Abstract
Rev Bras Ter Intensiva. 2020;32(4):551-556
DOI 10.5935/0103-507X.20200092
To analyze the clinical outcome of children with fluid-refractory septic shock initially treated with dopamine or epinephrine.
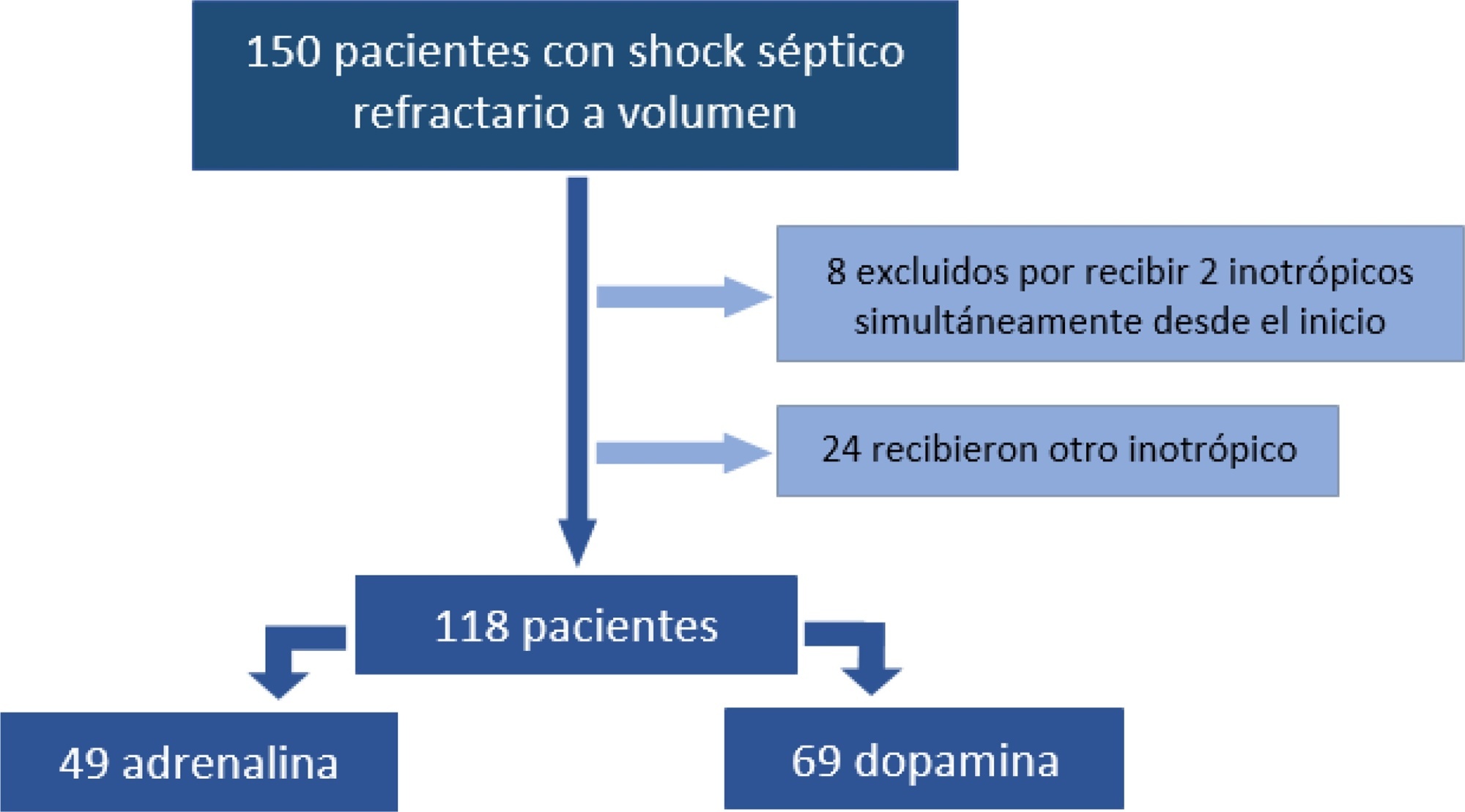
A retrospective cohort study was conducted at a pediatric emergency department of a tertiary hospital. Population: children admitted because of fluid-refractory septic shock. Clinical outcome was compared between two groups: Dopamine and Epinephrine. Variables evaluated were use of invasive mechanical ventilation, days of inotropic therapy, length of hospital stay, intensive care stay, and mortality. For numerical and categorical variables, we used measures of central tendency. They were compared by the Mann-Whitney U-test and the (2 test.
We included 118 patients. A total of 58.5% received dopamine and 41.5% received epinephrine. The rate of invasive mechanical ventilation was 38.8% for epinephrine versus 40.6% for dopamine (p = 0.84), with a median of 4 days for the Epinephrine Group and 5.5 for the Dopamine Group (p = 0.104). Median time of inotropic therapy was 2 days for both groups (p = 0.714). Median hospital stay was 11 and 13 days for the Epinephrine and Dopamine groups, respectively (p = 0.554), and median stay in intensive care was 4 days (0 - 81 days) in both groups (p = 0.748). Mortality was 5% for the Epinephrine Group versus 9% for the Dopamine Group (p = 0.64).
At our center, no differences in use of invasive mechanical ventilation, time of inotropic therapy, length of hospital stay, length of intensive care unit stay, or mortality were observed in children admitted to the pediatric emergency department with a diagnosis of fluid-refractory septic shock initially treated with dopamine versus epinephrine.
Abstract
Rev Bras Ter Intensiva. 2020;32(3):391-397
DOI 10.5935/0103-507X.20200067
To investigate the vancomycin effectiveness against gram-positive pathogens with the minimum inhibitory concentration of 1mg/L in pediatric patients based on the area under the curve and the minimum inhibitory concentration ratio > 400.
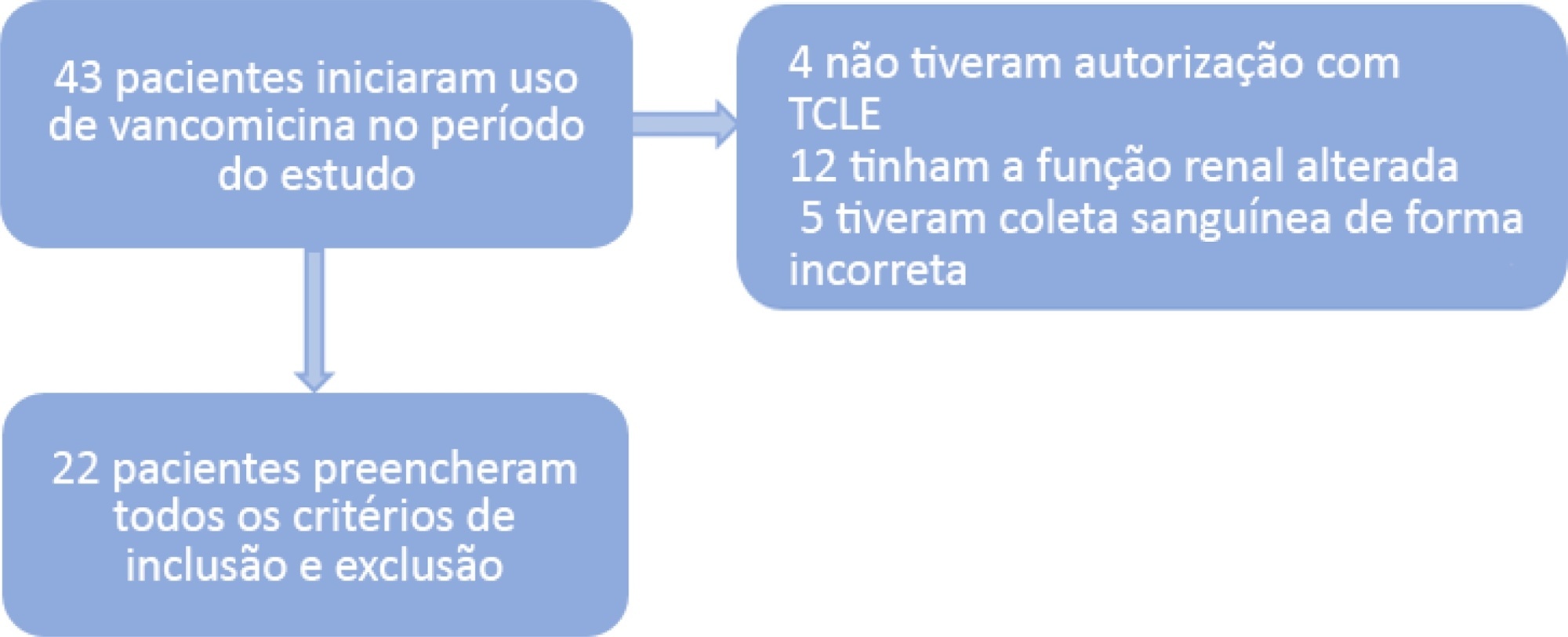
A population of 22 pediatric patients (13 boys) admitted to the pediatric intensive care unit with preserved renal function was stratified in two groups (G1 < 7 years and G2 ≥ 7 years). After the fourth dose administered of vancomycin (10 - 15mg/kg every 6 hours) was administered, two blood samples were collected (third and fifth hours), followed by serum measurement by immunoassays to investigate the pharmacokinetics and antimicrobial coverage.
There was no difference between the groups regarding dose, trough level or area under the curve. Coverage against gram-positive pathogens with a minimum inhibitory concentration of 1mg/L occurred in only 46% of patients in both groups. The pharmacokinetics in both groups were altered relative to the reference values, and the groups differed in regard to increased total body clearance and shortening of the biological half-life, which were more pronounced in younger patients.
A minimum empirical dose of 60mg/kg per day should be prescribed for pediatric patients in intensive care units with preserved renal function. The use of the ratio between the area under the curve and minimum inhibitory concentration in the evaluation of vancomycin coverage is recommended to achieve the desired outcome, since the pharmacokinetics are altered in these patients, which may impact the effectiveness of the antimicrobial.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):295-300
DOI 10.5935/0103-507X.20200046
To evaluate the effectiveness of the different formulas for estimating the insertion depth of an endotracheal tube in children.
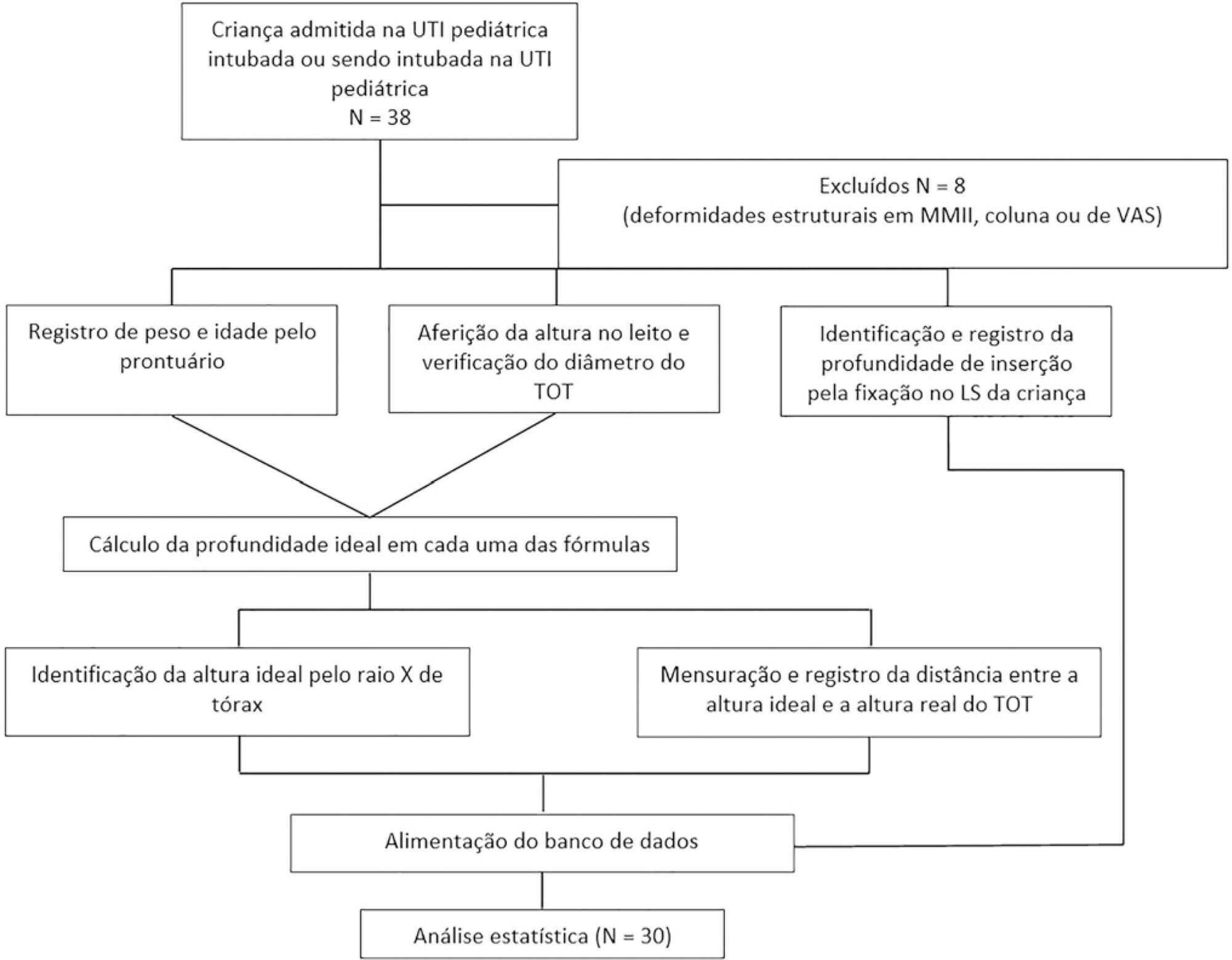
This was an observational and cross-sectional study that included children between 29 days and 2 years of age who were hospitalized in a pediatric intensive care unit and mechanically ventilated. The formulas based on height [(height/10) + 5], the inner diameter of the tube (endotracheal tube × 3), and weight (weight + 6) were evaluated to determine which of them showed better concordance with the ideal insertion depth of the endotracheal tube as evaluated by X-ray.
The correlation between the height-based calculation and the ideal depth observed on X-ray was strong, with r = 0.88, p < 0.05, and a concordance correlation coefficient of 0.88; the correlation between the weight-based calculation and depth on X-ray was r = 0.75, p < 0.05, and concordance correlation coefficient 0.43; and the correlation between endotracheal tube diameter-based calculation and depth on X-ray was r = 0.80, p < 0.05, and concordance correlation coefficient 0.78. Lin’s concordance correlation analysis indicated that the measurements showed weak concordance (< 0.90).
The formulas that estimate the insertion depth of the endotracheal tube in children were not accurate and were discordant with the gold-standard method of X-ray evaluation. There is a need for a new method based on anthropometric variables (weight and height) and age that is effective in guiding health professionals of pediatric intensive care units at the time of intubation.
Abstract
Rev Bras Ter Intensiva. 2020;32(2):261-267
DOI 10.5935/0103-507X.20200042
To evaluate the functional status of pediatric patients undergoing congenital heart surgery after discharge from the intensive care unit, and to evaluate the correlations among clinical variables, functional status and surgical risk.
Cross-sectional study including patients aged 1 month to less than 18 years undergoing congenital heart surgery between October 2017 and May 2018. Functional outcome was assessed by the Functional Status Scale, surgical risk classification was determined using the Risk Adjustment for Congenital Heart Surgery-1 (RACHS-1), and clinical variables were collected from electronic medical records.
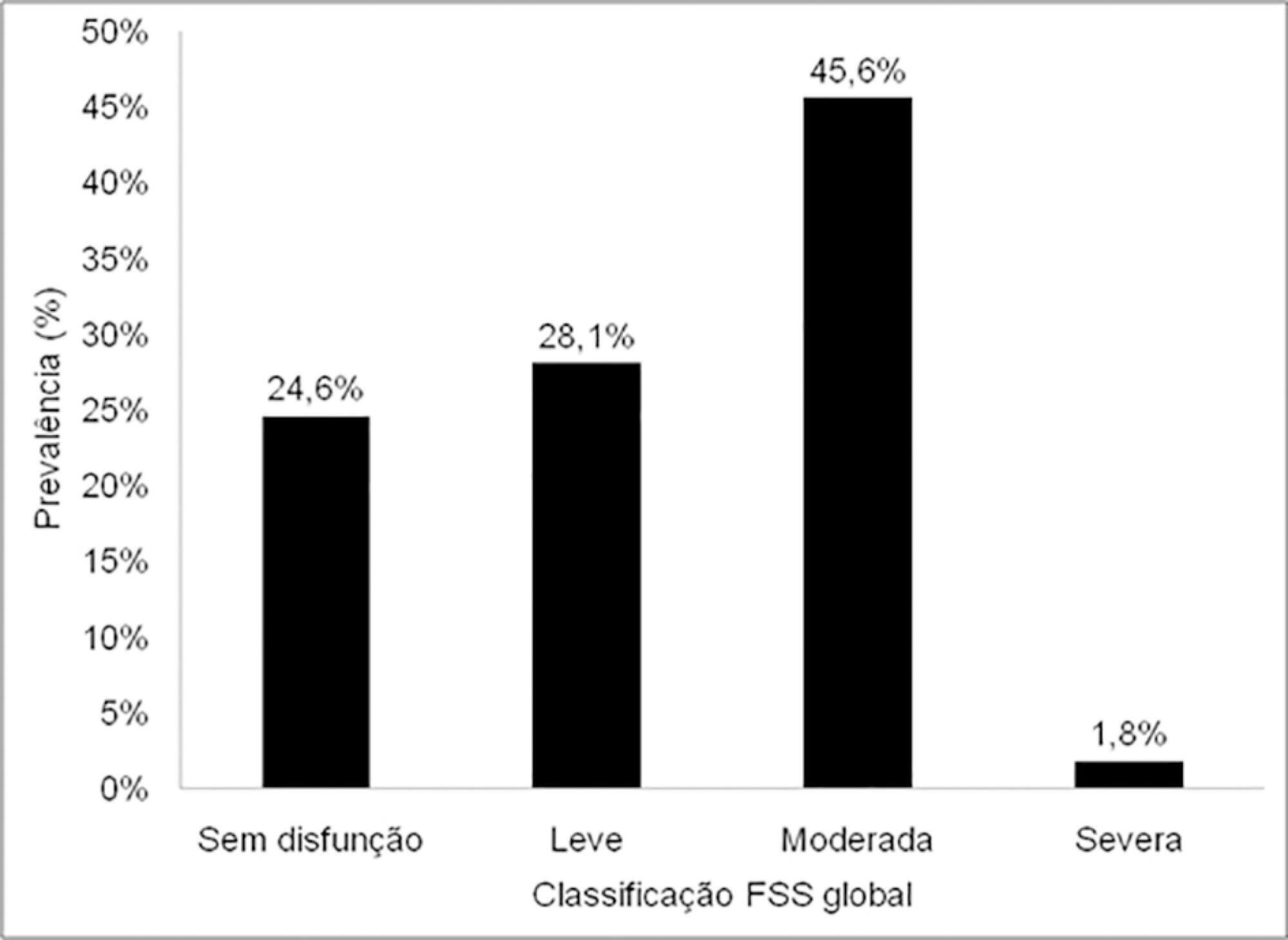
The sample comprised 57 patients with a median age of 7 months (2 - 17); 54.4% were male, and 75.5% showed dysfunction, which was moderate in 45.6% of the cases. RACHS-1 category > 3 was observed in 47% of the sample, indicating higher surgical risk. There was a correlation between functional deficit and younger age, longer duration of invasive mechanical ventilation and longer intensive care unit stay. Moreover, greater functional deficit was observed among patients classified as RACHS-1 category > 3.
The prevalence of functional deficit was high among children and adolescents with congenital heart disease after cardiac surgery. Higher surgical risk, longer duration of invasive mechanical ventilation, longer intensive care unit stay and younger age were correlated with worse functional status.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):393-402
DOI 10.5935/0103-507X.20190062
To review the scientific evidence regarding the initiation of enteral nutrition in the pediatric burn population.
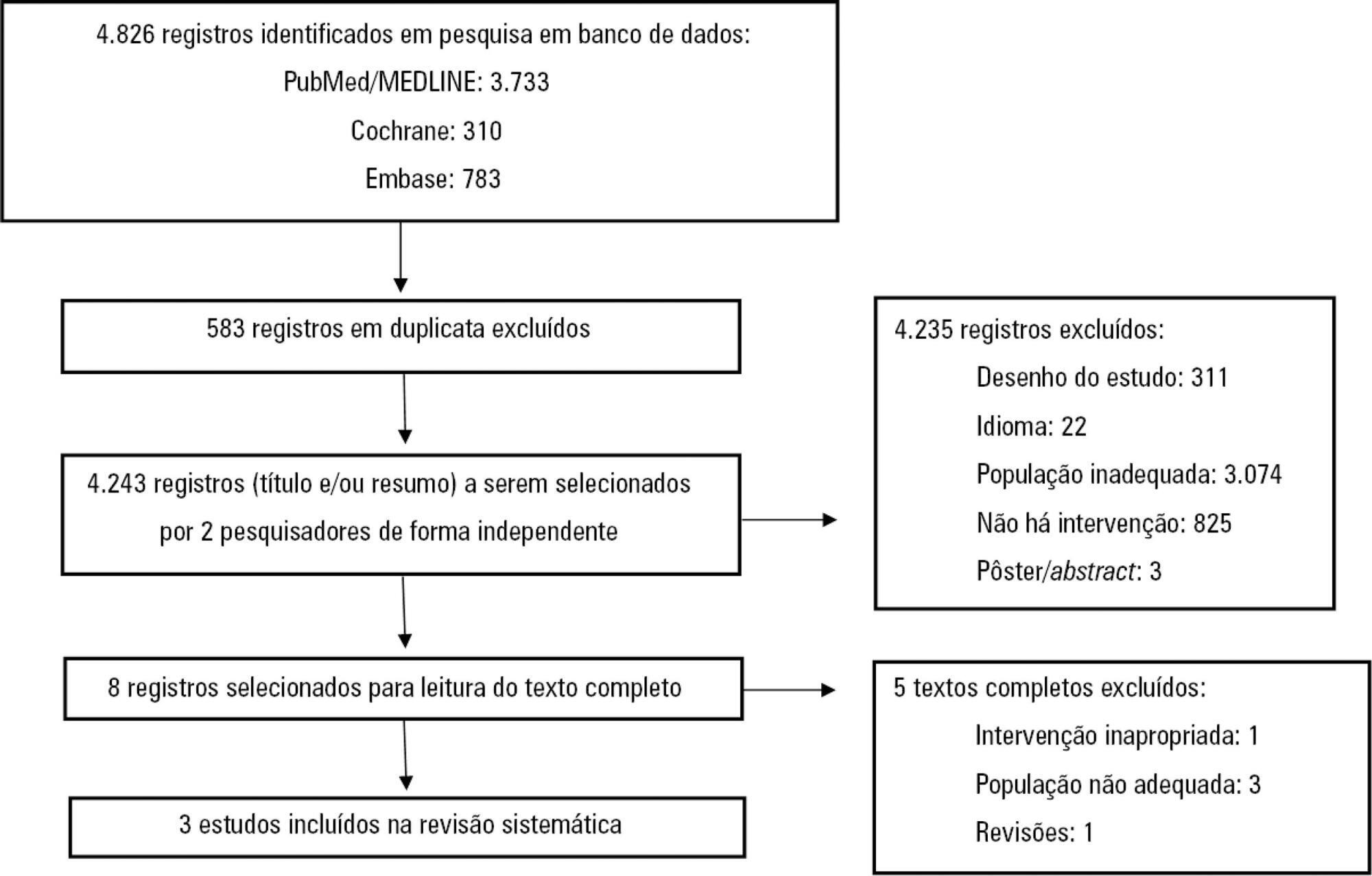
This study was a systematic review and meta-analysis of randomized clinical trials comparing early enteral nutrition and late enteral nutrition in individuals aged 1 month to 18 years with burns. The MEDLINE/PubMed, Embase and Cochrane Library databases were searched using the terms "burns", "fires", "child nutrition disorders", "nutritional support" and related terms.
Three articles that included a total of 781 patients were identified. There was no significant difference in the mortality rate between the early and late groups (OR = 0.72, 95%CI = 0.46 - 1.15, p = 0.17). Patients who received early enteral nutrition had a 3.69-day reduction in the length of hospital stay (mean difference = -3.69, 95%CI = -4.11 - -3.27, p < 0.00001). There was a higher incidence of diarrhea and vomiting and decreased intestinal permeability in the early group. This group also presented higher a serum insulin concentration and insulin/glucagon ratio as well as lower caloric deficit and weight loss when compared to the control group.
Analysis of the different intragroup variables suggests the importance of starting nutritional support early. Considering the number of pediatric burn patients, there is a need for robust studies with greater scientific impact.
Abstract
Rev Bras Ter Intensiva. 2019;31(3):333-339
DOI 10.5935/0103-507X.20190045
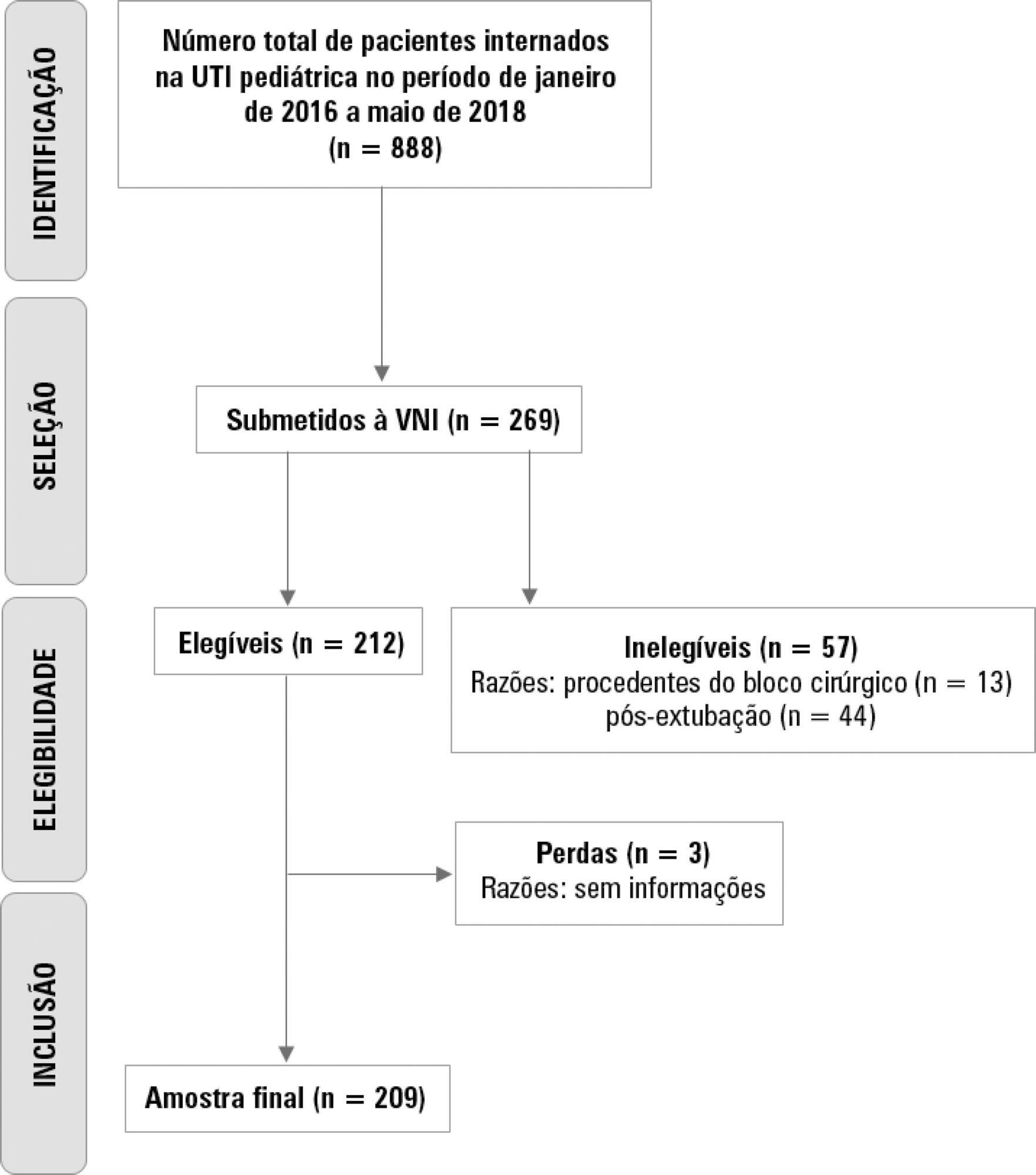
To describe the use of noninvasive ventilation to prevent tracheal intubation in children in a pediatric intensive care unit and to analyze the factors related to respiratory failure.
A retrospective cohort study was performed from January 2016 to May 2018. The study population included children aged 1 to 14 years who were subjected to noninvasive ventilation as the first therapeutic choice for acute respiratory failure. Biological, clinical and managerial data were analyzed by applying a model with the variables that obtained significance ≤ 0.20 in a bivariate analysis. Logistic regression was performed using the ENTER method. The level of significance was set at 5%.
The children had a mean age of 68.7 ± 42.3 months, 96.6% had respiratory disease as a primary diagnosis, and 15.8% had comorbidities. Of the 209 patients, noninvasive ventilation was the first option for ventilatory support in 86.6% of the patients, and the fraction of inspired oxygen was ≥ 0.40 in 47% of the cases. The lethality rate was 1.4%. The data for the use of noninvasive ventilation showed a high success rate of 95.3% (84.32 - 106). The Pediatric Risk of Mortality (PRISM) score and the length of stay in the intensive care unit were the significant clinical variables for the success or failure of noninvasive ventilation.
A high rate of effectiveness was found for the use of noninvasive ventilation for acute episodes of respiratory failure. A higher PRISM score on admission, comorbidities associated with respiratory symptoms and oxygen use ≥ 40% were independent factors related to noninvasive ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2019;31(2):248-257
DOI 10.5935/0103-507X.20190038
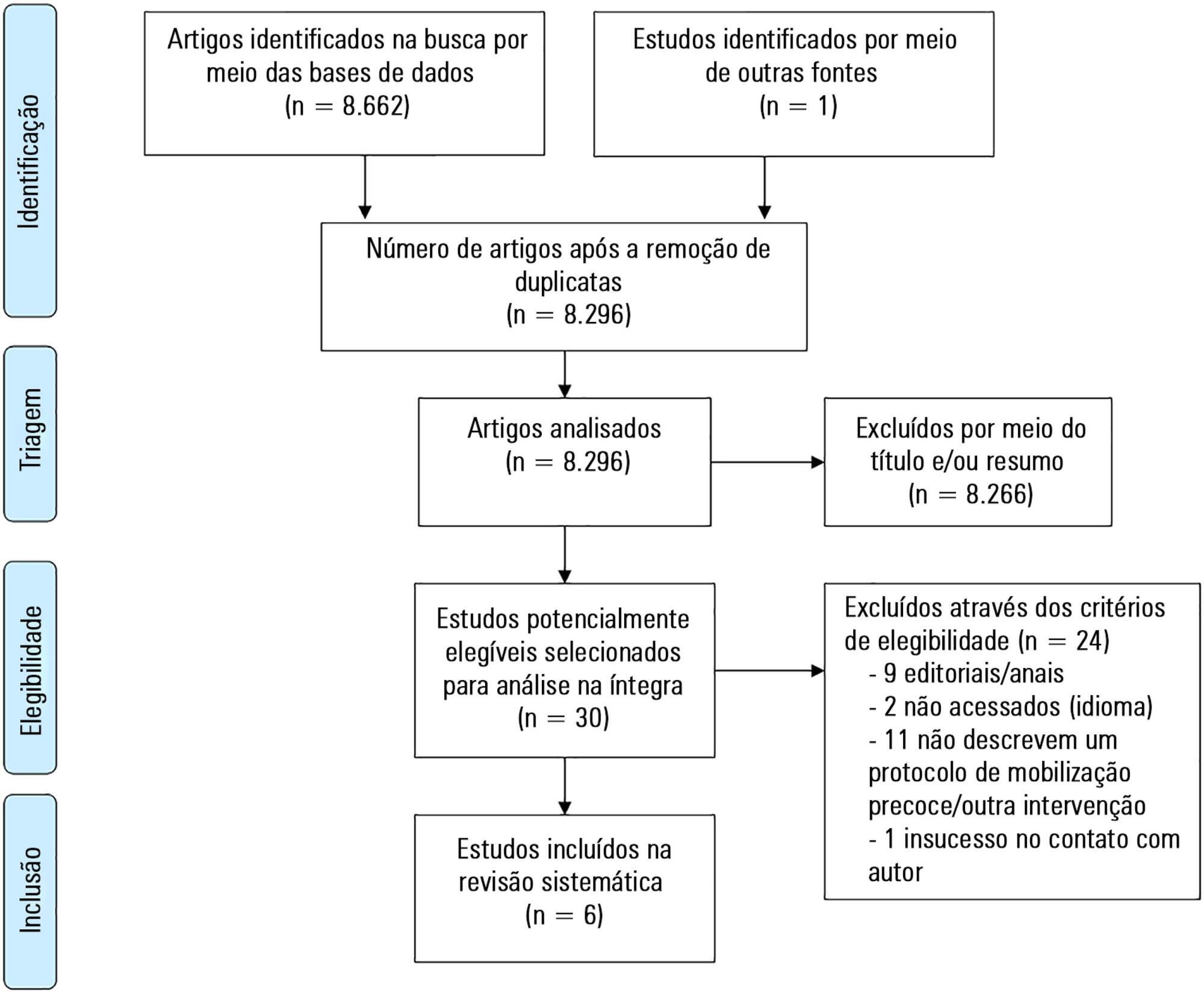
To describe the existing early mobilization protocols in pediatric intensive care units.
A systematic literature review was performed using the databases MEDLINE®, Embase, SciELO, LILACS and PeDRO, without restrictions of date and language. Observational and randomized and nonrandomized clinical trials that described an early mobilization program in patients aged between 29 days and 18 years admitted to the pediatric intensive care unit were included. The methodological quality of the studies was evaluated using the Newcastle-Ottawa Scale, Methodological Index for Non-Randomized Studies and the Cochrane Collaboration.
A total of 8,663 studies were identified, of which 6 were included in this review. Three studies described the implementation of an early mobilization program, including activities such as progressive passive mobilization, positioning, and discussion of mobilization goals with the team, in addition to contraindications and interruption criteria. Cycle ergometer and virtual reality games were also used as resources for mobilization. Four studies considered the importance of the participation of the multidisciplinary team in the implementation of early mobilization protocols.
In general, early mobilization protocols are based on individualized interventions, depending on the child's development. In addition, the use of a cycle ergometer may be feasible and safe in this population. The implementation of institutional and multidisciplinary protocols may contribute to the use of early mobilization in pediatric intensive care units; however, studies demonstrating the efficacy of such intervention are needed.
Abstract
Rev Bras Ter Intensiva. 2018;30(3):333-337
DOI 10.5935/0103-507X.20180045
To analyze the characteristics and outcomes of children hospitalized for burns in a pediatric trauma intensive care unit for burn patients.
An observational study was conducted through the retrospective analysis of children (< 16 years) admitted to the pediatric trauma intensive care unit for burn victims between January 2013 and December 2015. Sociodemographic and clinical variables were analyzed including the causal agent, burned body surface, presence of inhalation injury, length of hospital stay and mortality.
The study analyzed a sum of 140 patients; 61.8% were male, with a median age of 24 months and an overall mortality of 5%. The main cause of burns was scalding (51.4%), followed by accidents involving fire (38.6%) and electric shock (6.4%). Mechanical ventilation was used in 20.7% of the cases. Associated inhalation injury presented a relative risk of 6.1 (3.5 - 10.7) of needing ventilatory support and a relative risk of mortality of 14.1 (2.9 - 68.3) compared to patients without this associated injury. A significant connection was found between burned body surface and mortality (p < 0.002), reaching 80% in patients with a burned area greater than 50%. Patients who died had a significantly higher Tobiasen Abbreviated Burn Severity Index than survivors (9.6 ± 2.2 versus 4.4 ± 1.1; p < 0.001). A Tobiasen Abbreviated Burn Severity Index ≥ 7 represented a relative risk of death of 68.4 (95%CI 9.1 - 513.5).
Scalding burns are quite frequent and are associated with high morbidity. Mortality is associated with the amount of burned body surface and the presence of inhalation injury. Special emphasis should be given to accidents involving fire, reinforcing proper diagnosis and treatment of inhalation injury.