Abstract
Rev Bras Ter Intensiva. 2016;28(4):397-404
DOI 10.5935/0103-507X.20160073
To identify factors associated with maternal death in patients admitted to an intensive care unit.
A cross-sectional study was conducted in a maternal intensive care unit. All medical records of patients admitted from January 2012 to December 2014 were reviewed. Pregnant and puerperal women were included; those with diagnoses of hydatidiform mole, ectopic pregnancy, or anembryonic pregnancy were excluded, as were patients admitted for non-obstetrical reasons. Death and hospital discharge were the outcomes subjected to comparative analysis.
A total of 373 patients aged 13 to 45 years were included. The causes for admission to the intensive care unit were hypertensive disorders of pregnancy, followed by heart disease, respiratory failure, and sepsis; complications included acute kidney injury (24.1%), hypotension (15.5%), bleeding (10.2%), and sepsis (6.7%). A total of 28 patients died (7.5%). Causes of death were hemorrhagic shock, multiple organ failure, respiratory failure, and sepsis. The independent risk factors associated with death were acute kidney injury (odds ratio [OR] = 6.77), hypotension (OR = 15.08), and respiratory failure (OR = 3.65).
The frequency of deaths was low. Acute kidney injury, hypotension, and respiratory insufficiency were independent risk factors for maternal death.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):413-419
DOI 10.5935/0103-507X.20160074
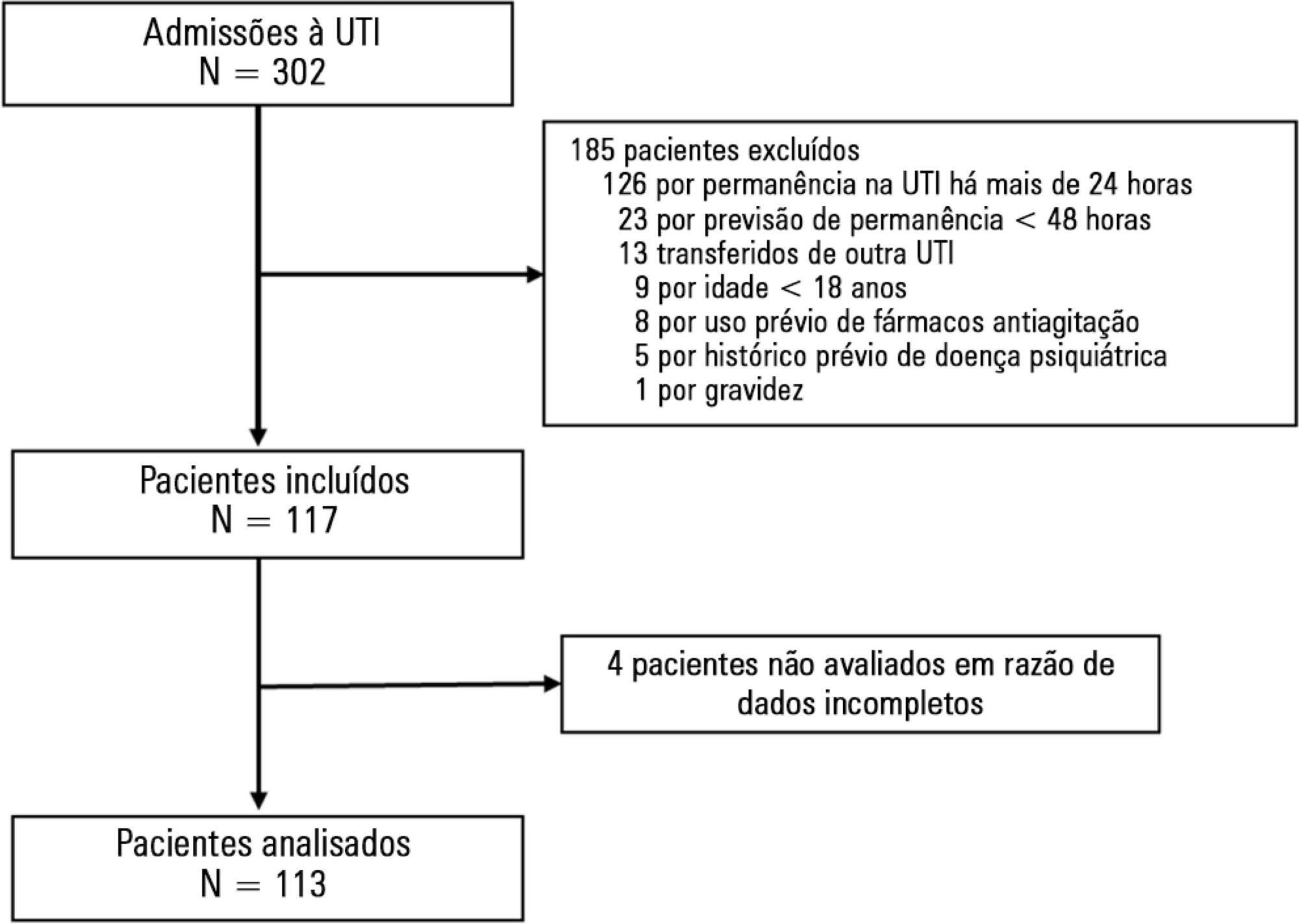
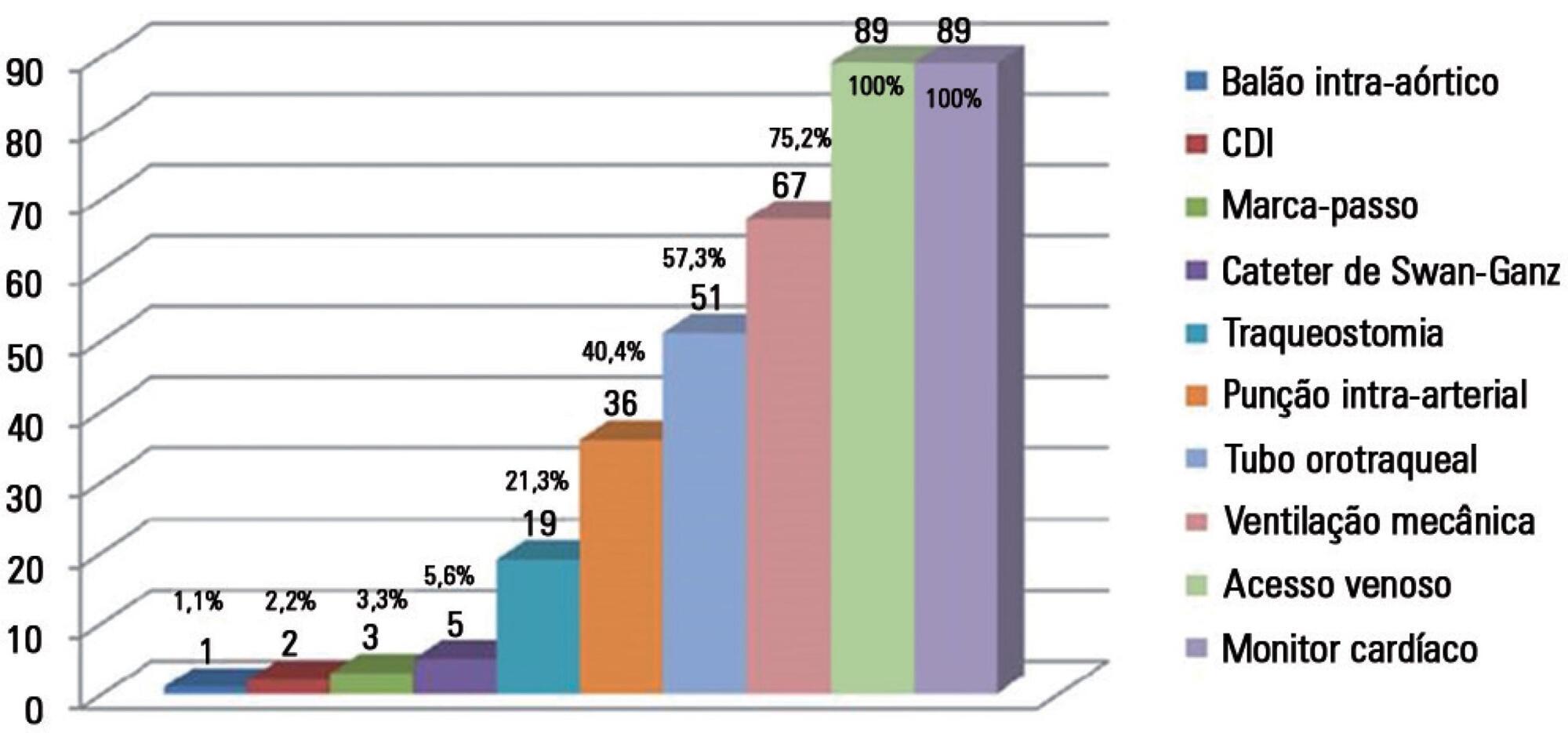
To evaluate the incidence of agitation in the first 7 days after intensive care unit admission, its risk factors and its associations with clinical outcomes.
This single-center prospective cohort study included all patients older than 18 years with a predicted stay > 48 hours within the first 24 hours of intensive care unit admission. Agitation was defined as a Richmond Agitation Sedation Scale score ≥ +2, an episode of agitation or the use of a specific medication recorded in patient charts.
Agitation occurred in 31.8% of the 113 patients. Multivariate analysis showed that delirium [OR = 24.14; CI95% 5.15 - 113.14; p < 0.001], moderate or severe pain [OR = 5.74; CI95% 1.73 - 19.10; p = 0.004], mechanical ventilation [OR = 10.14; CI95% 2.93 - 35.10; p < 0.001], and smoking habits [OR = 4.49; CI95% 1.33 - 15.17; p = 0.015] were independent factors for agitation, while hyperlactatemia was associated with a lower risk [OR = 0.169; CI95% 0.04 - 0.77; p = 0.021]. Agitated patients had fewer mechanical ventilation-free days at day 7 (p = 0.003).
The incidence of agitation in the first 7 days after admission to the intensive care unit was high. Delirium, moderate/severe pain, mechanical ventilation, and smoking habits were independent risk factors. Agitated patients had fewer ventilator-free days in the first 7 days.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):420-426
DOI 10.5935/0103-507X.20160075
To determine the incidence of afferent limb failure of the in-hospital Medical Emergency Team, characterizing it and comparing the mortality between the population experiencing afferent limb failure and the population not experiencing afferent limb failure.
A total of 478 activations of the Medical Emergency Team of Hospital Pedro Hispano occurred from January 2013 to July 2015. A sample of 285 activations was obtained after excluding incomplete records and activations for patients with less than 6 hours of hospitalization. The sample was divided into two groups: the group experiencing afferent limb failure and the group not experiencing afferent limb failure of the Medical Emergency Team. Both populations were characterized and compared. Statistical significance was set at p ≤ 0.05.
Afferent limb failure was observed in 22.1% of activations. The causal analysis revealed significant differences in Medical Emergency Team activation criteria (p = 0.003) in the group experiencing afferent limb failure, with higher rates of Medical Emergency Team activation for cardiac arrest and cardiovascular dysfunction. Regarding patient outcomes, the group experiencing afferent limb failure had higher immediate mortality rates and higher mortality rates at hospital discharge, with no significant differences. No significant differences were found for the other parameters.
The incidence of cardiac arrest and the mortality rate were higher in patients experiencing failure of the afferent limb of the Medical Emergency Team. This study highlights the need for health units to invest in the training of all healthcare professionals regarding the Medical Emergency Team activation criteria and emergency medical response system operations.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):427-435
DOI 10.5935/0103-507X.20160076
The objective of this study was to analyze the clinical profile of patients with in-hospital cardiac arrest using the Utstein style.
This study is an observational, prospective, longitudinal study of patients with cardiac arrest treated in intensive care units over a period of 1 year.
The study included 89 patients who underwent cardiopulmonary resuscitation maneuvers. The cohort was 51.6% male with a mean age 59.0 years. The episodes occurred during the daytime in 64.6% of cases. Asystole/bradyarrhythmia was the most frequent initial rhythm (42.7%). Most patients who exhibited a spontaneous return of circulation experienced recurrent cardiac arrest, especially within the first 24 hours (61.4%). The mean time elapsed between hospital admission and the occurrence of cardiac arrest was 10.3 days, the mean time between cardiac arrest and cardiopulmonary resuscitation was 0.68 min, the mean time between cardiac arrest and defibrillation was 7.1 min, and the mean duration of cardiopulmonary resuscitation was 16.3 min. Associations between gender and the duration of cardiopulmonary resuscitation (19.2 min in women versus 13.5 min in men, p = 0.02), the duration of cardiopulmonary resuscitation and the return of spontaneous circulation (10.8 min versus 30.7 min, p < 0.001) and heart disease and age (60.6 years versus 53.6, p < 0.001) were identified. The immediate survival rates after cardiac arrest, until hospital discharge and 6 months after discharge were 71%, 9% and 6%, respectively.
The main initial rhythm detected was asystole/bradyarrhythmia; the interval between cardiac arrest and cardiopulmonary resuscitation was short, but defibrillation was delayed. Women received cardiopulmonary resuscitation for longer periods than men. The in-hospital survival rate was low.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):436-443
DOI 10.5935/0103-507X.20160077
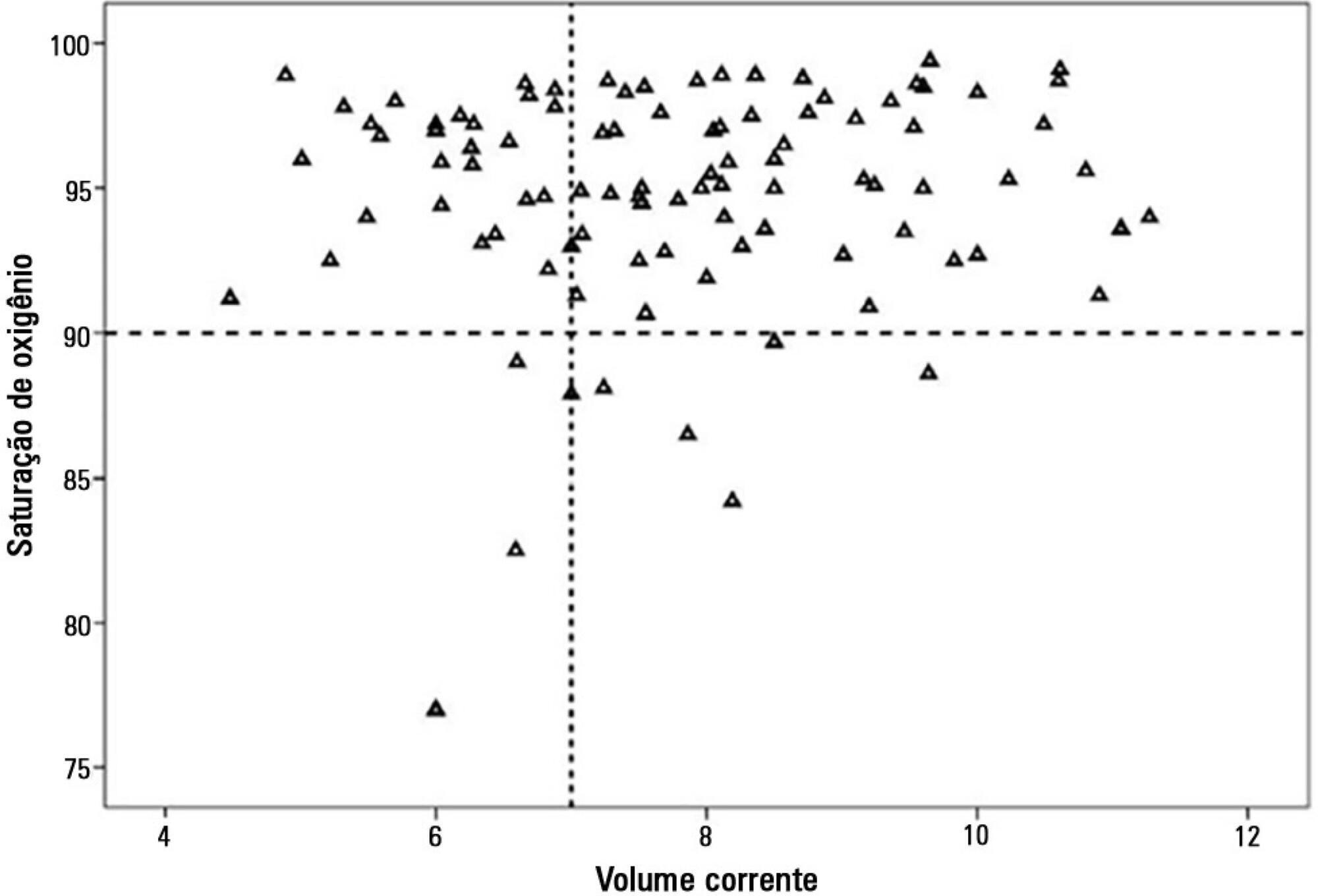
To evaluate the clinical course and respiratory parameters of mechanically ventilated children with cancer suffering from sepsis-related acute respiratory distress syndrome.
This 2-year prospective, longitudinal, observational cohort study enrolled 29 children and adolescents. Clinical data, measurements of blood gases and ventilation parameters were collected at four different time points. Fluctuations between measurements as well as differences in estimated means were analyzed by linear mixed models in which death within 28 days from the onset of acute respiratory distress syndrome was the primary endpoint.
There were 17 deaths within 28 days of acute respiratory distress syndrome onset and another 7 between 29 - 60 days. Only 5 patients survived for more than 60 days. Nine (31%) patients died as a direct consequence of refractory hypoxemia, and the others died of multiple organ failure and catecholamine-refractory shock. In 66% of the measurements, the tidal volume required to obtain oxygen saturation equal to or above 90% was greater than 7mL/kg. The estimated means of dynamic compliance were low and were similar for survivors and non-survivors but with a negative slope between the first and final measurements, accompanied by a negative slope of the tidal volume for non-survivors. Non-survivors were significantly more hypoxemic, with PaO2/FiO2 ratios showing lower estimated means and a negative slope along the four measurements. Peak, expiratory and mean airway pressures showed positive slopes in the non-survivors, who also had more metabolic acidosis.
In most of our children with cancer, sepsis and acute respiratory distress syndrome progressed with deteriorating ventilation indexes and escalating organic dysfunction, making this triad nearly fatal in children.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):444-451
DOI 10.5935/0103-507X.20160078
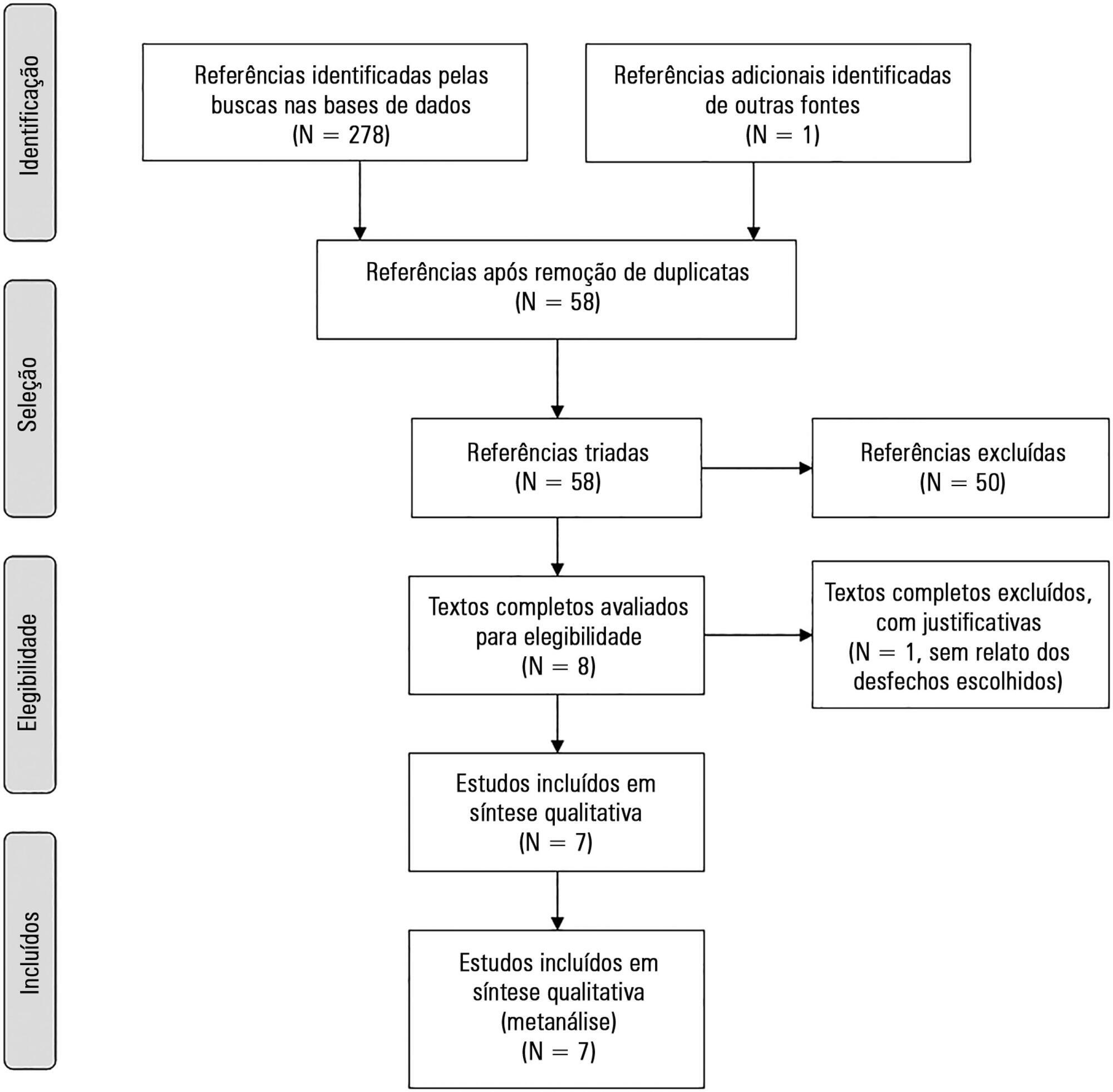
The aim of this study was to systematically review studies that compared a mild target sedation protocol with daily sedation interruption and to perform a meta-analysis with the data presented in these studies.
We searched Medline, Scopus and Web of Science databases to identify randomized clinical trials comparing sedation protocols with daily sedation interruption in critically ill patients requiring mechanical ventilation. The primary outcome was mortality in the intensive care unit.
Seven studies were included, with a total of 892 patients. Mortality in the intensive care unit did not differ between the sedation protocol and daily sedation interruption groups (odds ratio [OR] = 0.81; 95% confidence interval [CI] 0.60 - 1.10; I2 = 0%). Hospital mortality, duration of mechanical ventilation, intensive care unit and hospital length of stay did not differ between the groups either. Sedation protocols were associated with an increase in the number of days free of mechanical ventilation (mean difference = 6.70 days; 95%CI 1.09 - 12.31 days; I2 = 87.2%) and a shorter duration of hospital length of stay (mean difference = -5.05 days, 95%CI -9.98 - -0.11 days; I2 = 69%). There were no differences in regard to accidental extubation, extubation failure and the occurrence of delirium.
Sedation protocols and daily sedation interruption do not appear to differ in regard to the majority of analyzed outcomes. The only differences found were small and had a high degree of heterogeneity.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):235-239
DOI 10.5935/0103-507X.20150043
To evaluate the association between the in-hospital mortality of patients hospitalized due to respiratory diseases and the availability of intensive care units.
This retrospective cohort study evaluated a database from a hospital medicine service involving patients hospitalized due to respiratory non-terminal diseases. Data on clinical characteristics and risk factors associated with mortality, such as Charlson score and length of hospital stay, were collected. The following analyses were performed: univariate analysis with simple stratification using the Mantel Haenszel test, chi squared test, Student’s t test, Mann-Whitney test, and logistic regression.
Three hundred thirteen patients were selected, including 98 (31.3%) before installation of the intensive care unit and 215 (68.7%) after installation of the intensive care unit. No significant differences in the clinical and anthropometric characteristics or risk factors were observed between the groups. The mortality rate was 18/95 (18.9%) before the installation of the intensive care unit and 21/206 (10.2%) after the installation of the intensive care unit. Logistic regression analysis indicated that the probability of death after the installation of the intensive care unit decreased by 58% (OR: 0.42; 95%CI 0.205 -0.879; p = 0.021).
Considering the limitations of the study, the results suggest a benefit, with a decrease of one death per every 11 patients treated for respiratory diseases after the installation of an intensive care unit in our hospital. The results corroborate the benefits of the implementation of intensive care units in secondary hospitals.
Abstract
Rev Bras Ter Intensiva. 2015;27(3):240-246
DOI 10.5935/0103-507X.20150044
To determine the etiology and clinical disease progression variables of sepsis associated with the prognosis of patients admitted to a pediatric intensive care unit.
Prospective and retrospective case series. Data were collected from the medical records of patients diagnosed with sepsis who were admitted to the pediatric intensive care unit of a general hospital from January 2011 to December 2013. Bacteria were identified in blood and fluid cultures. Age, sex, vaccination schedule, comorbidities, prior antibiotic use, clinical data on admission, and complications during disease progression were compared in the survival and death groups at a 5% significance level.
A total of 115 patients, with a mean age of 30.5 months, were included in the study. Bacterial etiology was identified in 40 patients. Altered peripheral perfusion on admission and diagnosis of severe sepsis were associated with complications. A greater number of complications occurred in the group of patients older than 36 months (p = 0.003; odds ratio = 4.94). The presence of complications during hospitalization was associated with death (odds ratio = 27.7). The main etiological agents were Gram-negative bacteria (15/40), Staphylococcus aureus (11/40) and Neisseria meningitidis (5/40).
Gram-negative bacteria and Staphylococcus aureus predominated in the etiology of sepsis among children and adolescents admitted to an intensive care unit. The severity of sepsis and the presence of altered peripheral perfusion on admission were associated with complications. Moreover, the presence of complications was a factor associated with death.