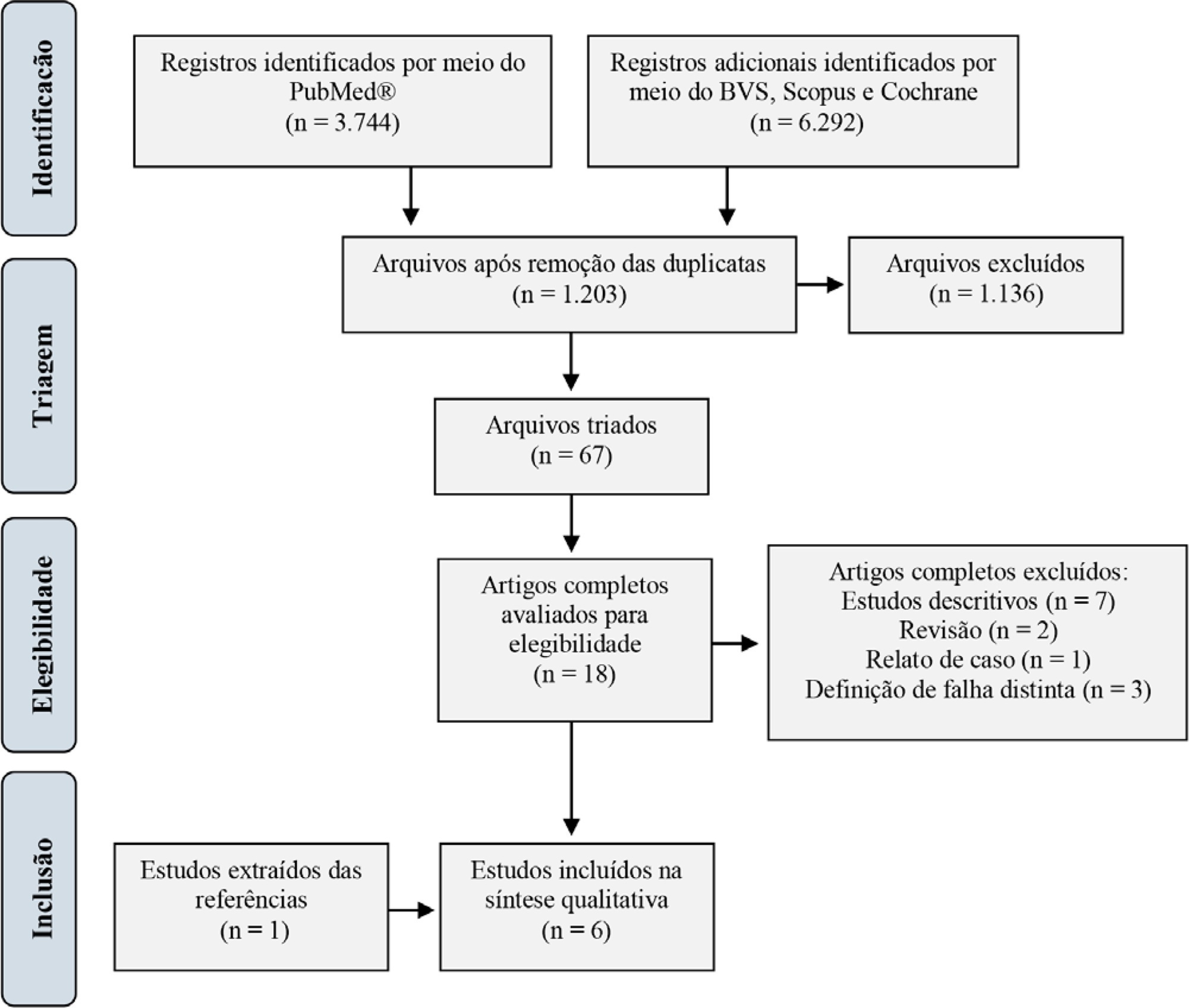
For extubation in pediatric patients, the evaluation of readiness is strongly recommended. However, a device or practice that is superior to clinical judgment has not yet been accurately determined. Thus, it is important to conduct a review on the techniques of choice in clinical practice to predict extubation failure in pediatric patients. Based on a search in the PubMed®, Biblioteca Virtual em Saúde, Cochrane Library and Scopus databases, we conducted a survey of the predictive variables of extubation failure most commonly used in clinical practice in pediatric patients. Of the eight predictors described, the three most commonly used were the spontaneous breathing test, the rapid shallow breathing index and maximum inspiratory pressure. Although the disparity of the data presented in the studies prevented statistical treatment, it was still possible to describe and analyze the performance of these tests.
Abstract
Rev Bras Ter Intensiva. 2020;32(4):551-556
DOI 10.5935/0103-507X.20200092
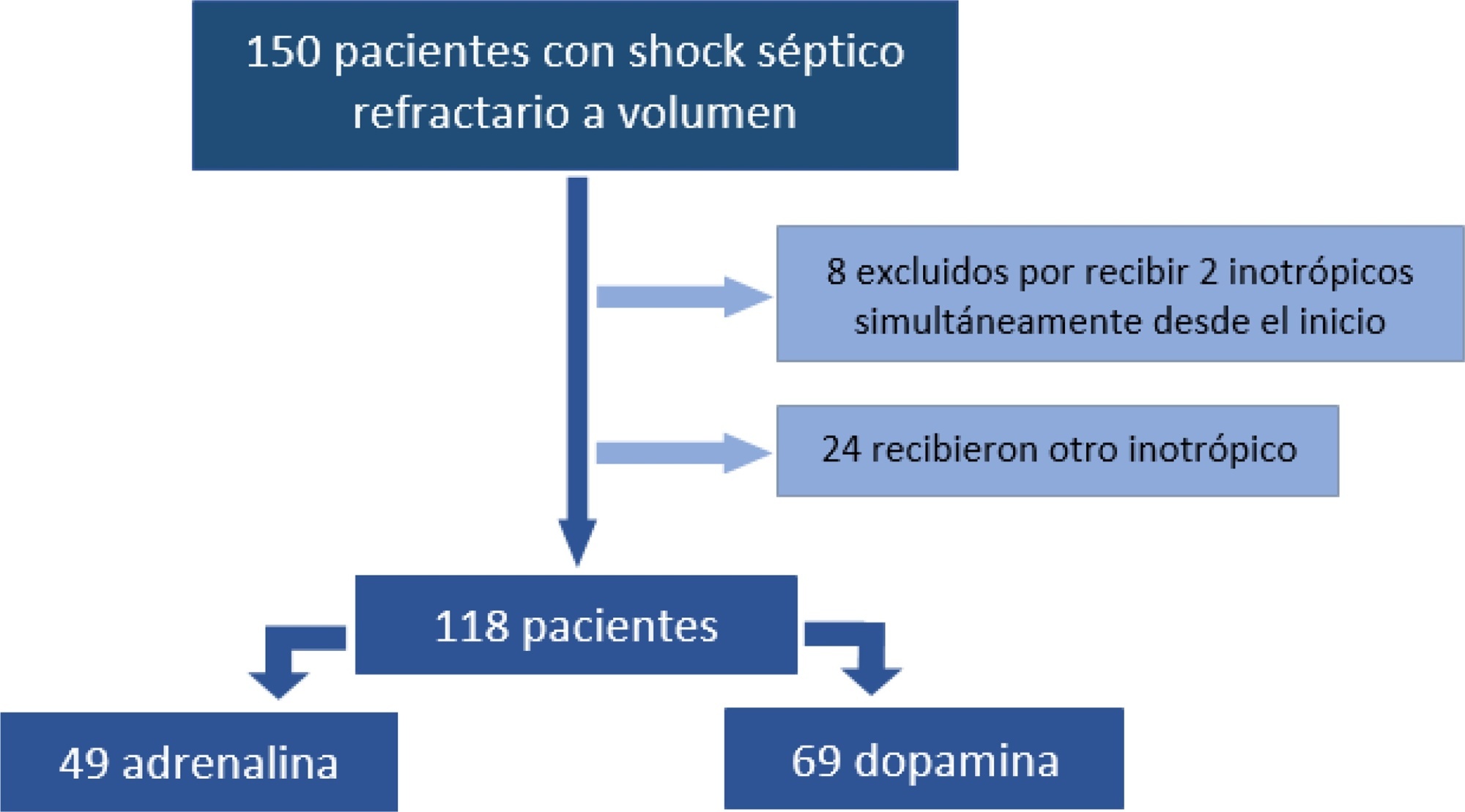
To analyze the clinical outcome of children with fluid-refractory septic shock initially treated with dopamine or epinephrine.
A retrospective cohort study was conducted at a pediatric emergency department of a tertiary hospital. Population: children admitted because of fluid-refractory septic shock. Clinical outcome was compared between two groups: Dopamine and Epinephrine. Variables evaluated were use of invasive mechanical ventilation, days of inotropic therapy, length of hospital stay, intensive care stay, and mortality. For numerical and categorical variables, we used measures of central tendency. They were compared by the Mann-Whitney U-test and the (2 test.
We included 118 patients. A total of 58.5% received dopamine and 41.5% received epinephrine. The rate of invasive mechanical ventilation was 38.8% for epinephrine versus 40.6% for dopamine (p = 0.84), with a median of 4 days for the Epinephrine Group and 5.5 for the Dopamine Group (p = 0.104). Median time of inotropic therapy was 2 days for both groups (p = 0.714). Median hospital stay was 11 and 13 days for the Epinephrine and Dopamine groups, respectively (p = 0.554), and median stay in intensive care was 4 days (0 - 81 days) in both groups (p = 0.748). Mortality was 5% for the Epinephrine Group versus 9% for the Dopamine Group (p = 0.64).
At our center, no differences in use of invasive mechanical ventilation, time of inotropic therapy, length of hospital stay, length of intensive care unit stay, or mortality were observed in children admitted to the pediatric emergency department with a diagnosis of fluid-refractory septic shock initially treated with dopamine versus epinephrine.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):391-397
DOI 10.5935/0103-507X.20200067
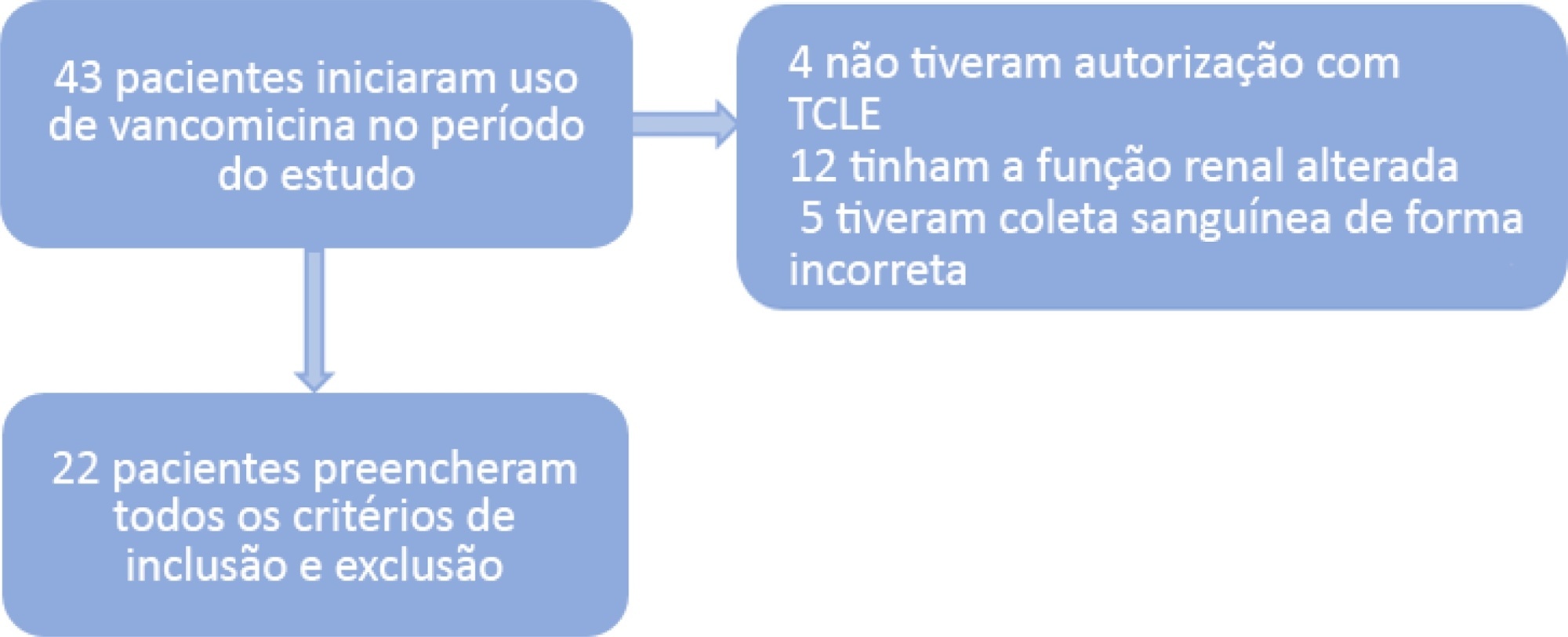
To investigate the vancomycin effectiveness against gram-positive pathogens with the minimum inhibitory concentration of 1mg/L in pediatric patients based on the area under the curve and the minimum inhibitory concentration ratio > 400.
A population of 22 pediatric patients (13 boys) admitted to the pediatric intensive care unit with preserved renal function was stratified in two groups (G1 < 7 years and G2 ≥ 7 years). After the fourth dose administered of vancomycin (10 - 15mg/kg every 6 hours) was administered, two blood samples were collected (third and fifth hours), followed by serum measurement by immunoassays to investigate the pharmacokinetics and antimicrobial coverage.
There was no difference between the groups regarding dose, trough level or area under the curve. Coverage against gram-positive pathogens with a minimum inhibitory concentration of 1mg/L occurred in only 46% of patients in both groups. The pharmacokinetics in both groups were altered relative to the reference values, and the groups differed in regard to increased total body clearance and shortening of the biological half-life, which were more pronounced in younger patients.
A minimum empirical dose of 60mg/kg per day should be prescribed for pediatric patients in intensive care units with preserved renal function. The use of the ratio between the area under the curve and minimum inhibitory concentration in the evaluation of vancomycin coverage is recommended to achieve the desired outcome, since the pharmacokinetics are altered in these patients, which may impact the effectiveness of the antimicrobial.
Search
Search in:
Case reports (56) Child (53) Coronavirus infections (34) COVID-19 (46) Critical care (116) Critical illness (54) Extracorporeal membrane oxygenation (26) Infant, newborn (27) Intensive care (72) Intensive care units (256) Intensive care units, pediatric (31) mechanical ventilation (38) Mortality (76) Physical therapy modalities (28) Prognosis (61) Respiration, artificial (119) Respiratory insufficiency (26) risk factors (34) SARS-CoV-2 (28) Sepsis (98)