Abstract
Rev Bras Ter Intensiva. 2015;27(2):134-140
DOI 10.5935/0103-507X.20150024
The development of the extracorporeal membrane oxygenation in Latin America represents a challenge in this specialty field. The objective of this article was to describe the results of a new extracorporeal membrane oxygenation program in an intensive care unit.
This retrospective cohort study included 22 patients who required extracorporeal membrane oxygenation and were treated from January 2011 to June 2014. The baseline characteristics, indications, duration of the condition, days on mechanical ventilation, days in the intensive care unit, complications, and hospital mortality were evaluated.
Fifteen patients required extracorporeal membrane oxygenation after lung transplantation, and seven patients required oxygenation due to acute respiratory distress. All transplanted patients were weaned from extracorporeal membrane oxygenation with a median duration of 3 days (Interquartile range - IQR: 2 - 5), were on mechanical ventilation for a median of 15.5 days (IQR: 3 - 25), and had an intensive care unit stay of 31.5 days (IQR: 19 - 53) and a median hospital stay of 60 days (IQR: 36 - 89) with 20% mortality. Patients with acute respiratory distress had a median oxygenation membrane duration of 9 days (IQR: 3 - 14), median mechanical ventilation time of 25 days (IQR: 13 - 37), a 31 day stay in therapy (IQR: 11 - 38), a 32 day stay in the hospital (IQR: 11 - 41), and 57% mortality. The main complications were infections (80%), acute kidney failure (43%), bleeding at the surgical site and at the site of cannula placement (22%), plateletopenia (60%), and coagulopathy (30%).
In spite of the steep learning curve, we considered this experience to be satisfactory, with results and complications comparable to those reported in the literature.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):141-148
DOI 10.5935/0103-507X.20150025
To evaluate the impact of body mass index on the short-term prognosis of non-surgical critically ill patients while controlling for performance status and comorbidities.
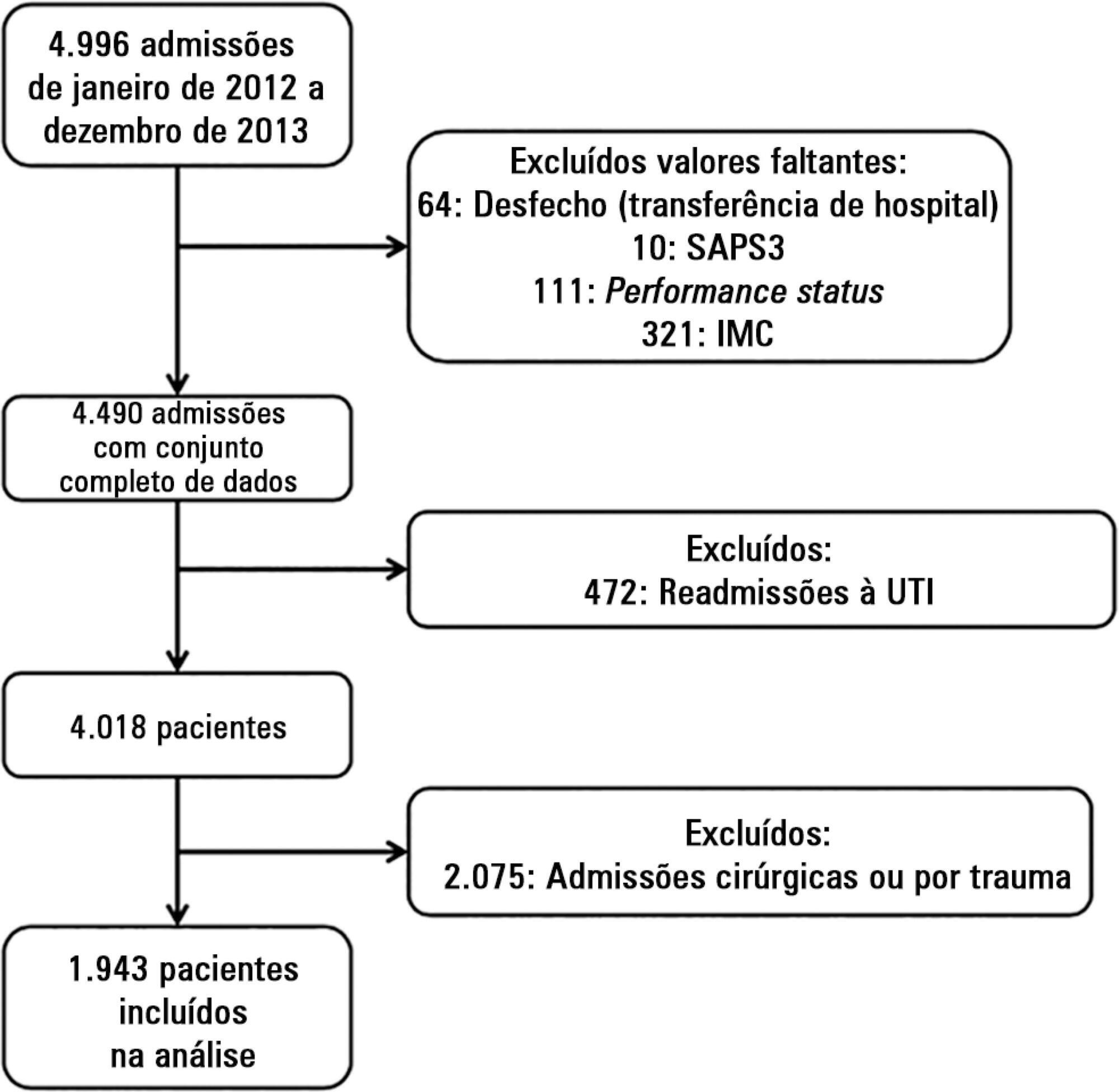
We performed a retrospective analysis on a two-year single-center database including 1943 patients. We evaluated the impact of body mass index on hospital mortality using a gradient-boosted model that also included comorbidities and was assessed by Charlson’s comorbidity index, performance status and illness severity, which was measured by the SAPS3 score. The SAPS3 score was adjusted to avoid including the same variable twice in the model. We also assessed the impact of body mass index on the length of stay in the hospital after intensive care unit admission using multiple linear regressions.
A low value (< 20kg/m2) was associated with a sharp increase in hospital mortality. Mortality tended to subsequently decrease as body mass index increased, but the impact of a high body mass index in defining mortality was low. Mortality increased as the burden of comorbidities increased and as the performance status decreased. Body mass index interacted with the impact of SAPS3 on patient outcome, but there was no significant interaction between body mass index, performance status and comorbidities. There was no apparent association between body mass index and the length of stay at the hospital after intensive care unit admission.
Body mass index does appear to influence the shortterm outcomes of critically ill medical patients, who are generally underweight. This association was independent of comorbidities and performance status.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):149-154
DOI 10.5935/0103-507X.20150026
To analyze the clinical activities performed and the accepted pharmacist recommendations made by a pharmacist as a part of his/her daily routine in an adult clinical intensive care unit over a period of three years.
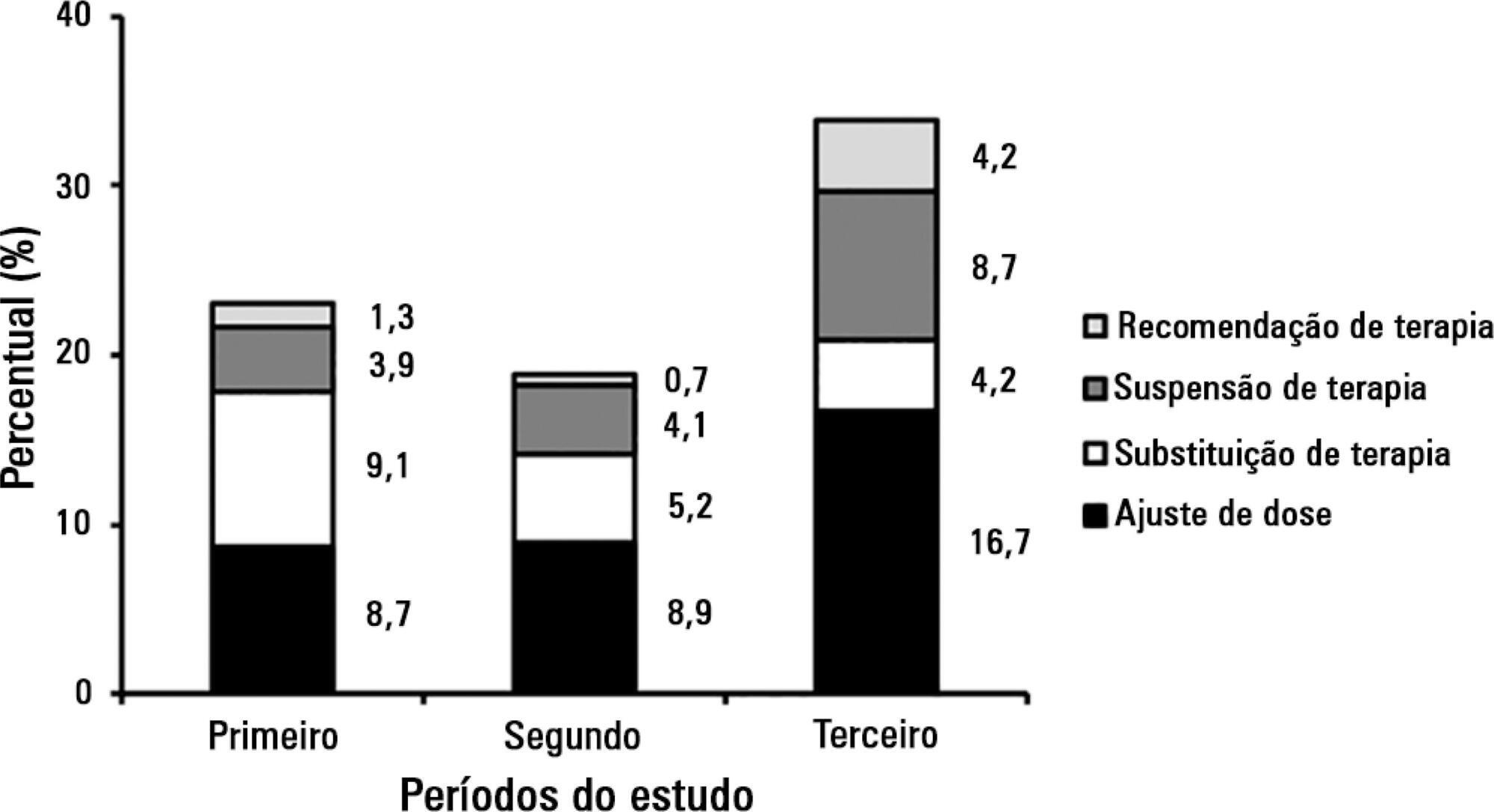
A cross-sectional, descriptive, and exploratory study was conducted at a tertiary university hospital from June 2010 to May 2013, in which pharmacist recommendations were categorized and analyzed.
A total of 834 pharmacist recommendations (278 per year, on average) were analyzed and distributed across 21 categories. The recommendations were mainly made to physicians (n = 699; 83.8%) and concerned management of dilutions (n = 120; 14.4%), dose adjustment (n = 100; 12.0%), and adverse drug reactions (n = 91; 10.9%). A comparison per period demonstrated an increase in pharmacist recommendations with larger clinical content and a reduction of recommendations related to logistic aspects, such as drug supply, over time. The recommendations concerned 948 medications, particularly including systemic anti-infectious agents.
The role that the pharmacist played in the intensive care unit of the institution where the study was performed evolved, shifting from reactive actions related to logistic aspects to effective clinical participation with the multi-professional staff (proactive actions).
Abstract
Rev Bras Ter Intensiva. 2015;27(2):155-160
DOI 10.5935/0103-507X.20150027
To evaluate the changes in ventilatory mechanics and hemodynamics that occur in patients dependent on mechanical ventilation who are subjected to a standard respiratory therapy protocol.
This experimental and prospective study was performed in two intensive care units, in which patients dependent on mechanical ventilation for more than 48 hours were consecutively enrolled and subjected to an established respiratory physiotherapy protocol. Ventilatory variables (dynamic lung compliance, respiratory system resistance, tidal volume, peak inspiratory pressure, respiratory rate, and oxygen saturation) and hemodynamic variables (heart rate) were measured one hour before (T-1), immediately after (T0) and one hour after (T+1) applying the respiratory physiotherapy protocol.
During the period of data collection, 104 patients were included in the study. Regarding the ventilatory variables, an increase in dynamic lung compliance (T-1 = 52.3 ± 16.1mL/cmH2O versus T0 = 65.1 ± 19.1mL/cmH2O; p < 0.001), tidal volume (T-1 = 550 ± 134mL versus T0 = 698 ± 155mL; p < 0.001), and peripheral oxygen saturation (T-1 = 96.5 ± 2.29% versus T0 = 98.2 ± 1.62%; p < 0.001) were observed, in addition to a reduction of respiratory system resistance (T-1 = 14.2 ± 4.63cmH2O/L/s versus T0 = 11.0 ± 3.43cmH2O/L/s; p < 0.001), after applying the respiratory physiotherapy protocol. All changes were present in the assessment performed one hour (T+1) after the application of the respiratory physiotherapy protocol. Regarding the hemodynamic variables, an immediate increase in the heart rate after application of the protocol was observed, but that increase was not maintained (T-1 = 88.9 ± 18.7 bpm versus T0 = 93.7 ± 19.2bpm versus T+1 = 88.5 ± 17.1bpm; p < 0.001).
Respiratory therapy leads to immediate changes in the lung mechanics and hemodynamics of mechanical ventilation-dependent patients, and ventilatory changes are likely to remain for at least one hour.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):161-169
DOI 10.5935/0103-507X.20150028
Evaluation of the functional outcomes of patients undergoing an early rehabilitation protocol for critically ill patients from admission to discharge from the intensive care unit.
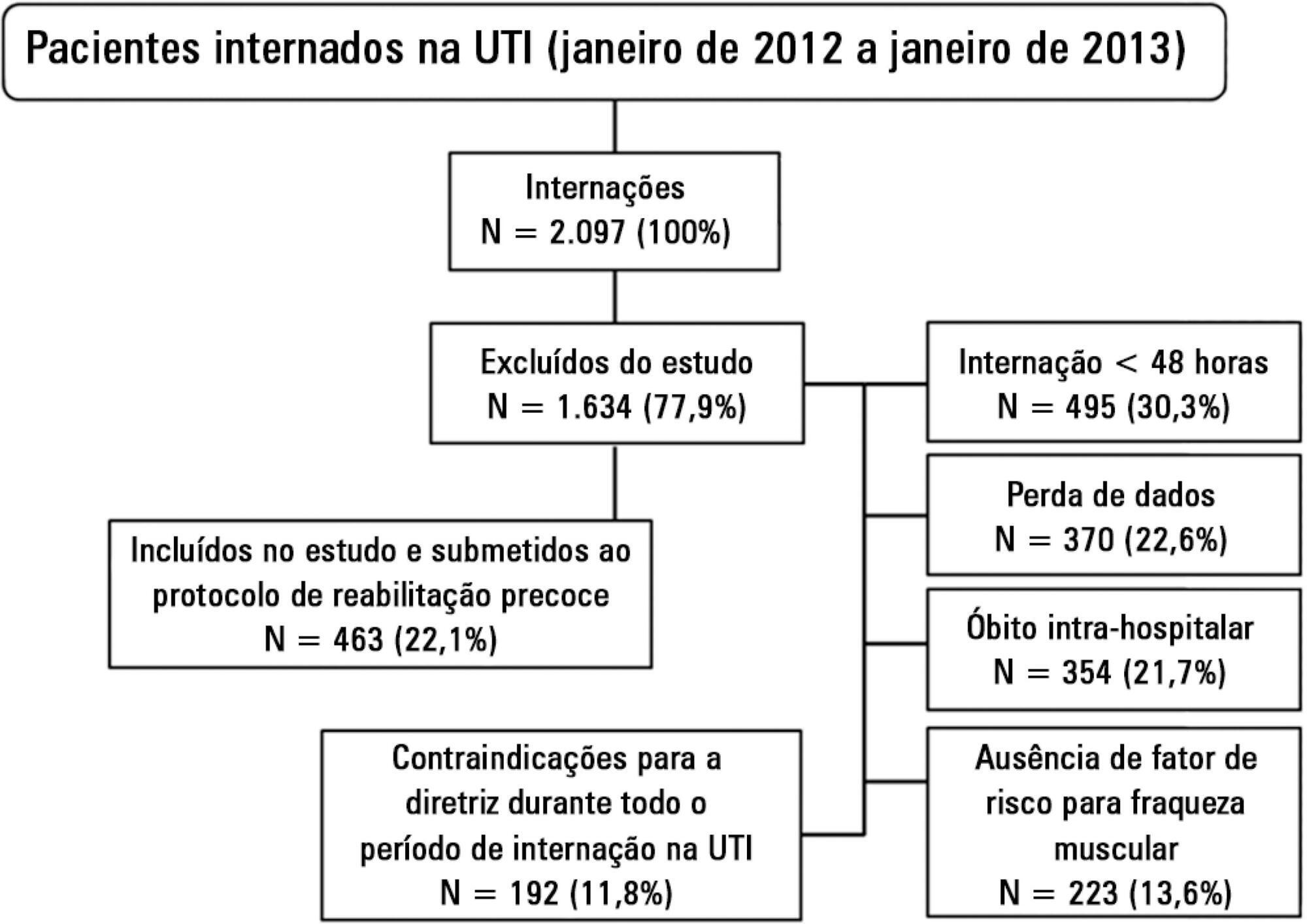
A retrospective cross-sectional study was conducted that included 463 adult patients with clinical and/or surgical diagnosis undergoing an early rehabilitation protocol. The overall muscle strength was evaluated at admission to the intensive care unit using the Medical Research Council scale. Patients were allocated to one of four intervention plans according to the Medical Research Council score, the suitability of the plan’s parameters, and the increasing scale of the plan expressing improved functional status. Uncooperative patients were allocated to intervention plans based on their functional status. The overall muscle strength and/or functional status were reevaluated upon discharge from the intensive care unit by comparison between the Intervention Plans upon admission (Planinitial) and discharge (Planfinal). Patients were classified into three groups according to the improvement of their functional status or not: responsive 1 (Planfinal > Planinitial), responsive 2 (Planfinal = Planinitial) and unresponsive (Planfinal < Planinitial).
In total, 432 (93.3%) of 463 patients undergoing the protocol responded positively to the intervention strategy, showing maintenance and/or improvement of the initial functional status. Clinical patients classified as unresponsive were older (74.3 ± 15.1 years of age; p = 0.03) and had longer lengths of intensive care unit (11.6 ± 14.2 days; p = 0.047) and hospital (34.5 ± 34.1 days; p = 0.002) stays.
The maintenance and/or improvement of the admission functional status were associated with shorter lengths of intensive care unit and hospital stays. The results suggest that the type of diagnosis, clinical or surgical, fails to define the positive response to an early rehabilitation protocol.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):170-177
DOI 10.5935/0103-507X.20150029
The aim of this study was to investigate whether plasma serotonin levels or acetylcholinesterase activities determined upon intensive care unit admission could predict the occurrence of acute brain dysfunction in intensive care unit patients.
A prospective cohort study was conducted with a sample of 77 non-consecutive patients observed between May 2009 and September 2010. Delirium was determined using the Confusion Assessment Method for the Intensive Care Unit tool, and the acetylcholinesterase and serotonin measurements were determined from blood samples collected up to a maximum of 24 h after the admission of the patient to the intensive care unit.
In the present study, 38 (49.6%) patients developed delirium during their intensive care unit stays. Neither serum acetylcholinesterase activity nor serotonin level was independently associated with delirium. No significant correlations of acetylcholinesterase activity or serotonin level with delirium/coma-free days were observed, but in the patients who developed delirium, there was a strong negative correlation between the acetylcholinesterase level and the number of delirium/coma-free days, indicating that higher acetylcholinesterase levels are associated with fewer days alive without delirium or coma. No associations were found between the biomarkers and mortality.
Neither serum acetylcholinesterase activity nor serotonin level was associated with delirium or acute brain dysfunction in critically ill patients. Sepsis did not modify these relationships.
Abstract
Rev Bras Ter Intensiva. 2015;27(2):178-184
DOI 10.5935/0103-507X.20150030
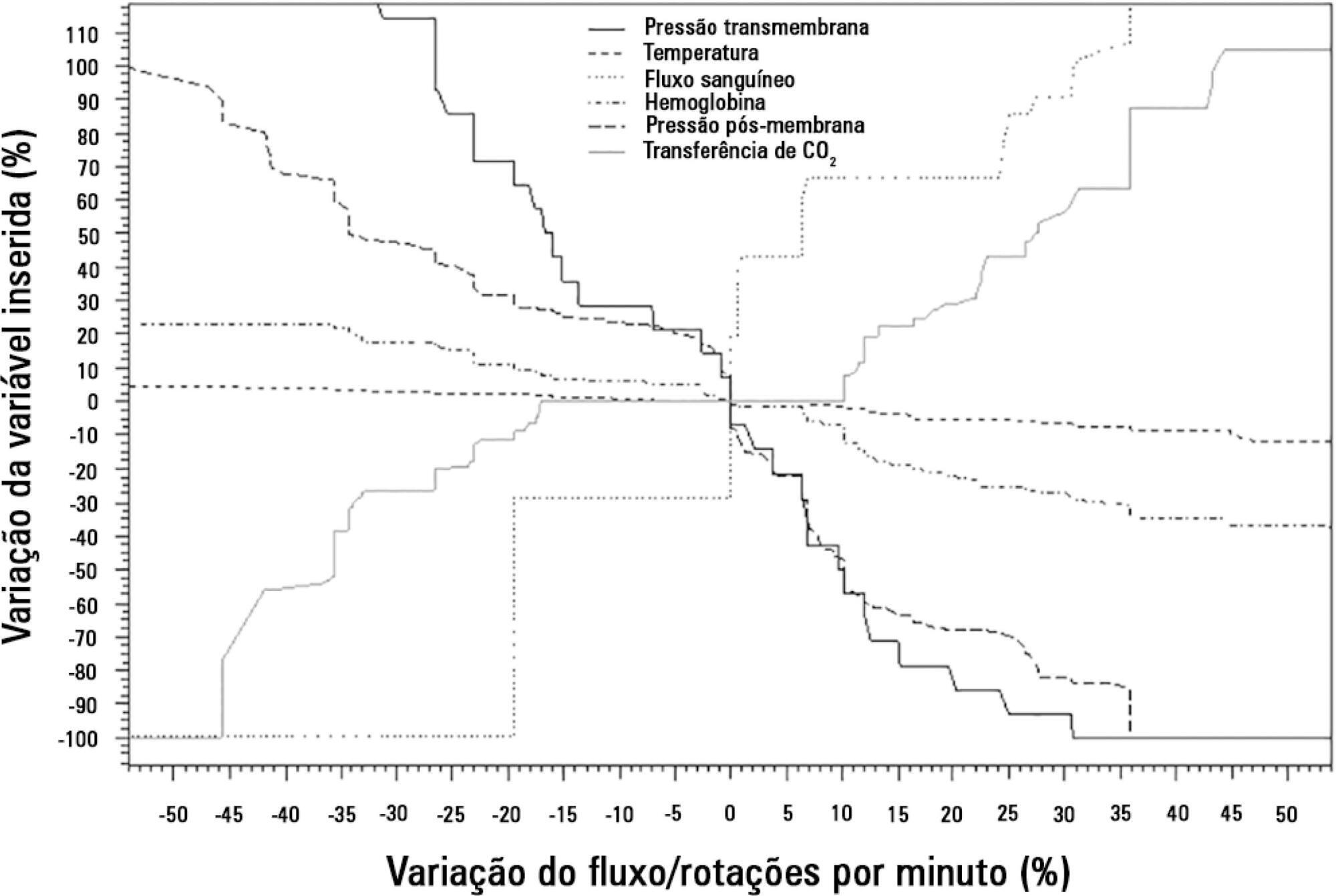
To analyze the correlations of the blood flow/pump rotation ratio and the transmembrane pressure, CO2 and O2 transfer during the extracorporeal respiratory support.
Five animals were instrumented and submitted to extracorporeal membrane oxygenation in a five-step protocol, including abdominal sepsis and lung injury.
This study showed that blood flow/pump rotations ratio variations are dependent on extracorporeal membrane oxygenation blood flow in a positive logarithmic fashion. Blood flow/pump rotation ratio variations are negatively associated with transmembrane pressure (R2 = 0.5 for blood flow = 1500mL/minute and R2 = 0.4 for blood flow = 3500mL/minute, both with p < 0.001) and positively associated with CO2 transfer variations (R2 = 0.2 for sweep gas flow ≤ 6L/minute, p < 0.001, and R2 = 0.1 for sweep gas flow > 6L/minute, p = 0.006), and the blood flow/pump rotation ratio is not associated with O2 transfer variations (R2 = 0.01 for blood flow = 1500mL/minute, p = 0.19, and R2 = - 0.01 for blood flow = 3500 mL/minute, p = 0.46).
Blood flow/pump rotation ratio variation is negatively associated with transmembrane pressure and positively associated with CO2 transfer in this animal model. According to the clinical situation, a decrease in the blood flow/pump rotation ratio can indicate artificial lung dysfunction without the occurrence of hypoxemia.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):1-6
DOI 10.5935/0103-507X.20140001
To evaluate the satisfaction of the intensive care unit staff with a computerized physician order entry and to compare the concept of the computerized physician order entry relevance among intensive care unit healthcare workers.
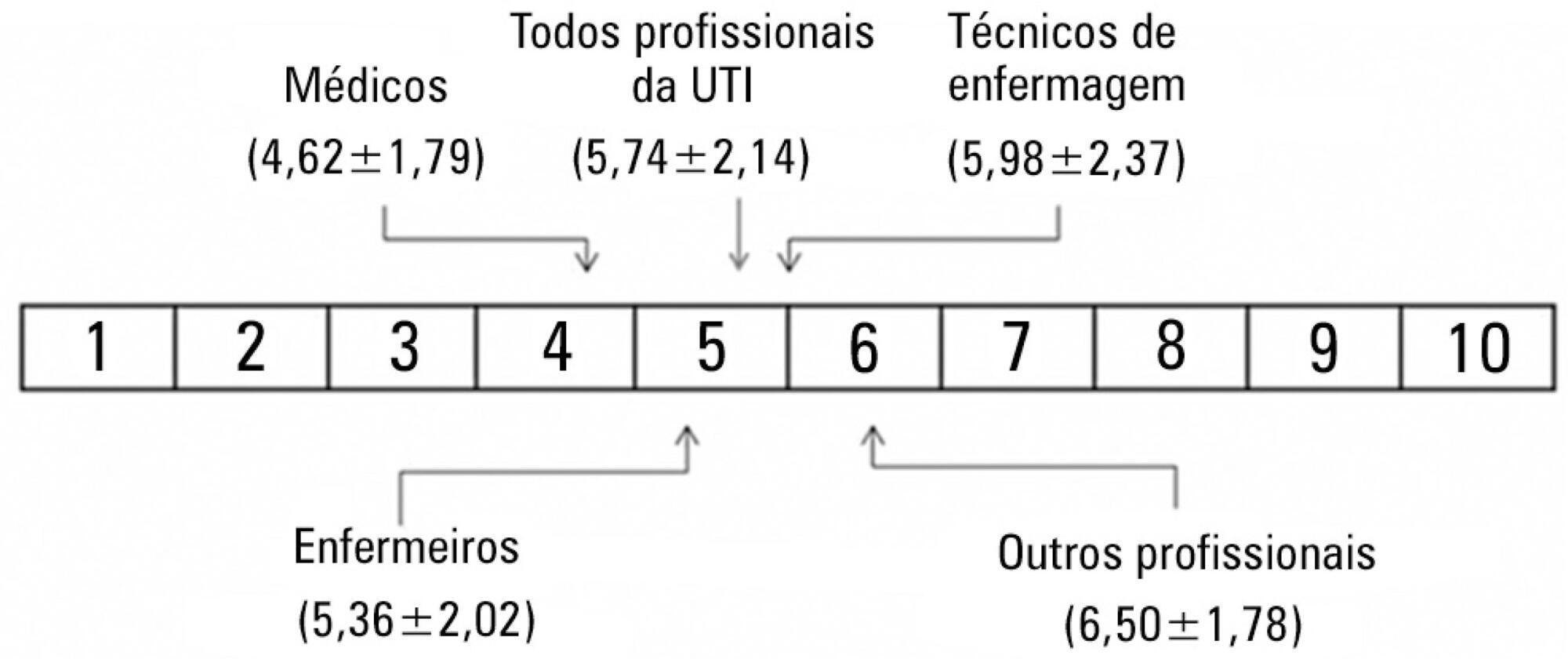
We performed a cross-sectional survey to assess the satisfaction of the intensive care unit staff with the computerized physician order entry in a 30-bed medical/surgical adult intensive care unit using a self-administered questionnaire. The questions used for grading satisfaction levels were answered according to a numerical scale that ranged from 1 point (low satisfaction) to 10 points (high satisfaction).
The majority of the respondents (n=250) were female (66%) between the ages of 30 and 35 years of age (69%). The overall satisfaction with the computerized physician order entry scored 5.74±2.14 points. The satisfaction was lower among physicians (n=42) than among nurses, nurse technicians, respiratory therapists, clinical pharmacists and diet specialists (4.62±1.79 versus 5.97±2.14, p<0.001); satisfaction decreased with age (p<0.001). Physicians scored lower concerning the potential of the computerized physician order entry for improving patient safety (5.45±2.20 versus 8.09±2.21, p<0.001) and the ease of using the computerized physician order entry (3.83±1.88 versus 6.44±2.31, p<0.001). The characteristics independently associated with satisfaction were the system's user-friendliness, accuracy, capacity to provide clear information, and fast response time.
Six months after its implementation, healthcare workers were satisfied, albeit not entirely, with the computerized physician order entry. The overall users' satisfaction with computerized physician order entry was lower among physicians compared to other healthcare professionals. The factors associated with satisfaction included the belief that digitalization decreased the workload and contributed to the intensive care unit quality with a user-friendly and accurate system and that digitalization provided concise information within a reasonable time frame.