Abstract
Rev Bras Ter Intensiva. 2014;26(4):347-354
DOI 10.5935/0103-507X.20140053
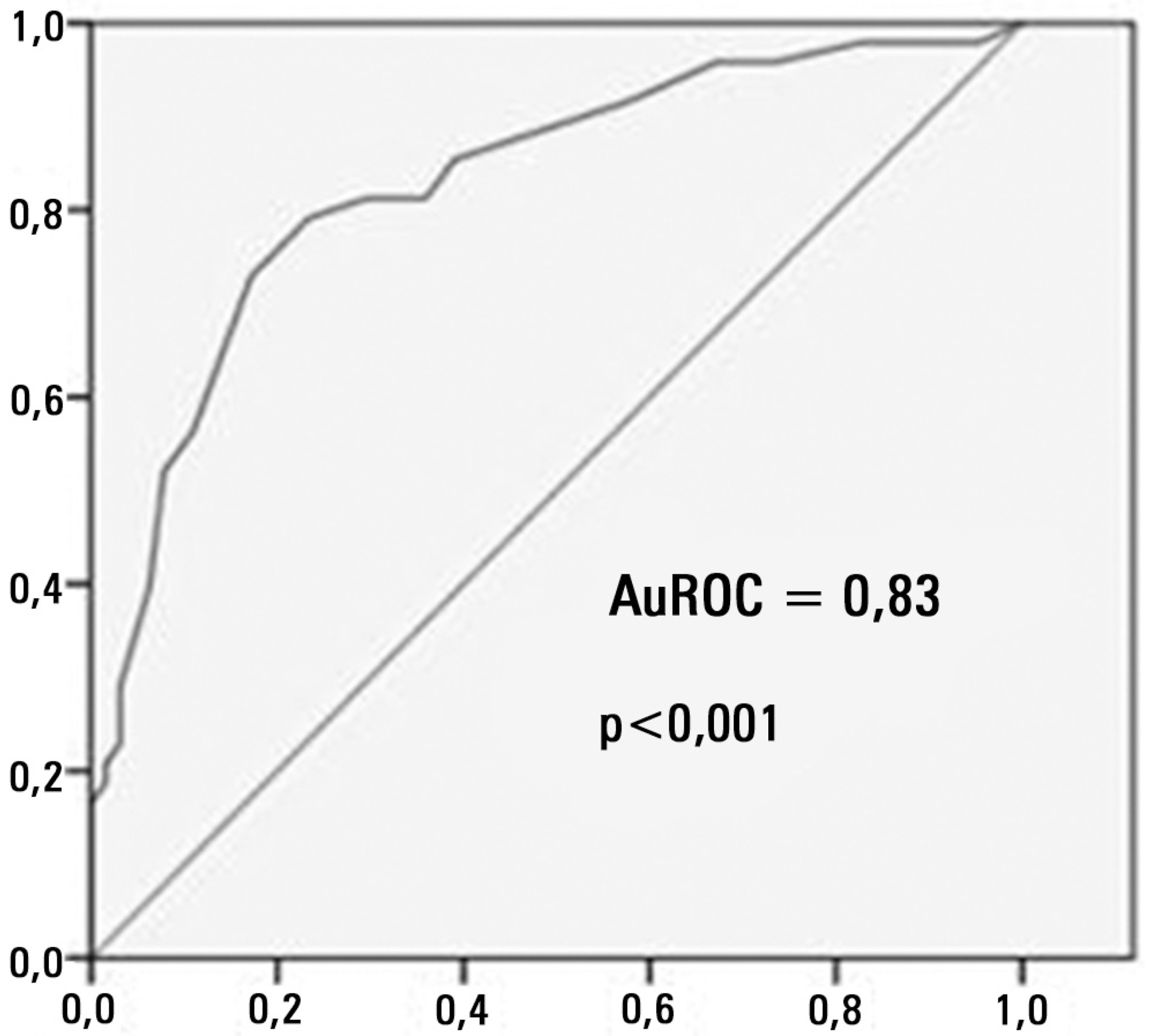
To assess the diagnostic and prognostic efficacy of urine neutrophil gelatinase-associated lipocalin in patients admitted to an intensive care unit.
Longitudinal, prospective cohort study conducted in a cardiology intensive care unit. The participants were divided into groups with and without acute kidney injury and were followed from admission to the intensive care unit until hospital discharge or death. Serum creatinine, urine output and urine neutrophil gelatinase-associated lipocalin were measured 24 and 48 hours after admission.
A total of 83 patients admitted to the intensive care unit for clinical reasons were assessed, most being male (57.8%). The participants were divided into groups without acute kidney injury (N=18), with acute kidney injury (N=28) and with severe acute kidney injury (N=37). Chronic diseases, mechanical ventilation and renal replacement therapy were more common in the groups with acute kidney injury and severe acute kidney injury, and those groups exhibited longer intensive care unit stay and hospital stay and higher mortality. Serum creatinine did not change significantly in the group with acute kidney injury within the first 24 hours of admission to the intensive care unit, although, urine neutrophil gelatinase-associated lipocalin was high in the groups with acute kidney injury and severe acute kidney injury (p<0.001). Increased urine neutrophil gelatinase-associated lipocalin was associated with death.
An increase in urine neutrophil gelatinase-associated lipocalin precedes variations in serum creatinine in patients with acute kidney injury and may be associated with death.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):355-359
DOI 10.5935/0103-507X.20140054
To assess adherence to a ventilator care bundle in an intensive care unit and to determine the impact of adherence on the rates of ventilatorassociated pneumonia.
A total of 198 beds were assessed for 60 days using a checklist that consisted of the following items: bed head elevation to 30 to 45º; position of the humidifier filter; lack of fluid in the ventilator circuit; oral hygiene; cuff pressure; and physical therapy. Next, an educational lecture was delivered, and 235 beds were assessed for the following 60 days. Data were also collected on the incidence of ventilator-acquired pneumonia.
Adherence to the following ventilator care bundle items increased: bed head elevation from 18.7% to 34.5%; lack of fluid in the ventilator circuit from 55.6% to 72.8%; oral hygiene from 48.5% to 77.8%; and cuff pressure from 29.8% to 51.5%. The incidence of ventilator-associated pneumonia was statistically similar before and after intervention (p=0.389).
The educational intervention performed in this study increased the adherence to the ventilator care bundle, but the incidence of ventilator-associated pneumonia did not decrease in the small sample that was assessed.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):360-366
DOI 10.5935/0103-507X.20140055
In Brazil, there are no data on the preferences of intensivists regarding hemodynamic monitoring methods. The present study aimed to identify the methods used by national intensivists, the hemodynamic variables they consider important, the regional differences, the reasons for choosing a particular method, and the use of protocols and continued training.
National intensivists were invited to answer an electronic questionnaire during three intensive care events and later, through the Associação de Medicina Intensiva Brasileira portal, between March and October 2009. Demographic data and aspects related to the respondent preferences regarding hemodynamic monitoring were researched.
In total, 211 professionals answered the questionnaire. Private hospitals showed higher availability of resources for hemodynamic monitoring than did public institutions. The pulmonary artery catheter was considered the most trusted by 56.9% of the respondents, followed by echocardiograms, at 22.3%. Cardiac output was considered the most important variable. Other variables also considered relevant were mixed/central venous oxygen saturation, pulmonary artery occlusion pressure, and right ventricular end-diastolic volume. Echocardiography was the most used method (64.5%), followed by pulmonary artery catheter (49.3%). Only half of respondents used treatment protocols, and 25% worked in continuing education programs in hemodynamic monitoring.
Hemodynamic monitoring has a greater availability in intensive care units of private institutions in Brazil. Echocardiography was the most used monitoring method, but the pulmonary artery catheter remains the most reliable. The implementation of treatment protocols and continuing education programs in hemodynamic monitoring in Brazil is still insufficient.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):367-372
DOI 10.5935/0103-507X.20140056
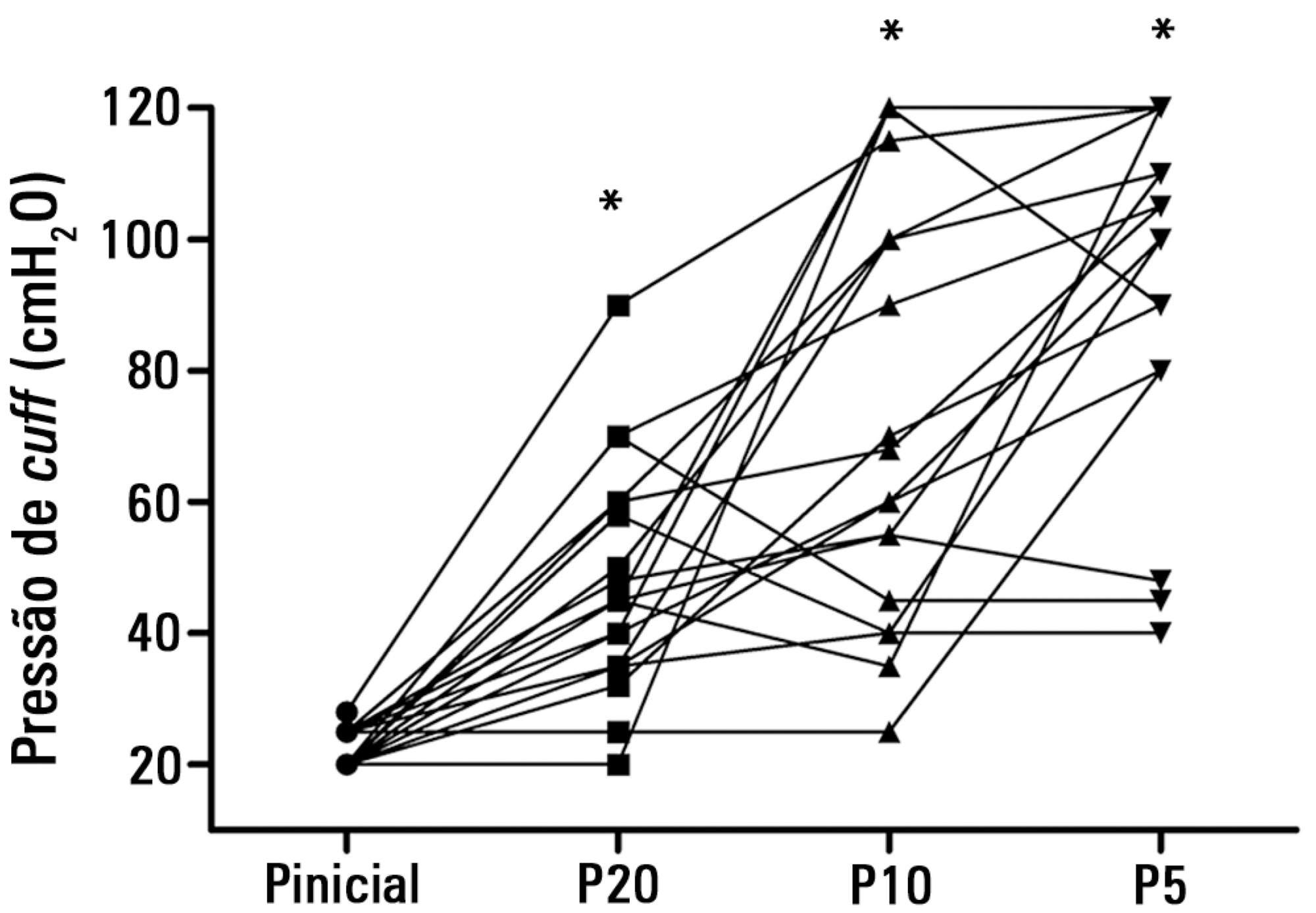
To test the effectiveness of using a cuff pressure relief valve technique to maintain cuff pressure levels within the normal in vitro range (Phase 1) in patients admitted to the intensive care unit (Phase 2) and to test the reproducibility of the technique using different syringes.
In Phase 1, a tracheal tube was inserted into a trachea model. Ten- and 20mL syringes were used to inflate the cuff through the tracheal tube. The cuff was slowly and steadily inflated until the syringe plunger would move in the opposite direction of the application. After the plunger stopped, the cuff pressures were recorded. In Phase 2, the same maneuvers for inflating the cuff were performed on 20 patients using 5, 10, and 20mL syringes and were compared with manometer measurements. The intraclass correlation coefficient and Bland-Altman analysis were employed to determine the reproducibility and agreement between syringes. Data were expressed as medians (interquartile range).
There was no reproducibility between syringes with an intraclass correlation coefficient ranging between -0.33 and 0.8 (p>0.05). The pressures generated with the syringes were higher than the pressures generated using a standard manometer: the 5mL syringe pressure was 105cmH2O (82.5-120cmH2O), the 10mL syringe pressure was 69cmH2O (47.5-111.3cmH2O), and the 20mL syringe pressure was 45cmH2O (35-59.5cmH2O). The Bland-Altman analysis confirmed the large bias and variability between the syringes used, compared with the manometer.
The use of syringes is not an effective technique for determining the cuff pressure in patients admitted to the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):373-378
DOI 10.5935/0103-507X.20140057
The objective of this study was to translate and culturally adapt the Behavioral Pain Scale to Brazilian Portuguese and to evaluate the psychometric properties of this scale.
This study was conducted in two phases: the Behavioral Pain Scale was translated and culturally adapted to Brazilian Portuguese and the psychometric properties of this scale were subsequently assessed (reliability and clinical utility). The study sample consisted of 100 patients who were older than 18 years of age, admitted to an intensive care unit, intubated, mechanically ventilated, and subjected or not to sedation and analgesia from July 2012 to December 2012. Pediatric and non-intubated patients were excluded. The study was conducted at a large private hospital that was situated in the city of São Paulo (SP).
Regarding reproducibility, the results revealed that the observed agreement between the two evaluators was 92.08% for the pain descriptor “adaptation to mechanical ventilation”, 88.1% for “upper limbs”, and 90.1% for “facial expression”. The kappa coefficient of agreement for “adaptation to mechanical ventilation” assumed a value of 0.740. Good agreement was observed between the evaluators with an intraclass correlation coefficient of 0.807 (95% confidence interval: 0.727-0.866).
The Behavioral Pain Scale was easy to administer and reproduce. Additionally, this scale had adequate internal consistency. The Behavioral Pain Scale was satisfactorily adapted to Brazilian Portuguese for the assessment of pain in critically ill patients.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):379-383
DOI 10.5935/0103-507X.20140058
To describe the oral health status of patients hospitalized in an intensive care unit.
Clinical assessment of the oral cavity was performed in 35 patients at two time-points (up to 48 hours after admission and 72 hours after the first assessment) and recorded in data collection forms. The following data were collected: plaque index, condition of the mucosa, presence or absence of dental prosthesis, number of teeth present, and tongue coating index.
The prevalence of nosocomial infection was 22% (eight patients), with 50% respiratory tract infections. All patients exhibited oral biofilm, and 20 (57%) showed biofilm visible to the naked eye; tongue coating was present on more than two thirds of the tongue in 24 patients (69%) and was thick in most cases. A significant increase in plaque index (p=0.007) occurred after 72 hours, although the tongue coating index was p<0.001 regarding the area and p=0.5 regarding the thickness.
The plaque and tongue coating indices increased with the length of hospital stay at the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):384-391
DOI 10.5935/0103-507X.20140059
This study aimed to describe and compare the characteristics and clinical outcomes of patients with septic and non-septic acute kidney injury.
This study evaluated an open cohort of 117 critically ill patients with acute kidney injury who were consecutively admitted to an intensive care unit, excluding patients with a history of advanced-stage chronic kidney disease, kidney transplantation, hospitalization or death in a period shorter than 24 hours. The presence of sepsis and in-hospital death were the exposure and primary variables in this study, respectively. A confounding analysis was performed using logistic regression.
No significant differences were found between the mean ages of the groups with septic and non-septic acute kidney injury [65.30±21.27 years versus 66.35±12.82 years, respectively; p=0.75]. In the septic and non-septic acute kidney injury groups, a predominance of females (57.4% versus 52.4%, respectively; p=0.49) and Afro-descendants (81.5% versus 76.2%, respectively; p=0.49) was observed. Compared with the non-septic patients, the patients with sepsis had a higher mean Acute Physiology and Chronic Health Evaluation II score [21.73±7.26 versus 15.75±5.98; p<0.001)] and a higher mean water balance (p=0.001). Arterial hypertension (p=0.01) and heart failure (p<0.001) were more common in the non-septic patients. Septic acute kidney injury was associated with a greater number of patients who required dialysis (p=0.001) and a greater number of deaths (p<0.001); however, renal function recovery was more common in this group (p=0.01). Sepsis (OR: 3.88; 95%CI: 1.51-10.00) and an Acute Physiology and Chronic Health Evaluation II score >18.5 (OR: 9.77; 95%CI: 3.73-25.58) were associated with death in the multivariate analysis.
Sepsis was an independent predictor of death. Significant differences were found between the characteristics and clinical outcomes of patients with septic versus non-septic acute kidney injury.
Abstract
Rev Bras Ter Intensiva. 2014;26(4):392-396
DOI 10.5935/0103-507X.20140060
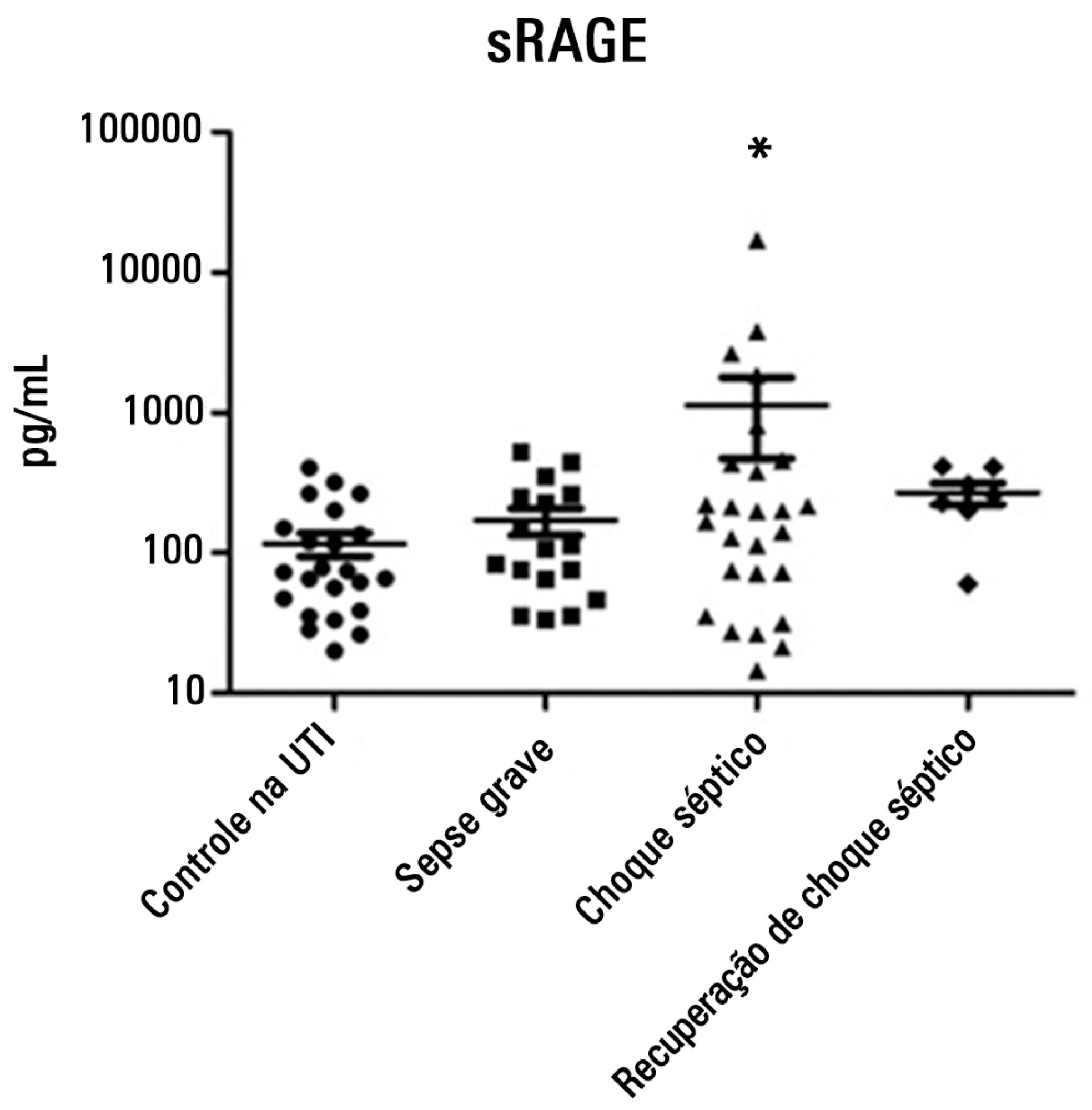
To evaluate and understand the clinical implications of the plasma levels of a soluble isoform of a receptor for advanced glycation end products (sRAGE) in different stages of sepsis.
Serum sRAGE values in patients who were divided into intensive care unit control, severe sepsis, septic shock and recovery from septic shock groups were statistically analyzed to assess quantity (Kruskal-Wallis), variability (Levine test) and correlation (Spearman rank test) with certain inflammatory mediators (IL-1 α, IL-6, IL-8, IL-10, IP-10, G-CSF, MCP-1, IFN-γ and TNF-α).
No changes in sRAGE levels were observed among the groups; however, the septic shock group showed differences in the variability of sRAGE compared to the other groups. A positive correlation with all the inflammatory mediators was reported in the septic shock group.
sRAGE levels are associated with worse outcomes in patients with septic shock. However, a statistical correlation analysis with other proinflammatory cytokines indicated that the pathways leading to those outcomes are different depending on the sRAGE levels. Future studies to elucidate the pathophysiological mechanisms involving sRAGE in models of sepsis are of great clinical importance for the safe handling of this biomarker.