Abstract
Rev Bras Ter Intensiva. 2015;27(3):247-251
DOI 10.5935/0103-507X.20150045
To evaluate the incidence of urinary tract infections due to Trichosporon spp. in an intensive care unit.
This descriptive observational study was conducted in an intensive care unit between 2007 and 2009. All consecutive patients admitted to the intensive care unit with a confirmed diagnosis were evaluated.
Twenty patients presented with urinary tract infections due to Trichosporon spp. The prevalence was higher among men (65%) and among individuals > 70 years of age (55%). The mortality rate was 20%. The average intensive care unit stay was 19.8 days. The onset of infection was associated with prior use of antibiotics and was more frequent in the fall and winter.
Infection due to Trichosporon spp. was more common in men and among those > 70 years of age and was associated with the use of an indwelling urinary catheter for more than 20 days and with the use of broadspectrum antibiotics for more than 14 days. In addition, patients with urinary infection due to Trichosporon spp. were most often hospitalized in intensive care units in the fall and winter periods.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):252-259
DOI 10.5935/0103-507X.20150046
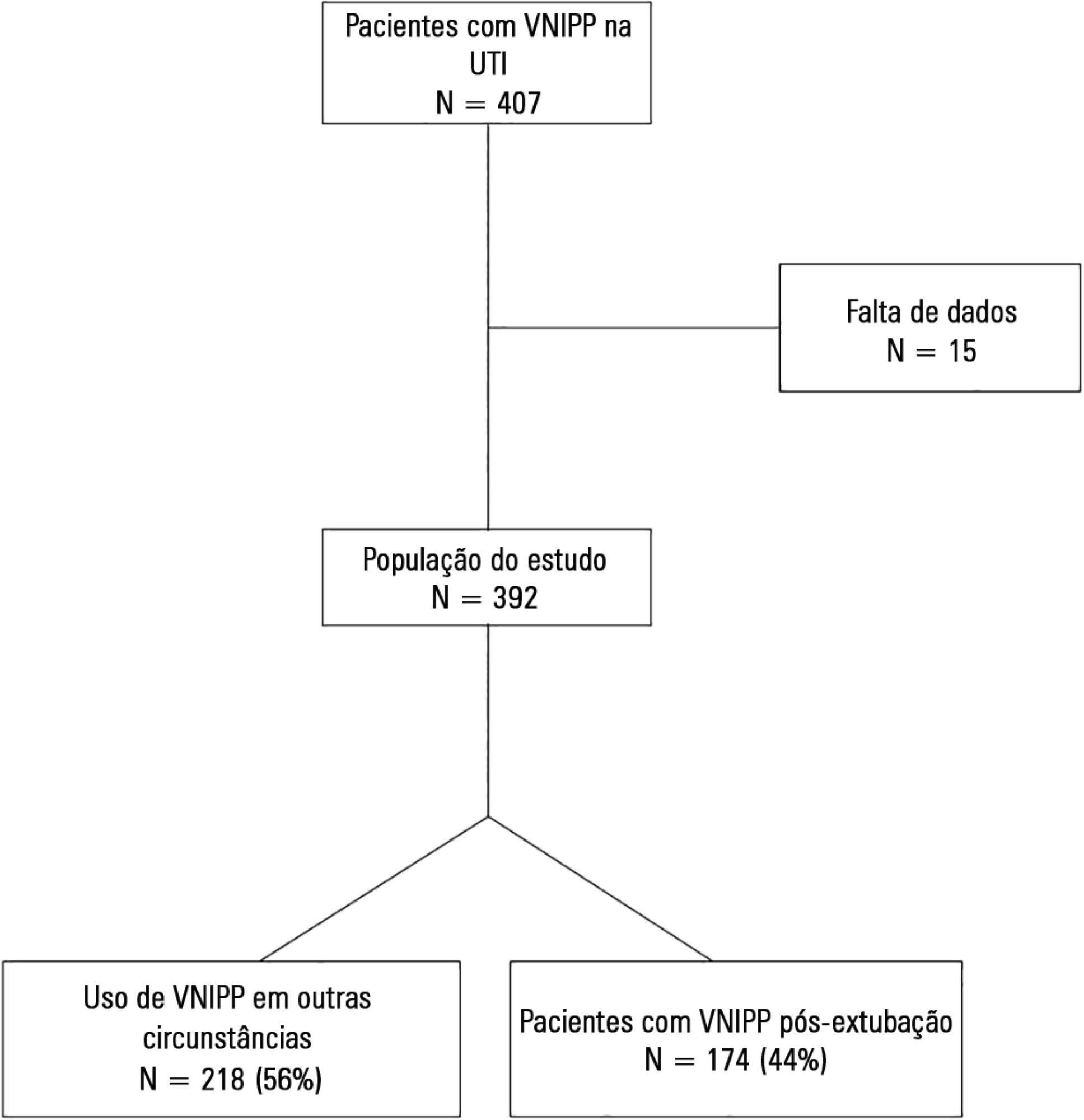
To describe postextubation noninvasive positive pressure ventilation use in intensive care unit clinical practice and to identify factors associated with noninvasive positive pressure ventilation failure.
This prospective cohort study included patients aged ≥ 18 years consecutively admitted to the intensive care unit who required noninvasive positive pressure ventilation within 48 hours of extubation. The primary outcome was noninvasive positive pressure ventilation failure.
We included 174 patients in the study. The overall noninvasive positive pressure ventilation use rate was 15%. Among the patients who used noninvasive positive pressure ventilation, 44% used it after extubation. The failure rate of noninvasive positive pressure ventilation was 34%. The overall mean ± SD age was 56 ± 18 years, and 55% of participants were male. Demographics; baseline pH, PaCO2 and HCO3; and type of equipment used were similar between groups. All of the noninvasive positive pressure ventilation final parameters were higher in the noninvasive positive pressure ventilation failure group [inspiratory positive airway pressure: 15.0 versus 13.7cmH2O (p = 0.015), expiratory positive airway pressure: 10.0 versus 8.9cmH2O (p = 0.027), and FiO2: 41 versus 33% (p = 0.014)]. The mean intensive care unit length of stay was longer (24 versus 13 days), p < 0.001, and the intensive care unit mortality rate was higher (55 versus 10%), p < 0.001 in the noninvasive positive pressure ventilation failure group. After fitting, the logistic regression model allowed us to state that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure compared with individuals with inspiratory positive airway pressure < 13.5 (OR = 3.02, 95%CI = 1.01 - 10.52, p value = 0.040).
The noninvasive positive pressure ventilation failure group had a longer intensive care unit length of stay and a higher mortality rate. Logistic regression analysis identified that patients with inspiratory positive airway pressure ≥ 13.5cmH2O on the last day of noninvasive positive pressure ventilation support are three times more likely to experience noninvasive positive pressure ventilation failure.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):260-265
DOI 10.5935/0103-507X.20150047
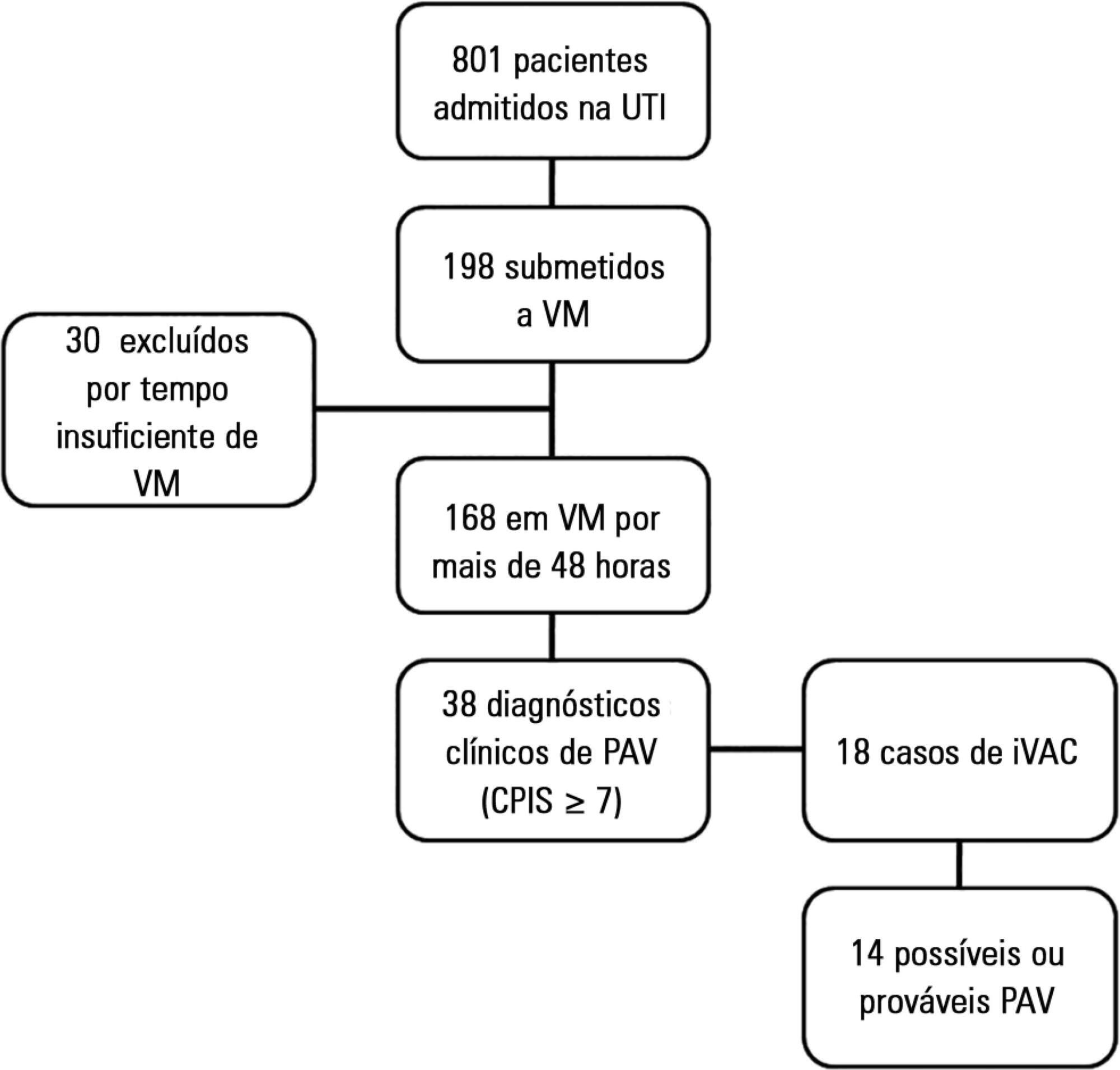
>To evaluate the agreement between a new epidemiological surveillance method of the Center for Disease Control and Prevention and the clinical pulmonary infection score for mechanical ventilator-associated pneumonia detection.
This was a prospective cohort study that evaluated patients in the intensive care units of two hospitals who were intubated for more than 48 hours between August 2013 and June 2014. Patients were evaluated daily by physical therapist using the clinical pulmonary infection score. A nurse independently applied the new surveillance method proposed by the Center for Disease Control and Prevention. The diagnostic agreement between the methods was evaluated. A clinical pulmonary infection score of ≥ 7 indicated a clinical diagnosis of mechanical ventilator-associated pneumonia, and the association of a clinical pulmonary infection score ≥ 7 with an isolated semiquantitative culture consisting of ≥ 104 colony-forming units indicated a definitive diagnosis.
Of the 801 patients admitted to the intensive care units, 198 required mechanical ventilation. Of these, 168 were intubated for more than 48 hours. A total of 18 (10.7%) cases of mechanical ventilation-associated infectious conditions were identified, 14 (8.3%) of which exhibited possible or probable mechanical ventilatorassociated pneumonia, which represented 35% (14/38) of mechanical ventilator-associated pneumonia cases. The Center for Disease Control and Prevention method identified cases of mechanical ventilator-associated pneumonia with a sensitivity of 0.37, specificity of 1.0, positive predictive value of 1.0, and negative predictive value of 0.84. The differences resulted in discrepancies in the mechanical ventilator-associated pneumonia incidence density (CDC, 5.2/1000 days of mechanical ventilation; clinical pulmonary infection score ≥ 7, 13.1/1000 days of mechanical ventilation).
The Center for Disease Control and Prevention method failed to detect mechanical ventilatorassociated pneumonia cases and may not be satisfactory as a surveillance method.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):205-211
DOI 10.5935/0103-507X.20150042
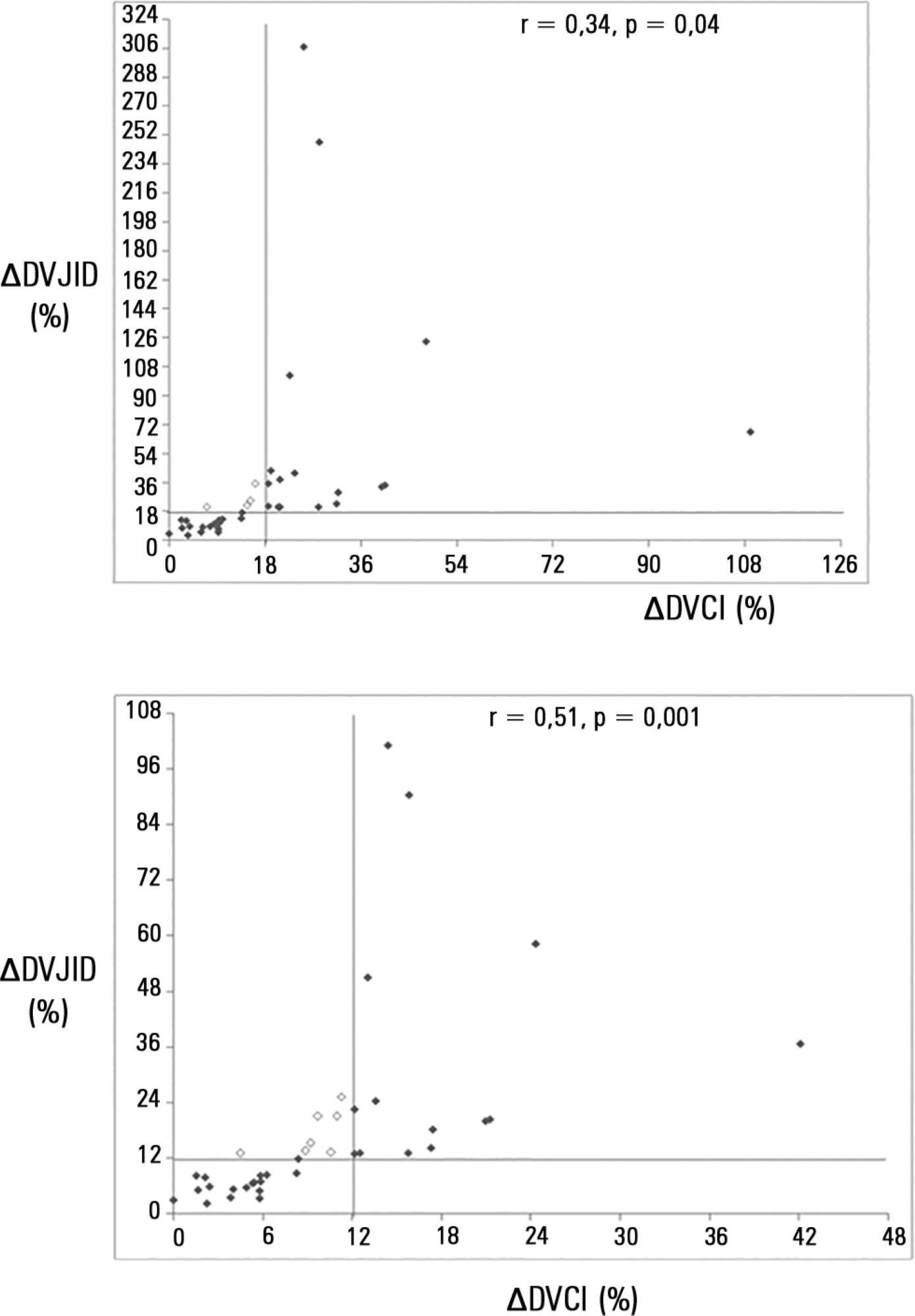
To investigate whether the respiratory variation of the inferior vena cava diameter (∆DIVC) and right internal jugular vein diameter (∆DRIJ) are correlated in mechanically ventilated patients.
This study was a prospective clinical analysis in an intensive care unit at a university hospital. Thirty-nine mechanically ventilated patients with hemodynamic instability were included. ∆DIVC and ∆DRIJ were assessed by echography. Vein distensibility was calculated as the ratio of (A) Dmax - Dmin/Dmin and (B) Dmax - Dmin/ mean of Dmax - Dmin and expressed as a percentage.
∆DIVC and ∆DRIJ were correlated by both methods: (A) r = 0.34, p = 0.04 and (B) r = 0.51, p = 0.001. Using 18% for ∆DIVC, indicating fluid responsiveness by method (A), 16 patients were responders and 35 measurements showed agreement (weighted Kappa = 0.80). The area under the ROC curve was 0.951 (95%CI 0.830 - 0.993; cutoff = 18.92). Using 12% for ∆DIVC, indicating fluid responsiveness by method (B), 14 patients were responders and 32 measurements showed agreement (weighted Kappa = 0.65). The area under the ROC curve was 0.903 (95%CI 0.765 - 0.973; cut-off value = 11.86).
The respiratory variation of the inferior vena cava and the right internal jugular veins are correlated and showed significant agreement. Evaluation of right internal jugular vein distensibility appears to be a surrogate marker for inferior vena cava vein distensibility for evaluating fluid responsiveness.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):44-50
DOI 10.5935/0103-507X.20150008
To assess the adherence to Infectious Disease Society of America/American Thoracic Society guidelines and the causes of lack of adherence during empirical antibiotic prescription in severe pneumonia in Latin America.
A clinical questionnaire was submitted to 36 physicians from Latin America; they were asked to indicate the empirical treatment in two fictitious cases of severe respiratory infection: community-acquired pneumonia and nosocomial pneumonia.
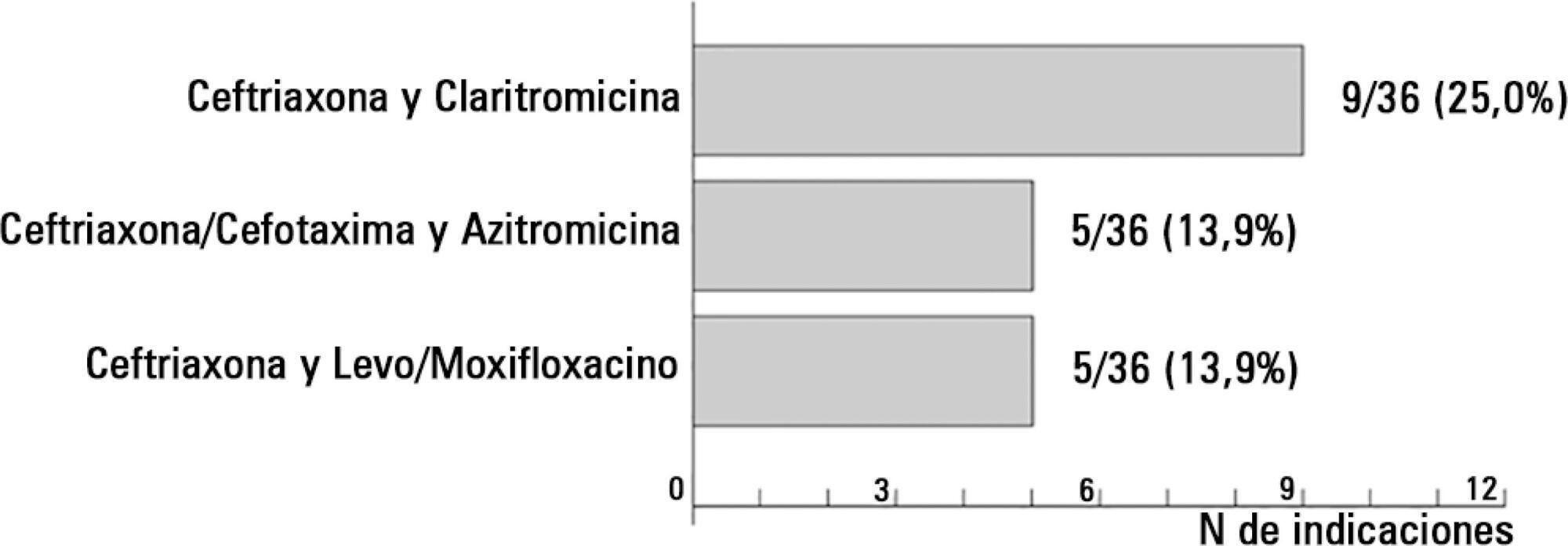
In the case of communityacquired pneumonia, 11 prescriptions of 36 (30.6%) were compliant with international guidelines. The causes for non-compliant treatment were monotherapy (16.0%), the unnecessary prescription of broad-spectrum antibiotics (40.0%) and the use of non-recommended antibiotics (44.0%).
The compliance rate with the Infectious Disease Society of America/American Thoracic Society guidelines in the community-acquired pneumonia scenario was 30.6%; the most frequent cause of lack of compliance was the indication of monotherapy. In the case of nosocomial pneumonia, the compliance rate with the guidelines was 2.8%, and the most important cause of non-adherence was lack of combined antipseudomonal therapy. If the use of monotherapy with an antipseudomonal antibiotic was considered the correct option, the treatment would be adequate in 100% of the prescriptions.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):51-56
DOI 10.5935/0103-507X.20150009
To assess the causes and factors associated with the death of patients between intensive care unit discharge and hospital discharge.
The present is a pilot, retrospective, observational cohort study. The records of all patients admitted to two units of a public/private university hospital from February 1, 2013 to April 30, 2013 were assessed. Demographic and clinical data, risk scores and outcomes were obtained from the Epimed monitoring system and confirmed in the electronic record system of the hospital. The relative risk and respective confidence intervals were calculated.
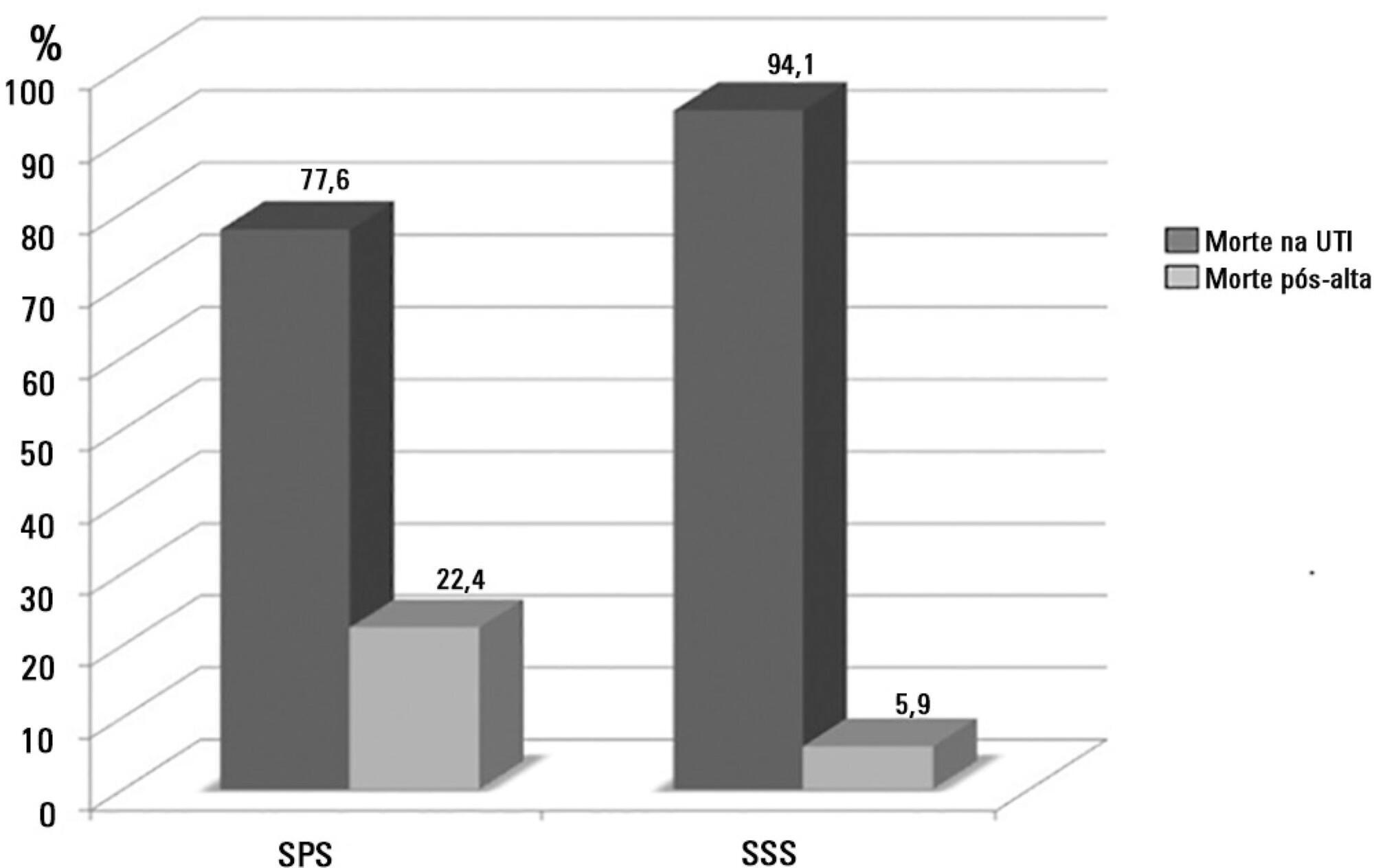
A total of 581 patients were evaluated. The mortality rate in the intensive care unit was 20.8% and in the hospital was 24.9%. Septic shock was the cause of death in 58.3% of patients who died after being discharged from the intensive care unit. Of the patients from the public health system, 73 (77.6%) died in the intensive care unit and 21 (22.4%) died in the hospital after being discharged from the unit. Of the patients from the Supplementary Health System, 48 (94.1%) died in the intensive care unit and 3 (5.9%) died in the hospital after being discharged from the unit (relative risk, 3.87%; 95% confidence interval, 1.21 - 12.36; p < 0.05). The post-discharge mortality rate was significantly higher in patients with intensive care unit hospitalization time longer than 6 days.
The main cause of death of patients who were discharged from the intensive care unit and died in the ward before hospital discharge was septic shock. Coverage by the public healthcare system and longer hospitalization time in the intensive care unit were factors associated with death after discharge from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):57-63
DOI 10.5935/0103-507X.20150010
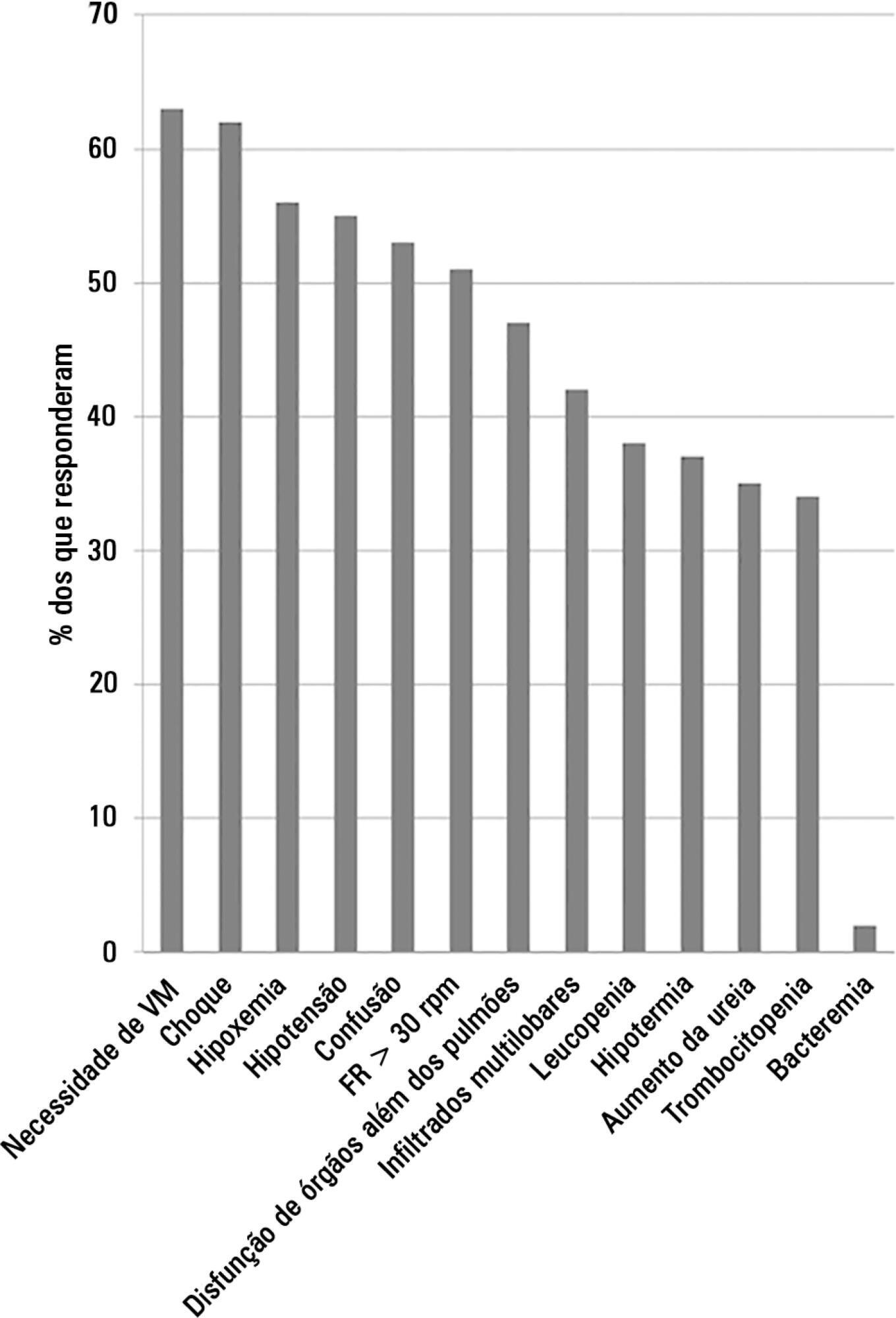
This study aimed to evaluate Brazilian physicians’ perceptions regarding the diagnosis, severity assessment, treatment and risk stratification of severe community-acquired pneumonia patients and to compare those perceptions to current guidelines.
We conducted a cross-sectional international anonymous survey among a convenience sample of critical care, pulmonary, emergency and internal medicine physicians from Brazil between October and December 2008. The electronic survey evaluated physicians’ attitudes towards the diagnosis, risk assessment and therapeutic interventions for patients with severe community-acquired pneumonia.
A total of 253 physicians responded to the survey, with 66% from Southeast Brazil. The majority (60%) of the responding physicians had > 10 years of medical experience. The risk assessment of severe community-acquired pneumonia was very heterogeneous, with clinical evaluation as the most frequent approach. Although blood cultures were recognized as exhibiting a poor diagnostic performance, these cultures were performed by 75% of respondents. In contrast, the presence of urinary pneumococcal and Legionella antigens was evaluated by less than 1/3 of physicians. The vast majority of physicians (95%) prescribe antibiotics according to a guideline, with the combination of a 3rd/4th generation cephalosporin plus a macrolide as the most frequent choice.
This Brazilian survey identified an important gap between guidelines and clinical practice and recommends the institution of educational programs that implement evidence-based strategies for the management of severe community-acquired pneumonia.
Abstract
Rev Bras Ter Intensiva. 2015;27(1):64-71
DOI 10.5935/0103-507X.20150011
The aim of the present study was to assess the feasibility of the early implementation of a swallowing rehabilitation program in tracheostomized patients under mechanical ventilation with dysphagia.
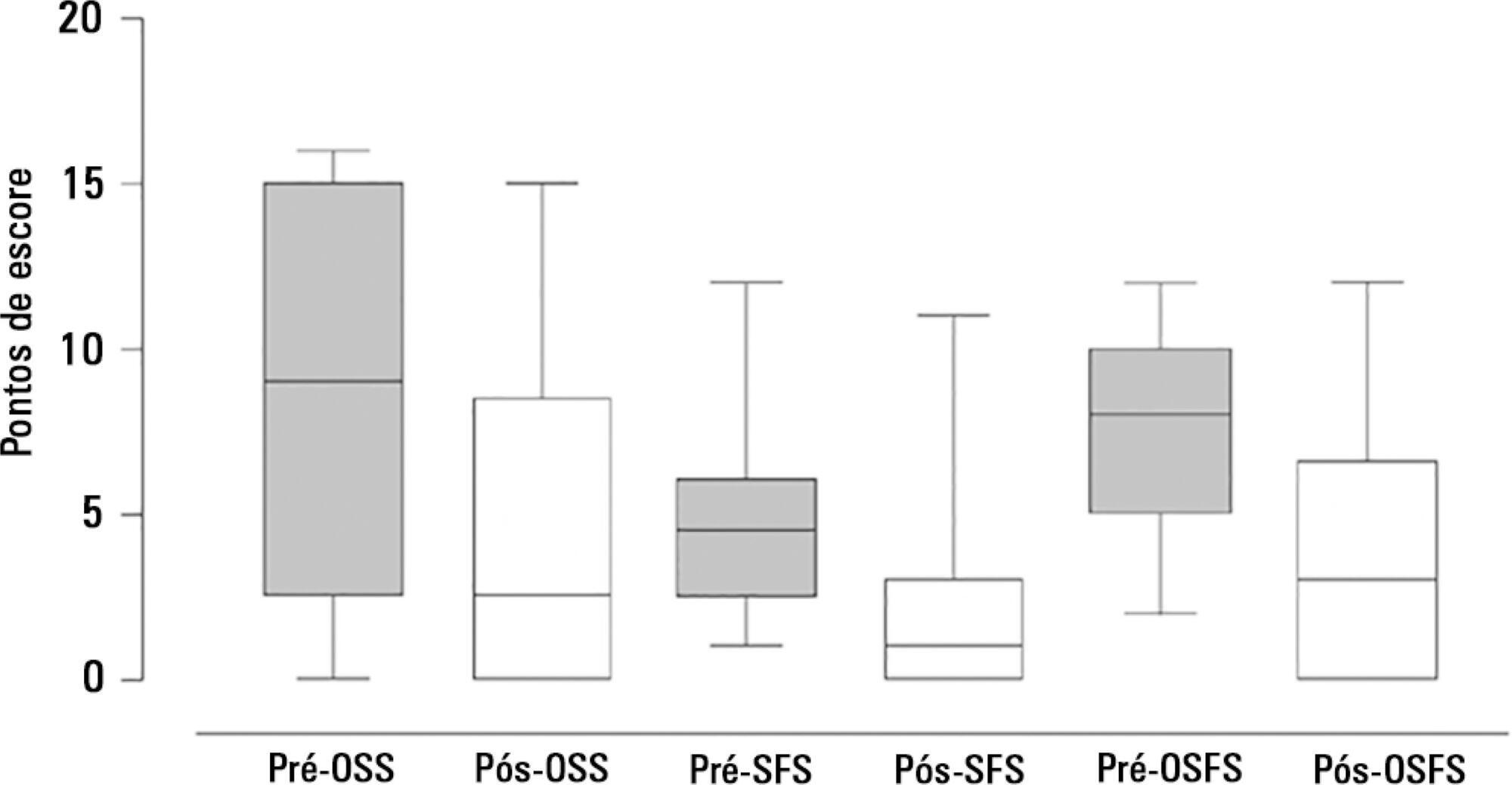
This prospective study was conducted in the intensive care units of a university hospital. We included hemodynamically stable patients under mechanical ventilation for at least 48 hours following 48 hours of tracheostomy and with an appropriate level of consciousness. The exclusion criteria were previous surgery in the oral cavity, pharynx, larynx and/or esophagus, the presence of degenerative diseases or a past history of oropharyngeal dysphagia. All patients were submitted to a swallowing rehabilitation program. An oropharyngeal structural score, a swallowing functional score and an otorhinolaryngological structural and functional score were determined before and after swallowing therapy.
We included 14 patients. The mean duration of the rehabilitation program was 12.4 ± 9.4 days, with 5.0 ± 5.2 days under mechanical ventilation. Eleven patients could receive oral feeding while still in the intensive care unit after 4 (2 - 13) days of therapy. All scores significantly improved after therapy.
In this small group of patients, we demonstrated that the early implementation of a swallowing rehabilitation program is feasible even in patients under mechanical ventilation.