Abstract
Rev Bras Ter Intensiva. 2014;26(1):28-35
DOI 10.5935/0103-507X.20140005
To define the characteristics and measure the reaction time of a health care team monitoring alarms in the intensive care unit.
A quantitative, observational, and descriptive study developed at the coronary care unit of a cardiology public hospital in Rio de Janeiro state (RJ). Data were obtained from the information collected on the patients, the monitoring used, and the measurement of the team's reaction time to the alarms of multi-parameter monitors during a non-participatory field observation.
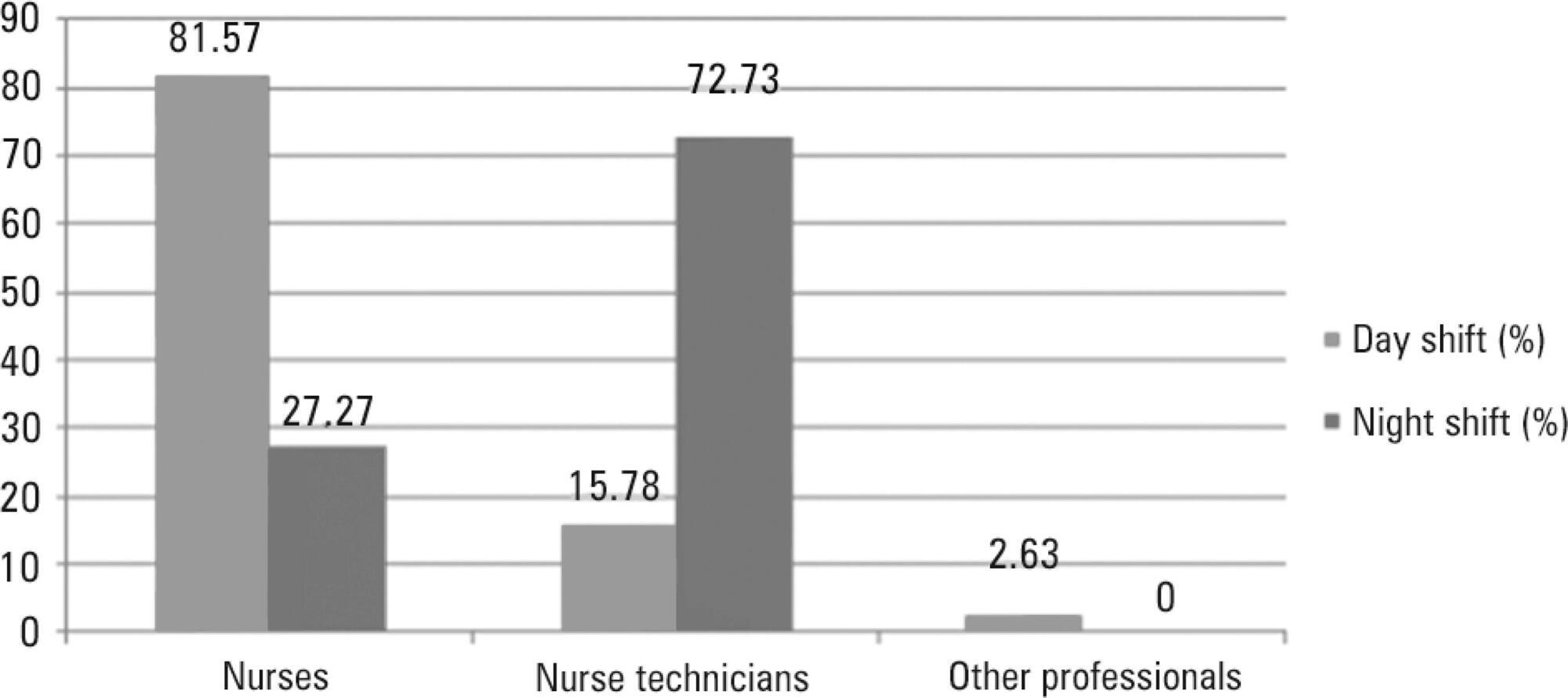
Eighty-eight patients were followed (49 during the day shift and 39 during the night shift). During the 40 hours of observation (20 hours during the day shift and 20 hours during the night shift), the total number of monitoring alarms was 227, with 106 alarms during the day shift and 121 during the night shift, an average of 5.7 alarms/hour. In total, 145 alarms unanswered by the team were observed, with 68 occurring during the day shift (64.15%) and 77 during the night shift (63.64%). This study demonstrated that the reaction time was longer than 10 minutes in more than 60% of the alarms, which were considered as unanswered alarms. The median reaction time of the answered alarms was 4 minutes and 54 seconds during the day shift and 4 minutes and 55 seconds during the night shift. The respiration monitoring was activated in only nine patients (23.07%) during the night shift. Regarding the alarm quality of these variables, the arrhythmia alarm was qualified in only 10 (20.40%) of the day-shift patients and the respiration alarm in four night-shift patients (44.44%).
The programming and configuration of the physiological variables monitored and the parameters of alarms in the intensive care unit were inadequate; there was a delay and lack of response to the alarms, suggesting that relevant alarms may have been ignored by the health care team, thus compromising the patient safety.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):36-43
DOI 10.5935/0103-507X.20140006
To assess the performance of the Nursing Activities Score in a pediatric intensive care unit, compare its scores expressed as time spent on nursing activities to the corresponding ones calculated using the Simplified Therapeutic Intervention Scoring System, and correlate the results obtained by both instruments with severity, morbidity and mortality.
Prospective, observational, and analytical cohort study conducted at a type III general pediatric intensive care unit. The study participants were all the children aged 29 days to 12 years admitted to the investigated pediatric intensive care unit from August 2008 to February 2009.
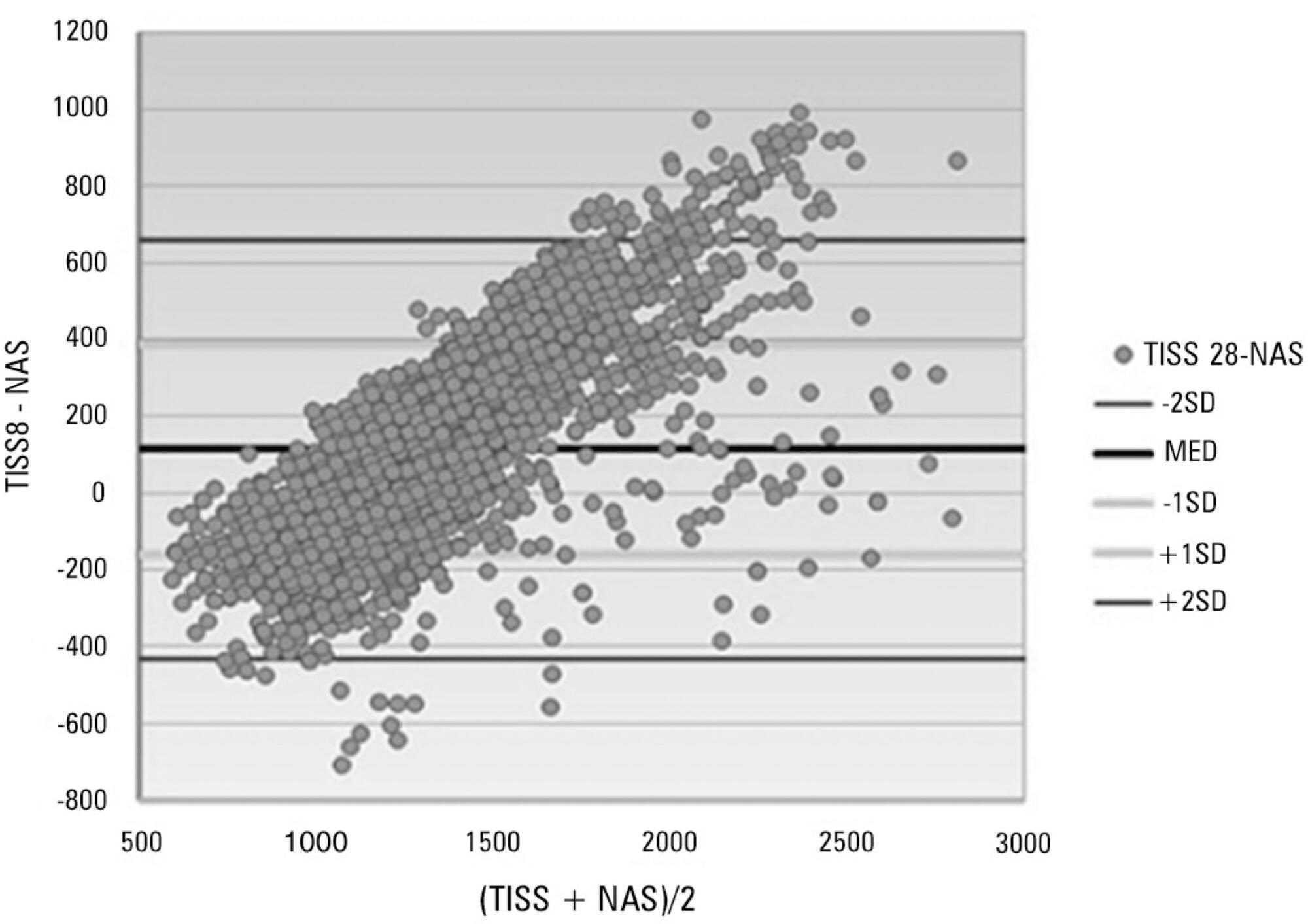
A total of 545 patients were studied, which corresponded to 2,951 assessments. The average score of the Simplified Therapeutic Intervention Scoring System was 28.79±10.37 (915±330 minutes), and that of the Nursing Activities Score was 55.6±11.82 (802±161 minutes). The number of minutes that resulted from the conversion of the Simplified Therapeutic Intervention Scoring System score was higher compared to that resulting from the Nursing Activities Score for all the assessments (p<0.001). The correlation between the instruments was significant, direct, positive, and moderate (R=0.564).
The agreement between the investigated instruments was satisfactory, and both instruments also exhibited satisfactory discrimination of mortality; for that purpose, the best cutoff point was 16 nursing hours/patient day.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):44-50
DOI 10.5935/0103-507X.20140007
To assess the discrimination and calibration of the Pediatric Index of Mortality 2 in patients admitted to a pediatric intensive care unit.
The study was conducted with a contemporary cohort from November 2005 to November 2006. Patients aged 29 days to 18 years were included in the study. Patients who died within 12 hours of admission and cases of readmission were excluded from the study. The performance of the Pediatric Index of Mortality 2 was assessed by means of the Hosmer-Lemeshow goodness-of-fit test, the standardized mortality ratio and the area under receiver operating characteristic (ROC) curve with 95% confidence interval. The significance level was established as 5%.
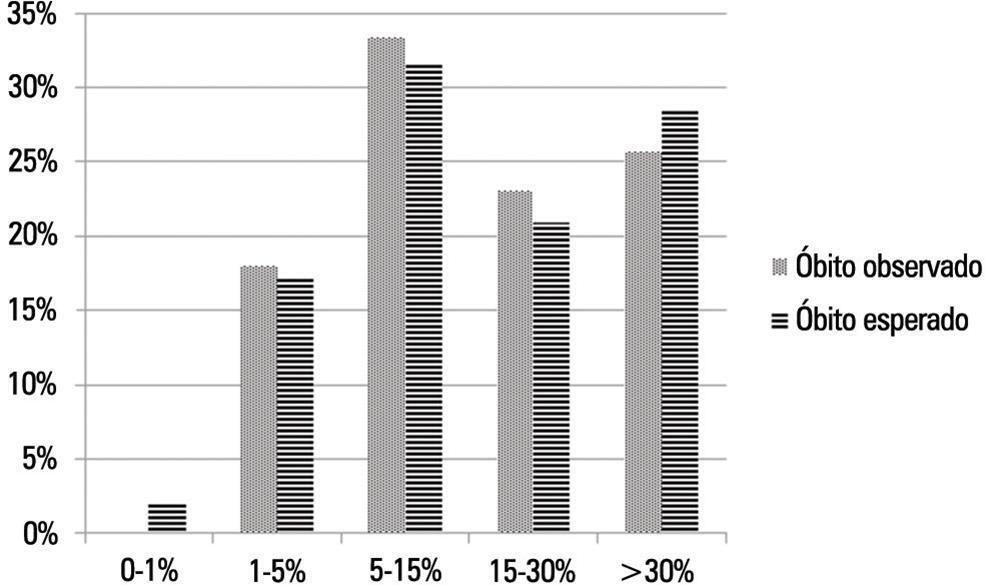
A total of 276 admissions to the pediatric intensive care unit were included in the analysis. The mortality rate was 14.13%, and the efficiency of admission 0.88%. The median age of the sample was 42.22 months, and most participants were male (60.1%). Most admissions were referrals from the emergency department. The mean duration of stay in pediatric intensive care unit was 6.43±5.23 days. Approximately 72.46% of admissions were for clinical reasons and exhibited an association with the outcome death (odds ratio: 2.9; 95%CI: 1.09-7.74; p=0.017). Calibration of the Pediatric Index of Mortality 2 with the chi-square statistic was 12.2686 (p=0.1396) in the Hosmer-Lemeshow goodness-of-fit test, and the standardized mortality ratio was 1.0. The area under the ROC curve assessing model discrimination was 0.778.
Pediatric Index of Mortality 2 exhibited satisfactory performance.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):51-56
DOI 10.5935/0103-507X.20140008
To identify risk factors for extubation failure and reintubation in newborn infants subjected to mechanical ventilation and to establish whether ventilation parameters and blood gas analysis behave as predictors of those outcomes.
Prospective study conducted at a neonatal intensive care unit from May to November 2011. A total of 176 infants of both genders subjected to mechanical ventilation were assessed after extubation. Extubation failure was defined as the need to resume mechanical ventilation within less than 72 hours. Reintubation was defined as the need to reintubate the infants any time after the first 72 hours.
Based on the univariate analysis, the variables gestational age <28 weeks, birth weight <1,000g and low Apgar scores were associated with extubation failure and reintubation. Based on the multivariate analysis, the variables length of mechanical ventilation (days), potential of hydrogen (pH) and partial pressure of oxygen (pO2) remained associated with extubation failure, and the five-minute Apgar score and age at extubation were associated with reintubation.
Low five-minute Apgar scores, age at extubation, length of mechanical ventilation, acid-base disorders and hyperoxia exhibited associations with the investigated outcomes of extubation failure and reintubation.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):57-64
DOI 10.5935/0103-507X.20140009
To describe the characteristics of physical therapy assistance to newborns and to provide a profile of physical therapists working in intensive care units in the city of São Paulo, Brazil.
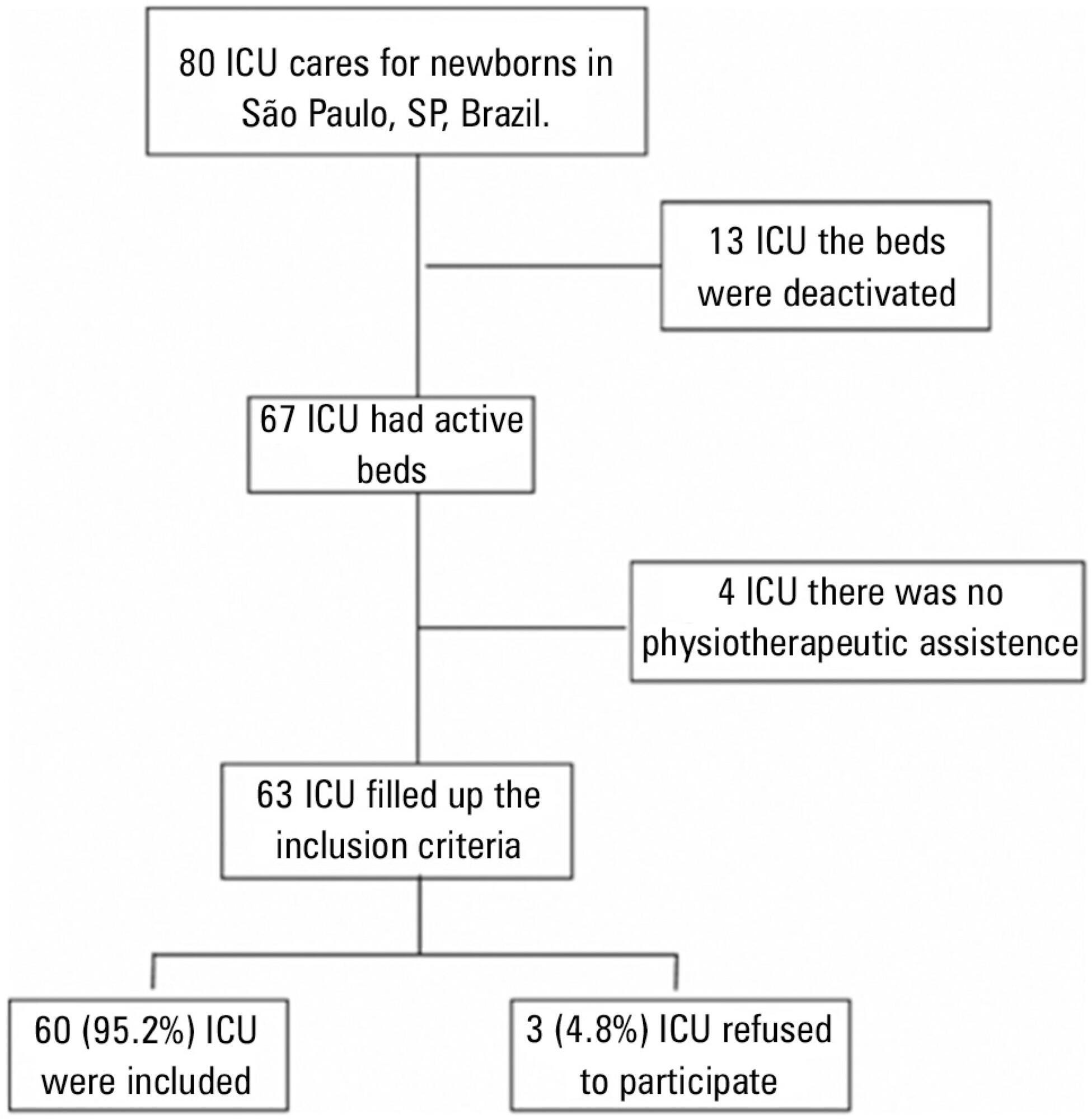
This cross-sectional study was conducted in every hospital in São Paulo city that had at least one intensive care unit bed for newborns registered at the National Registry of Health Establishments in 2010. In each unit, three types of physical therapists were included: an executive who was responsible for the physical therapy service in that hospital (chief-physical therapists), a physical therapist who was responsible for the physical therapy assistance in the neonatal unit (reference-physical therapists), and a randomly selected physical therapist who was directly involved in the neonatal care (care-physical therapists).
Among the 67 hospitals eligible for the study, 63 (94.0%) had a physical therapy service. Of those hospitals, three (4.8%) refused to participate. Thus, 60 chief-PTs, 52 reference-physical therapists, and 44 care-physical therapists were interviewed. During day shifts, night shifts, and weekends/holidays, there were no physical therapists in 1.7%, 45.0%, and 13.3% of the intensive care units, respectively. Physical therapy assistance was available for 17.8±7.2 hours/day, and each physical therapist cared for 9.4±2.6 newborns during six working hours. Most professionals had completed at least one specialization course.
Most neonatal intensive care units in the city of São Paulo had physical therapists working on the day shift. However, other shifts had incomplete staff with less than 18 hours of available physical therapy assistance per day.
Abstract
Rev Bras Ter Intensiva. 2014;26(1):65-70
DOI 10.5935/0103-507X.20140010
To evaluate the joint range of motion of critically ill patients during hospitalization in the intensive care unit.
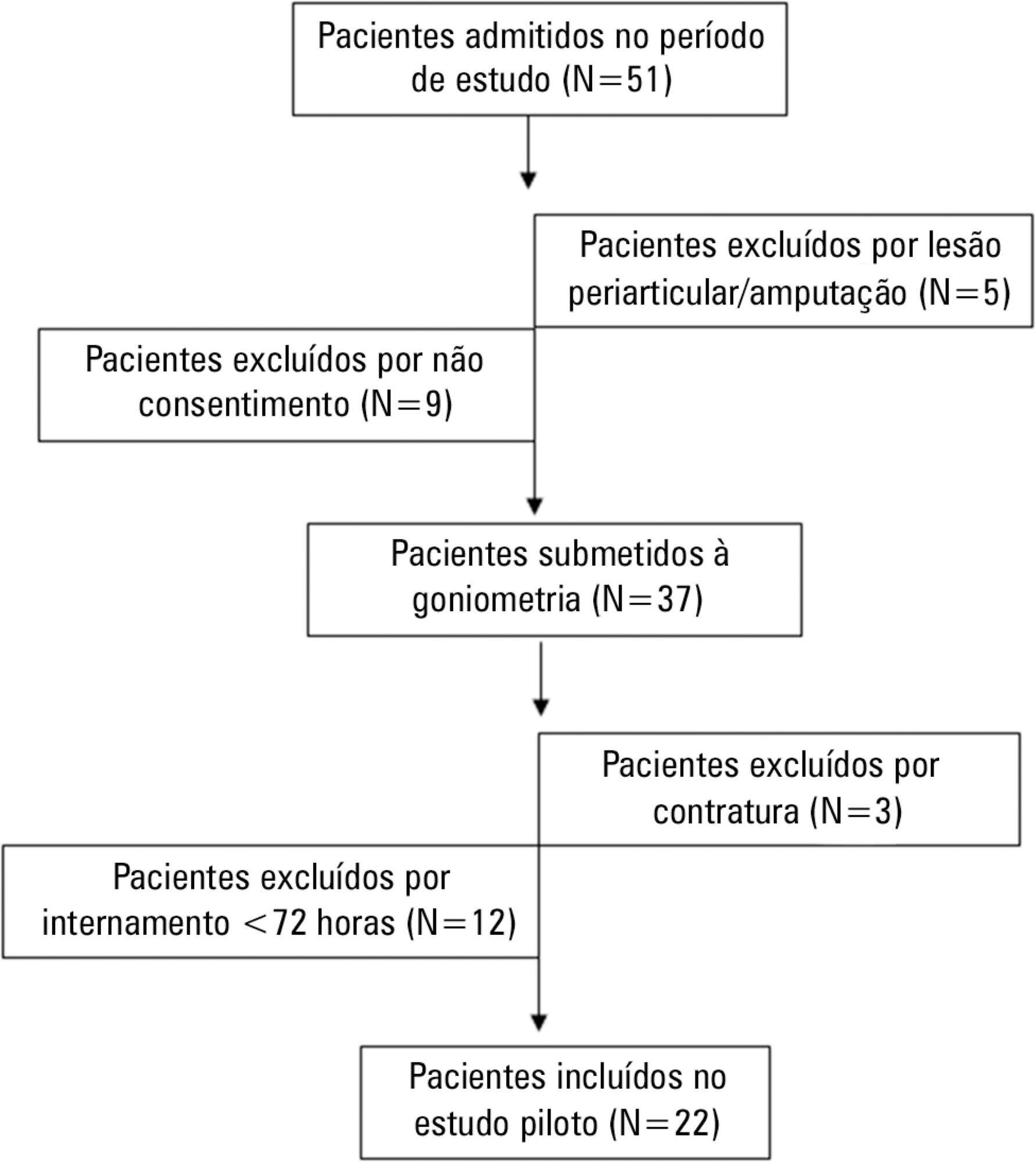
This work was a prospective longitudinal study conducted in a critical care unit of a public hospital in the city of Salvador (BA) from September to November 2010. The main variable evaluated was the passive joint range of motion. A goniometer was used to measure the elbows, knees and ankles at the time of admission and at discharge. All patients admitted in the period were included other than patients with length of stay <72 hours and patients with reduced joint range of motion on admission.
The sample consisted of 22 subjects with a mean age of 53.5±17.6 years, duration of stay in the intensive care unit of 13.0±6.0 days and time on mechanical ventilation of 12.0±6.3 days. The APACHE II score was 28.5±7.3, and the majority of patients had functional independence at admission with a prior Barthel index of 88.8±19. The losses of joint range of motion were 11.1±2.1°, 11.0±2.2°, 8.4±1.7°, 9.2±1.6°, 5.8±0.9° and 5.1±1.0°, for the right and left elbows, knees and ankles, respectively (p<0.001).
There was a tendency towards decreased range of motion of large joints such as the ankle, knee and elbow during hospitalization in the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):339-346
DOI 10.5935/0103-507X.20140052
This study aimed to determine which visitation policy was the most predominant in Brazilian intensive care units and what amenities were provided to visitors.
Eight hundred invitations were sent to the e-mail addresses of intensivist physicians and nurses who were listed in the research groups of the Brazilian Association of Intensive Care Network and the Brazilian Research in Intensive Care Network. The e-mail contained a link to a 33-item questionnaire about the profile of their intensive care unit.
One hundred sixty-two questionnaires from intensive care units located in all regions of the country, but predominantly in the Southeast and South (58% and 16%), were included in the study. Only 2.6% of the intensive care units reported having liberal visitation policies, while 45.1% of the intensive care units allowed 2 visitation periods and 69.1% allowed 31-60 minutes of visitation per period. In special situations, such as end-of-life cases, 98.7% of them allowed flexible visitation. About half of them (50.8%) did not offer any bedside amenities for visitors. Only 46.9% of the intensive care units had a family meeting room, and 37% did not have a waiting room.
Restrictive visitation policies are predominant in Brazilian intensive care units, with most of them allowing just two periods of visitation per day. There is also a lack of amenities for visitors.