Abstract
Rev Bras Ter Intensiva. 2014;26(2):130-136
DOI 10.5935/0103-507X.20140019
To assess the performance of central venous oxygen saturation, lactate, base deficit, and C-reactive protein levels and SOFA and SWIFT scores on the day of discharge from the intensive care unit as predictors of patient readmission to the intensive care unit.
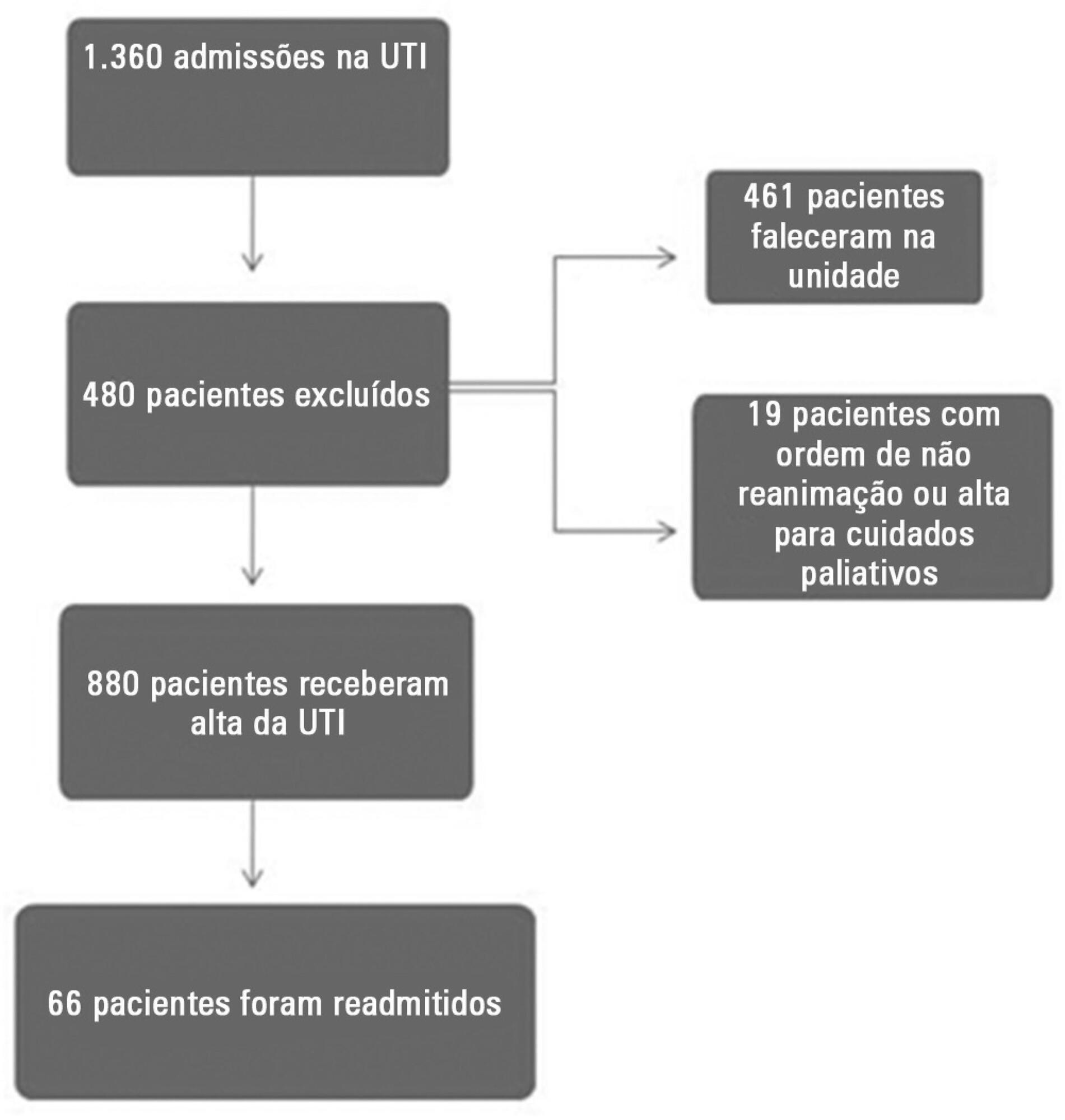
This prospective and observational study collected data from 1,360 patients who were admitted consecutively to a clinical-surgical intensive care unit from August 2011 to August 2012. The clinical characteristics and laboratory data of readmitted and non-readmitted patients after discharge from the intensive care unit were compared. Using a multivariate analysis, the risk factors independently associated with readmission were identified.
The C-reactive protein, central venous oxygen saturation, base deficit, and lactate levels and the SWIFT and SOFA scores did not correlate with the readmission of critically ill patients. Increased age and contact isolation because of multidrug-resistant organisms were identified as risk factors that were independently associated with readmission in this study group.
Inflammatory and perfusion parameters were not associated with patient readmission. Increased age and contact isolation because of multidrug-resistant organisms were identified as predictors of readmission to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):7-13
DOI 10.5935/0103-507X.20140002
To evaluate the role of quality indicators and adverse events registering in the quality assessment of intensive care physiotherapy and to evaluate the impact of implementing protocolized care and professional training in the quality improvement process.
A prospective before-after study was designed to assess 15 indicators of the quality of care. Baseline compliance and adverse events were collected before and after the implementation of treatment protocols and staff training.
Eighty-nine patients admitted, being 48 in the pre-intervention period and 41 in the post-intervention period with a total of 1246 and 1191 observations respectively. Among the indicators related to the global population, there was a significant improvement in chest x-ray control, multidisciplinary rounds and shift changes as well as in compliance with these decisions. Indicators related to the population under mechanical ventilation, obtained by direct observation at bedside, showed a significant improvement in the compliance with the tidal volume of 6-8mL/Kg, plateau pressure <30cmH2O, adequate mechanical ventilation alarm setting, mechanical ventilation humidification control, adequate humidification line exchange and orotracheal tube position. Among the mechanical ventilation indicators collected through the physiotherapy records, there was significantly improved compliance with the predicted tidal volume registry and cuff pressure registry. There was a significant reduction in the number of adverse events. There was no impact on intensive care unit mortality, length of stay, duration of mechanical ventilation and ventilator-free days.
It is possible to measure the quality of physiotherapy care using indicators of quality control. The implementation of care protocols and training of the professionals can improve team performance.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):143-147
DOI 10.5935/0103-507X.20140021
To evaluate the behavior of fractional excretion of potassium in the course of acute kidney injury in critically ill patients.
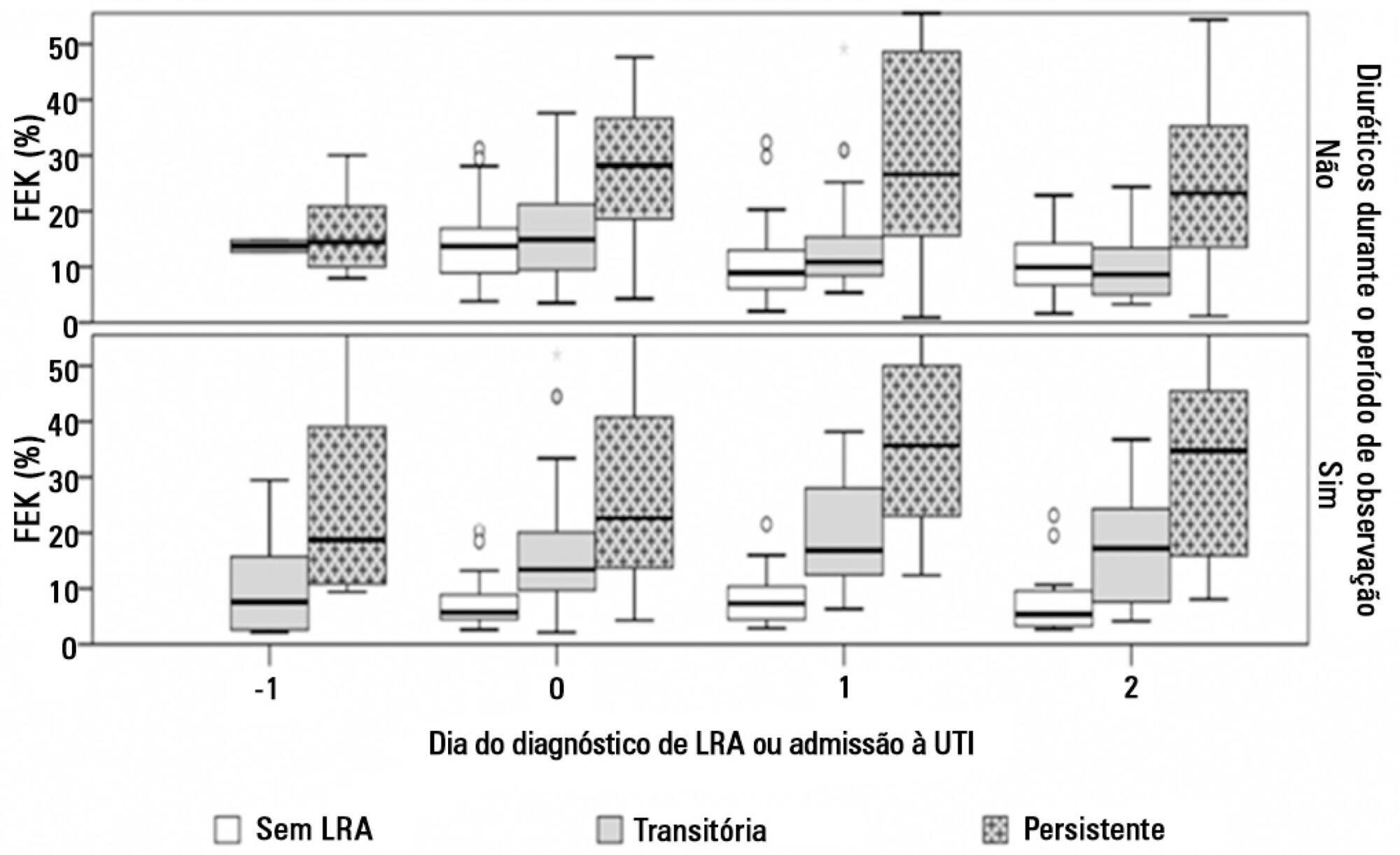
As part of a larger study in which we have evaluated blood and urinary parameters in the course of acute kidney injury, 168 patients were included. Blood and urine samples were collected daily until the removal of the urinary catheter or the initiation of renal replacement therapy. We describe the evolution of fractional excretion of potassium based on whether acute kidney injury was diagnosed, its duration (transient or persistent) and its severity (creatinine-based Acute Kidney Injury Network - AKIN stage). The diagnostic performance of fractional excretion of potassium in predicting the duration of acute kidney injury and the need for renal replacement therapy on the day of acute kidney injury diagnosis was also evaluated.
Fractional excretion of potassium was significantly higher in persistent acute kidney injury compared to transient acute kidney injury on the day of acute kidney injury diagnosis (24.8 vs. 13.8%, p<0.001). Both groups had the median fractional excretion of potassium increasing in the two days preceding the acute kidney injury diagnosis. Patients without acute kidney injury had stable low fractional excretion of potassium values. The fractional excretion of potassium was fairly accurate in predicting persistent acute kidney injury (area under the curve: 0.712; 95% confidence interval: 0.614-0.811; p<0.001) on the day of acute kidney injury diagnosis. The area under the curve was 0.663 (95% confidence interval: 0.523-0.803; p=0.03) for renal replacement therapy. The fractional excretion of potassium increased with maximum AKIN stage reached, in both transient and persistent acute kidney injury.
Sequential fractional excretion of potassium assessment appears to be useful in critically ill patients at risk for acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):148-154
DOI 10.5935/0103-507X.20140022
Patients with traumatic brain injury are particularly susceptible to sepsis, which may exacerbate the systemic inflammatory response and lead to organ dysfunction. The influence of clinical variables on the mortality of intensive care unit patients with traumatic brain injury and sepsis was investigated.
The present investigation was a retrospective study involving 175 patients with traumatic brain injury who were treated in a period of 1 year at a reference hospital for trauma and who had sepsis, severe sepsis, or septic shock. Demographic and clinical data were obtained, and the SOFA score was calculated at the time sepsis was found and after 72 hours.
There was a predominance of young men with severe traumatic brain injury, multiple head injuries, sepsis with a pulmonary focus, prolonged hospital stay, and high mortality (37.7%). Circulatory and respiratory failure had a high incidence, but renal and coagulation failure were less frequent, and liver failure was not observed. After logistic regression, the presence of septic shock and respiratory failure 72 hours after the sepsis diagnosis was associated with higher mortality, with an odds ratio of 7.56 (95%CI=2.04-27.31, p=0.0024) and 6.62 (95%CI=1.93-22.78, p=0.0027), respectively. In addition, there was a higher mortality among patients who had no organ failure on D1 but who developed the condition after 72 hours of sepsis and in those patients who already had organ failure at the time sepsis was diagnosed and remained in this condition after 72 hours.
Septic shock and progressive organ (particularly respiratory) dysfunction increases the mortality of patients with traumatic brain injury and sepsis.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):163-168
DOI 10.5935/0103-507X.20140024
To compare the effectiveness of the alveolar recruitment maneuver and the breath stacking technique with respect to lung mechanics and gas exchange in patients with acute lung injury.
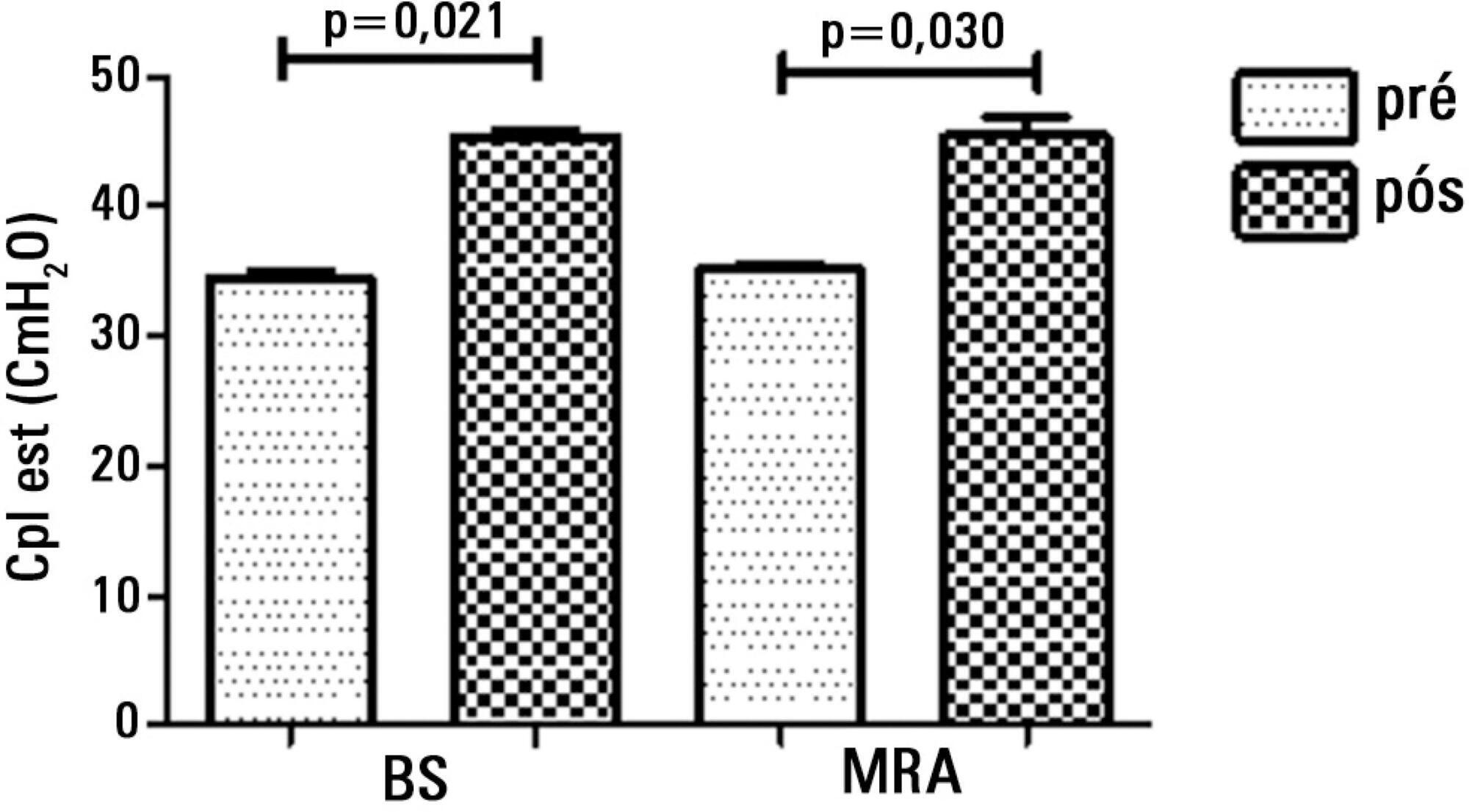
Thirty patients were distributed into two groups: Group 1 - breath stacking; and Group 2 - alveolar recruitment maneuver. After undergoing conventional physical therapy, all patients received both treatments with an interval of 1 day between them. In the first group, the breath stacking technique was used initially, and subsequently, the alveolar recruitment maneuver was applied. Group 2 patients were initially subjected to alveolar recruitment, followed by the breath stacking technique. Measurements of lung compliance and airway resistance were evaluated before and after the use of both techniques. Gas analyses were collected before and after the techniques were used to evaluate oxygenation and gas exchange.
Both groups had a significant increase in static compliance after breath stacking (p=0.021) and alveolar recruitment (p=0.03), but with no significant differences between the groups (p=0.95). The dynamic compliance did not increase for the breath stacking (p=0.22) and alveolar recruitment (p=0.074) groups, with no significant difference between the groups (p=0.11). The airway resistance did not decrease for either groups, i.e., breath stacking (p=0.91) and alveolar recruitment (p=0.82), with no significant difference between the groups (p=0.39). The partial pressure of oxygen increased significantly after breath stacking (p=0.013) and alveolar recruitment (p=0.04), but there was no significant difference between the groups (p=0.073). The alveolar-arterial O2 difference decreased for both groups after the breath stacking (p=0.025) and alveolar recruitment (p=0.03) interventions, and there was no significant difference between the groups (p=0.81).
Our data suggest that the breath stacking and alveolar recruitment techniques are effective in improving the lung mechanics and gas exchange in patients with acute lung injury.
Abstract
Rev Bras Ter Intensiva. 2014;26(2):155-162
DOI 10.5935/0103-507X.20140023
To determine the factors that influence the adequacy of enteral nutritional therapy in an intensive care unit.
This prospective observational study was conducted in an intensive care unit between 2010 and 2012. Patients >18 years of age underwent exclusive enteral nutritional therapy for ≥72 hours. The energy and protein requirements were calculated according to the ICU protocols. The data regarding enteral nutrition, the causes of non-compliance, and the biochemical test results were collected daily.
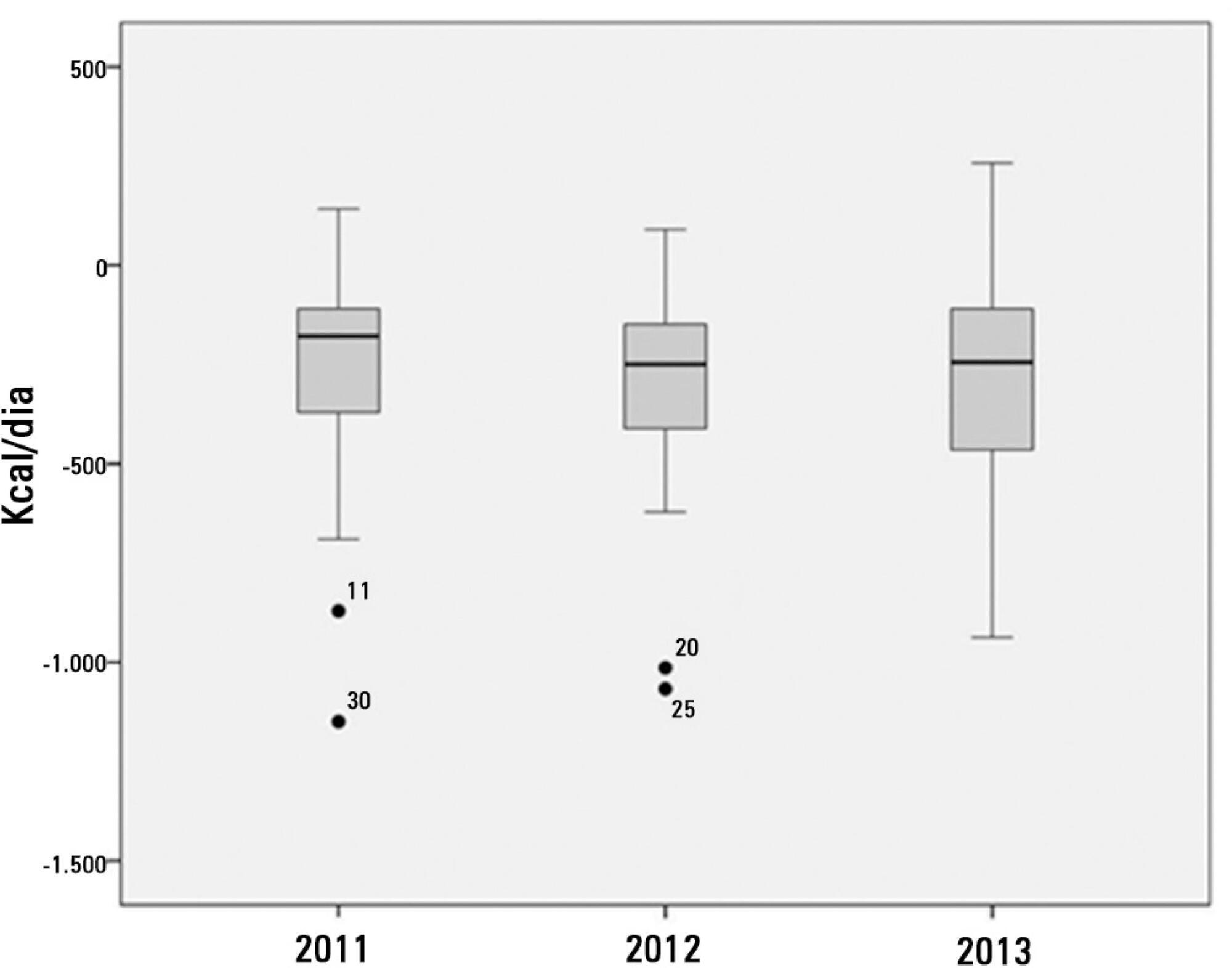
Ninety-three patients admitted to the intensive care unit were evaluated. Among these patients, 82% underwent early enteral nutritional therapy, and 80% reached the nutritional goal in <36 hours. In addition, 81.6%±15.4% of the enteral nutrition volume was infused, with an adequacy of 82.2%±16.0% for calories, 82.2%±15.9% for proteins, and a mean energy balance of -289.9±277.1kcal/day. A negative correlation of C-reactive protein with the volume infused and the energy and protein balance was observed. In contrast, a positive correlation was found between C-reactive protein and the time required to reach nutritional goals. Extubation was the main cause for interrupting the enteral nutritional therapy (29.9% of the interruption hours), and the patients >60 years of age exhibited a lower percentage of recovery of the oral route compared with the younger patients (p=0.014).
Early enteral nutritional therapy and the adequacy for both energy and protein of the nutritional volume infused were in accordance with the established guidelines. Possible inadequacies of energy and protein balance appeared to be associated with an acute inflammatory response, which was characterized by elevated C-reactive protein levels. The main cause of interruption of the enteral nutritional therapy was the time spent in extubation.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):21-27
DOI 10.5935/0103-507X.20140004
To characterize the profile of effective organ and tissue donors and to understand which organs and tissues were donated for transplantation.
This was a quantitative, descriptive, exploratory, retrospective study that analyzed clinical data from 305 donors between January 2006 to December 2010. The data were then analyzed using descriptive analyses, generating frequency tables, measures of position (mean, minimum and maximum) and measures of dispersion (standard deviation) for data that was social and clinical in nature.
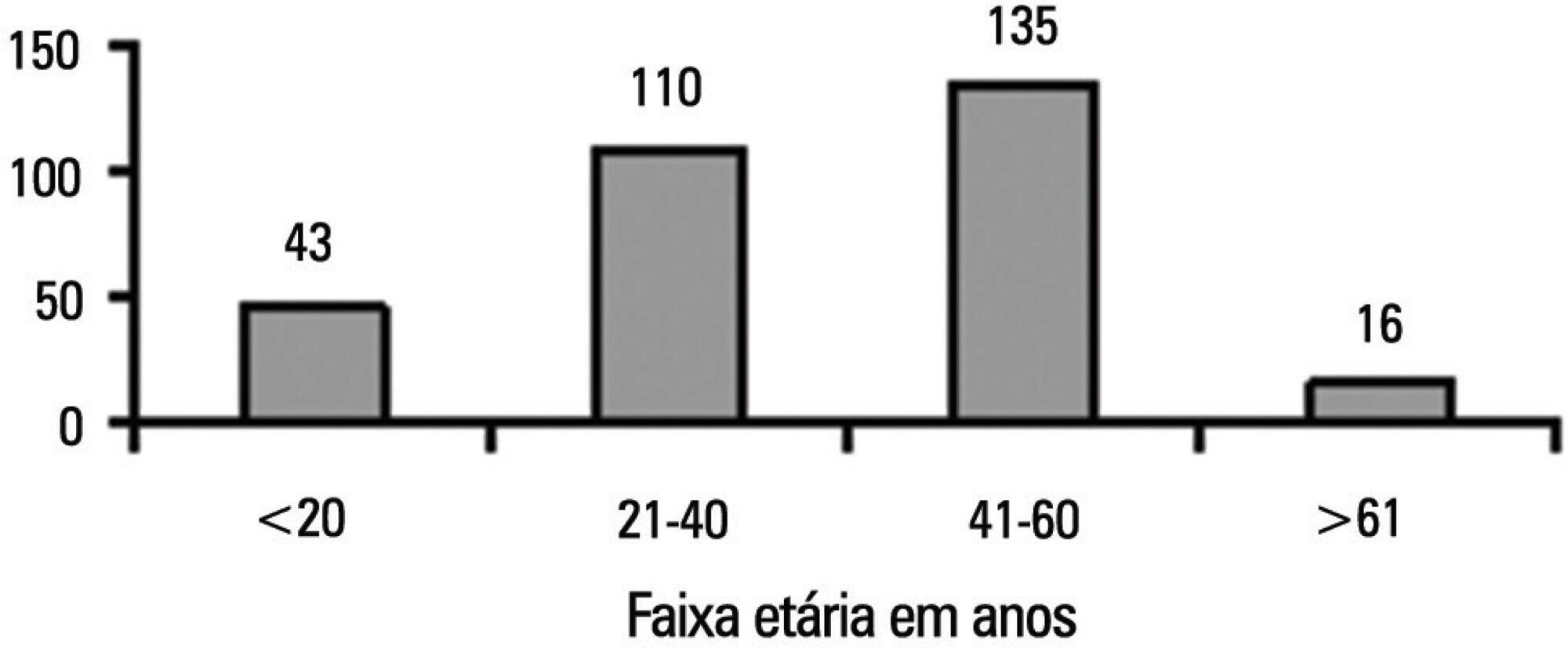
There was an overall predominance of white (72%) and male (55%) individuals between the ages of 41 and 60 years (44%). The primary cause of brain death was cerebrovascular accident (55%). In the patient history, 31% of the patients were classified as overweight, 27% as hypertensive and only 4.3% as having diabetes mellitus. Vasoactive drugs were used in 92.7% of the donors, and the main drug of choice was noradrenaline (81.6%). Hyperglycemia and hypernatremia were diagnosed in 78% and 71% of the donors, respectively.
Significant hemodynamic changes were found, and the results indicate that the use of vasoactive drugs was the main strategy used to control these changes. Furthermore, most donors presented with hyperglycemia and hypernatremia, which were frequently reported in association with brain death. The persistent nature of these findings suggests that the organ donors were inadequately maintained.