Abstract
Rev Bras Ter Intensiva. 2013;25(3):188-196
DOI 10.5935/0103-507X.20130034
Deep sedation in critically ill patients is associated with a longer duration of mechanical ventilation and a prolonged length of stay in the intensive care unit. Several protocols have been used to improve these outcomes. We implement and evaluate an analgesia-based, goal-directed, nurse-driven sedation protocol used to treat critically ill patients who receive mechanical ventilation.
We performed a prospective, two-phase (before-after), non-randomized multicenter study that involved 13 intensive care units in Chile. After an observational phase (observational group, n=155), we designed, implemented and evaluated an analgesia-based, goal-directed, nurse-driven sedation protocol (intervention group, n=132) to treat patients who required mechanical ventilation for more than 48 hours. The primary outcome was to achieve ventilator-free days by day 28.
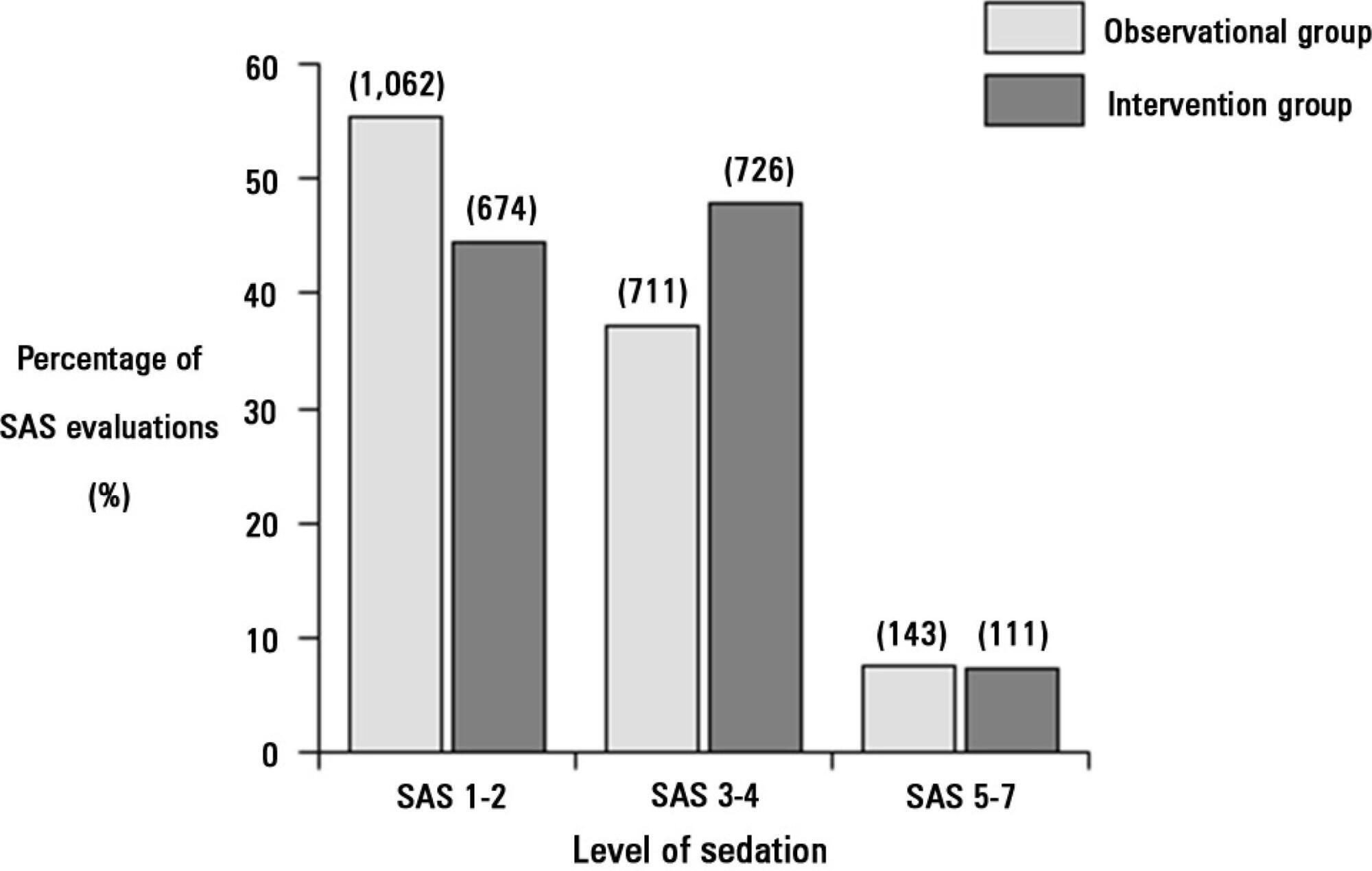
The proportion of patients in deep sedation or in a coma decreased from 55.2% to 44.0% in the interventional group. Agitation did not change between the periods and remained approximately 7%. Ventilator-free days to day 28, length of stay in the intensive care unit and mortality were similar in both groups. At one year, post-traumatic stress disorder symptoms in survivors were similar in both groups.
We designed and implemented an analgesia-based, goal-directed, nurse-driven sedation protocol in Chile. Although there was no improvement in major outcomes, we observed that the present protocol was safe and feasible and that it resulted in decreased periods of deep sedation without increasing agitation.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):205-211
DOI 10.5935/0103-507X.20130036
Corrected anion gap and strong ion gap are commonly used to estimate unmeasured anions. We evaluated the performance of the anion gap corrected for albumin, phosphate and lactate in predicting strong ion gap in a mixed population of critically ill patients. We hypothesized that anion gap corrected for albumin, phosphate and lactate would be a good predictor of strong ion gap, independent of the presence of metabolic acidosis. In addition, we evaluated the impact of strong ion gap at admission on hospital mortality.
We included 84 critically ill patients. Correlation and agreement between the anion gap corrected for albumin, phosphate and lactate and strong ion gap was evaluated by the Pearson correlation test, linear regression, a Bland-Altman plot and calculating interclass correlation coefficient. Two subgroup analyses were performed: one in patients with base-excess <-2mEq/L (low BE group - lBE) and the other in patients with base-excess >-2mEq/L (high BE group - hBE). A logistic regression was performed to evaluate the association between admission strong ion gap levels and hospital mortality.
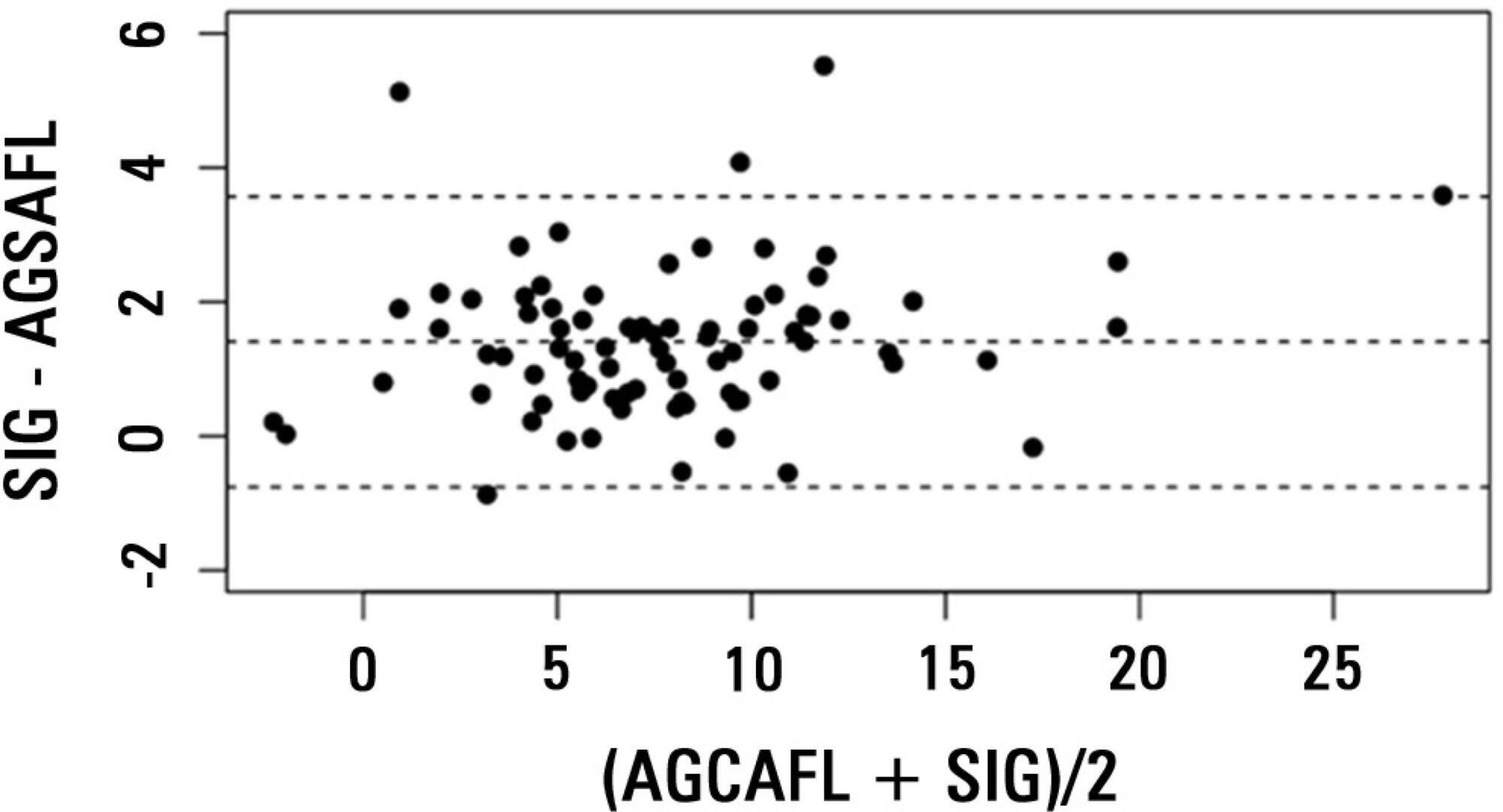
There was a very strong correlation and a good agreement between anion gap corrected for albumin, phosphate and lactate and strong ion gap in the general population (r2=0.94; bias 1.40; limits of agreement -0.75 to 3.57). Correlation was also high in the lBE group (r2=0.94) and in the hBE group (r2=0.92). High levels of strong ion gap were present in 66% of the whole population and 42% of the cases in the hBE group. Strong ion gap was not associated with hospital mortality by logistic regression.
Anion gap corrected for albumin, phosphate and lactate and strong ion gap have an excellent correlation. Unmeasured anions are frequently elevated in critically ill patients with normal base-excess. However, there was no association between unmeasured anions and hospital mortality.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):212-217
DOI 10.5935/0103-507X.20130037
To investigate the association between the rapid shallow breathing index and successful extubation in patients with traumatic brain injury.
This study was a prospective study conducted in patients with traumatic brain injury of both genders who underwent mechanical ventilation for at least two days and who passed a spontaneous breathing trial. The minute volume and respiratory rate were measured using a ventilometer, and the data were used to calculate the rapid shallow breathing index (respiratory rate/tidal volume). The dependent variable was the extubation outcome: reintubation after up to 48 hours (extubation failure) or not (extubation success). The independent variable was the rapid shallow breathing index measured after a successful spontaneous breathing trial.
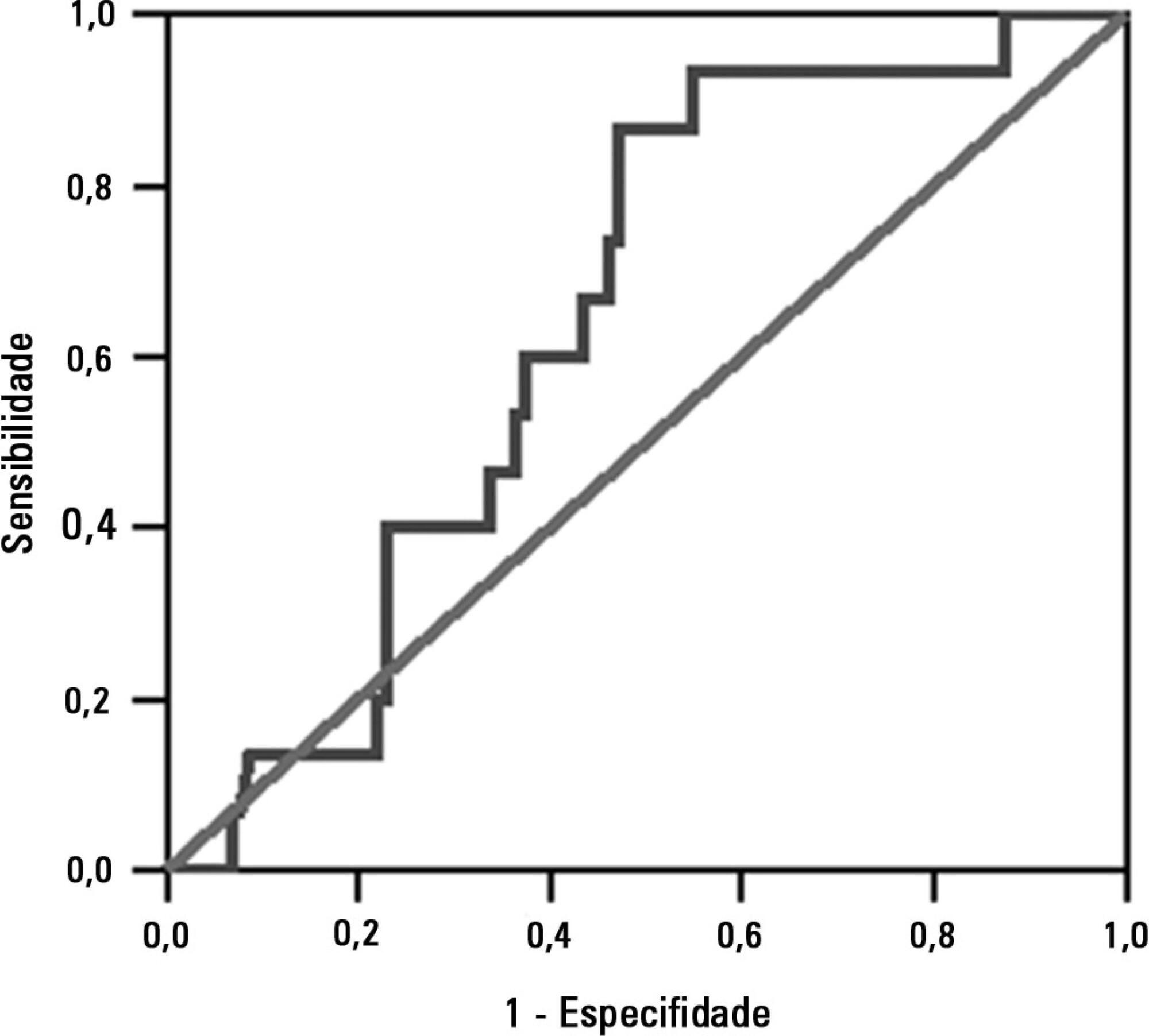
The sample comprised 119 individuals, including 111 (93.3%) males. The average age of the sample was 35.0±12.9 years old. The average duration of mechanical ventilation was 8.1±3.6 days. A total of 104 (87.4%) participants achieved successful extubation. No association was found between the rapid shallow breathing index and extubation success.
The rapid shallow breathing index was not associated with successful extubation in patients with traumatic brain injury.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):218-224
DOI 10.5935/0103-507X.20130038
To assess the functional and psychological features of patients immediately after discharge from the intensive care unit.
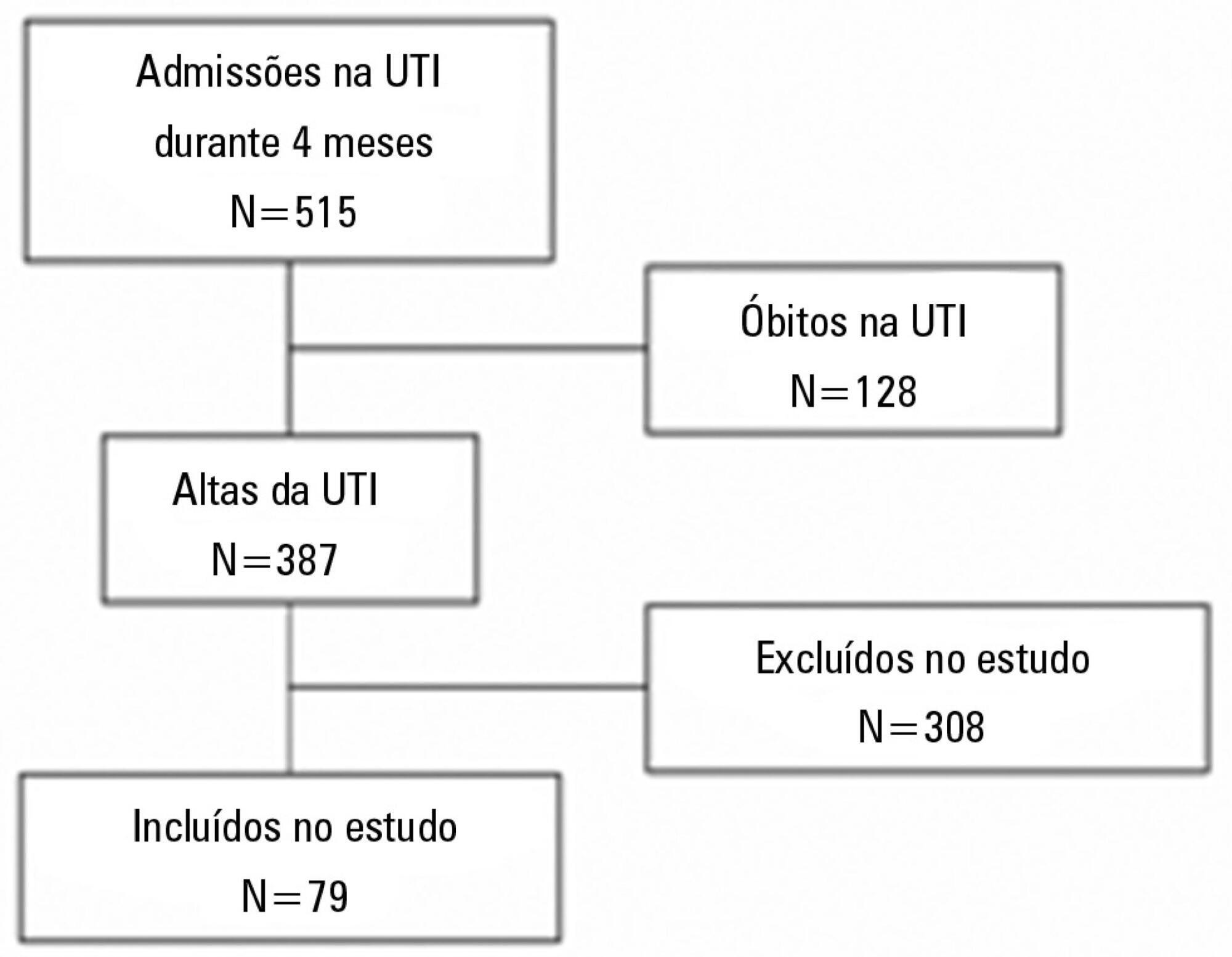
Prospective cohort study. Questionnaires and scales assessing the degree of dependence and functional capacity (modified Barthel and Karnofsky scales) and psychological problems (Hospital Anxiety and Depression Scale), in addition to the Epworth Sleepiness Scale, were administered during interviews conducted over the first week after intensive care unit discharge, to all survivors who had been admitted to this service from August to November 2012 and had remained longer than 72 hours.
The degree of dependence as measured by the modified Barthel scale increased after intensive care unit discharge compared with the data before admission (57±30 versus 47±36; p<0.001) in all 79 participants. This impairment was homogeneous among all the categories in the modified Barthel scale (p<0.001) in the 64 participants who were independent or partially dependent (Karnofsky score ≥40) before admission. The impairment affected the categories of personal hygiene (p=0.01) and stair climbing (p=0.04) only in the 15 participants who were highly dependent (Karnofsky score <40) before admission. Assessment of the psychological changes identified mood disorders (anxiety and/or depression) in 31% of the sample, whereas sleep disorders occurred in 43.3%.
Patients who remained in an intensive care unit for 72 hours or longer exhibited a reduced functional capacity and an increased degree of dependence during the first week after intensive care unit discharge. In addition, the incidence of depressive symptoms, anxiety, and sleep disorders was high among that population.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):225-232
DOI 10.5935/0103-507X.20130039
This study sought to compare patients at public and private intensive care units according to the nursing workload and interventions provided.
This retrospective, comparative cohort study included 600 patients admitted to 4 intensive care units in São Paulo. The nursing workload and interventions were assessed using the Nursing Activities Score during the first and last 24 hours of the patient's stay at the intensive care unit. Pearson's chi-square test, Fisher's exact test, the Mann-Whitney test, and Student's t test were used to compare the patient groups.
The average Nursing Activities Score upon admission to the intensive care unit was 61.9, with a score of 52.8 upon discharge. Significant differences were found among the patients at public and private intensive care units relative to the average Nursing Activities Score upon admission, as well as for 12 out of 23 nursing interventions performed during the first 24 hours of stay at the intensive care units. The patients at the public intensive care units exhibited a higher average score and overall more frequent nursing interventions, with the exception of those involved in the "care of drains", "mobilization and positioning", and "intravenous hyperalimentation". The groups also differed with regard to the evolution of the Nursing Activities Score among the total case series as well as the groups of survivors from the time of admission to discharge from the intensive care unit.
Patients admitted to public and private intensive care units exhibit differences in their nursing care demands, which may help managers with nursing manpower planning.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):233-238
DOI 10.5935/0103-507X.20130040
The objective of this study was to assess the correlation between the European System for Cardiac Operative Risk Evaluation (EuroSCORE) score and the risk of developing acute kidney injury in cardiac surgery patients.
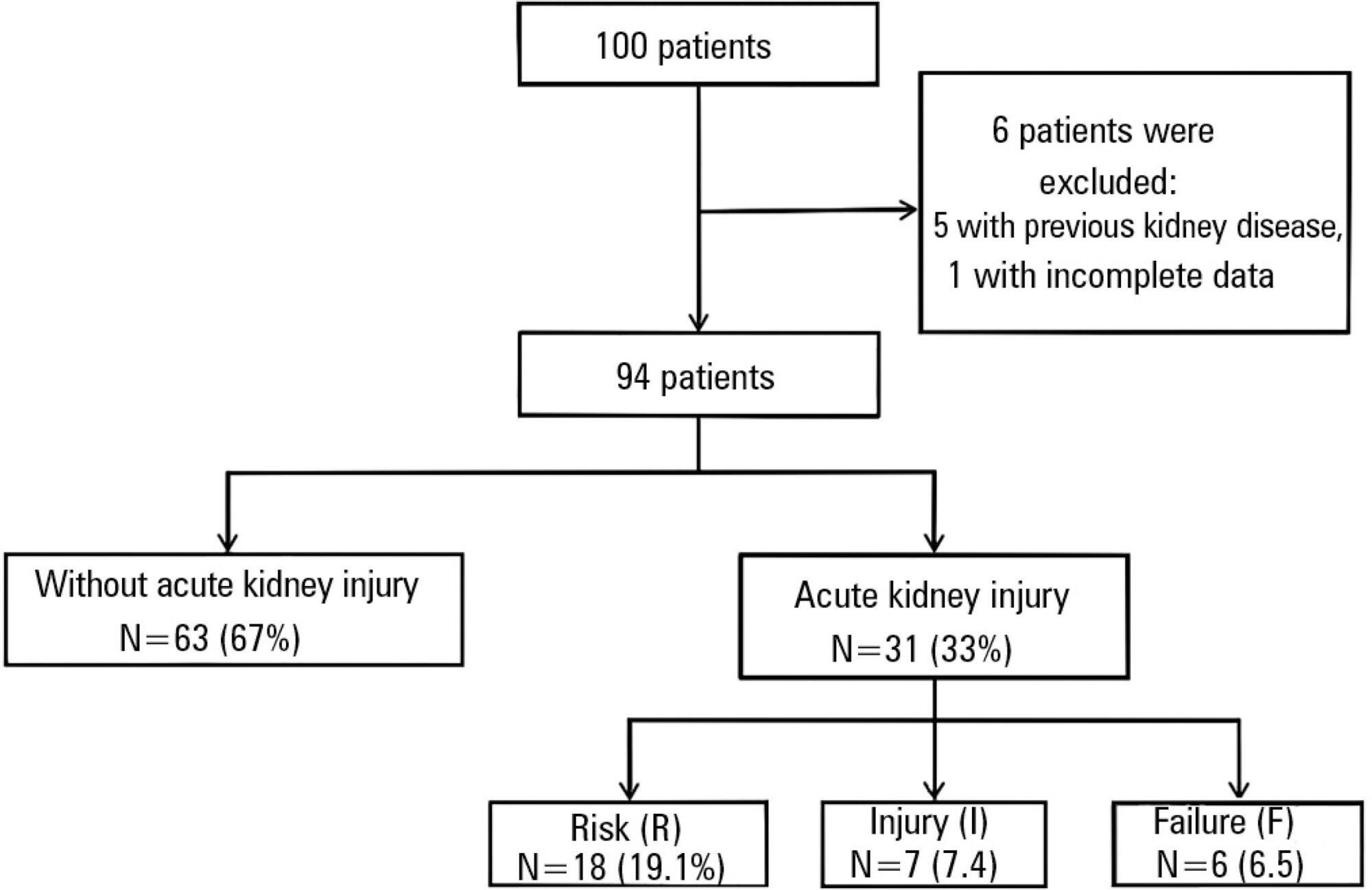
This retrospective study was conducted at a tertiary hospital on consecutive cardiac surgery patients (e.g., valvular, ischemic and congenital heart diseases) between October 2010 and July 2011.
One hundred patients were assessed. Among the 100 patients, six were excluded, including five because of prior kidney disease or dialysis therapy and one because of incomplete medical records. The primary surgical indications were myocardial revascularization in 55 patients (58.5% of cases) and valve replacement in 28 patients (29.8%). According to the EuroSCORE, 55 patients were classified as high risk (58.5%), 27 patients as medium risk (28.7%) and 12 patients as low risk (12.8%). In the postoperative period, patients were classified with the Risk, Injury, Failure, Loss and End-stage kidney disease (RIFLE) score. Among the 31 patients (33%) who displayed an increase in serum creatinine, 18 patients (19.1%) were classified as RIFLE "R" (risk), seven patients (7.4%) were classified as RIFLE "I" (injury) and six patients (6.5%) were classified as RIFLE "F" (failure). Among the patients who were considered to be high risk according to the EuroSCORE criteria, 24 patients (43.6%) showed acute kidney injury. Among the patients who were classified as medium or low risk, acute kidney injury occurred in 18.5 and 16.6% of the cases, respectively. The correlations between risk stratification (low, medium and high) and the EuroSCORE and postoperative RIFLE scores were statistically significant (p=0.03).
In the studied population, there was a statistically significant correlation between the EuroSCORE and the risk of developing acute kidney injury in the postoperative period after cardiac surgery.
Abstract
Rev Bras Ter Intensiva. 2013;25(3):239-244
DOI 10.5935/0103-507X.20130041
This study sought to evaluate infections related to health care caused by coagulase-negative Staphylococci in a neonatal intensive care unit by assessing antimicrobial susceptibility profiles and potentially effective antibiotic regimens.
This was a retrospective descriptive study performed on a case series of healthcare-associated infections, and the antimicrobial susceptibility profiles were evaluated. Newborns from other hospitals who were admitted to a neonatal intensive care unit in Rio de Janeiro between January 1, 2010, and June 30, 2012, were studied.
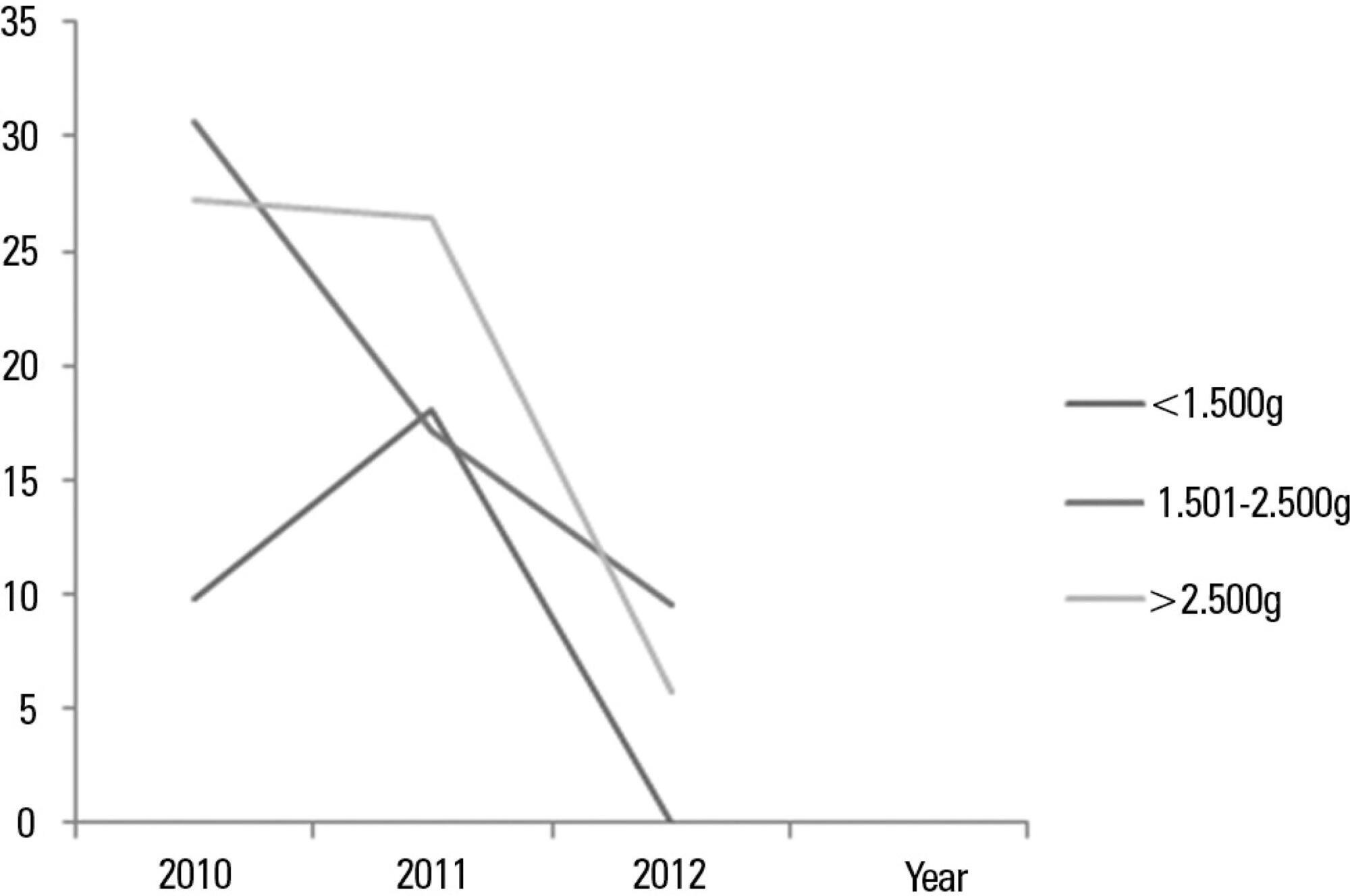
In total, 765 patients were admitted, totaling 3,051 patient-days, and the incidence density of general infection was 18.9 per 1,000 patient-days. The rate of central venous catheter use was 71.6%, and the positive culture rate for all sites and all infections related to health care were 68.4%. Coagulase-negative Staphylococci were identified in 11 (19.2%) of 57 health care-related infections, and infections with extended-spectrum beta-lactamase producing Klebsiella pneumoniae and Candida sp. constituted 5 cases each. Of the 11 cases of coagulase-negative Staphylococci, 10 (90.9%) were primary bloodstream infections. The sensitivity of the coagulase-negative Staphylococci isolates to vancomycin, clindamycin, ciprofloxacin, oxacillin and gentamycin was 100%, 81.8%, 72.7%, 27.2% and 22.2%, respectively. There were no deaths directly attributed to coagulase-negative Staphylococci infection.
Coagulase-negative Staphylococci was the main agent identified in healthcare-associated infections, with low rates of infections related to central venous catheter. In hospitals with a high oxacillin resistance profile, similar to those included in this study, vancomycin may be used as an initial therapy, although clindamycin represents a viable alternative.