Abstract
Rev Bras Ter Intensiva. 2016;28(1):62-69
DOI 10.5935/0103-507X.20160014
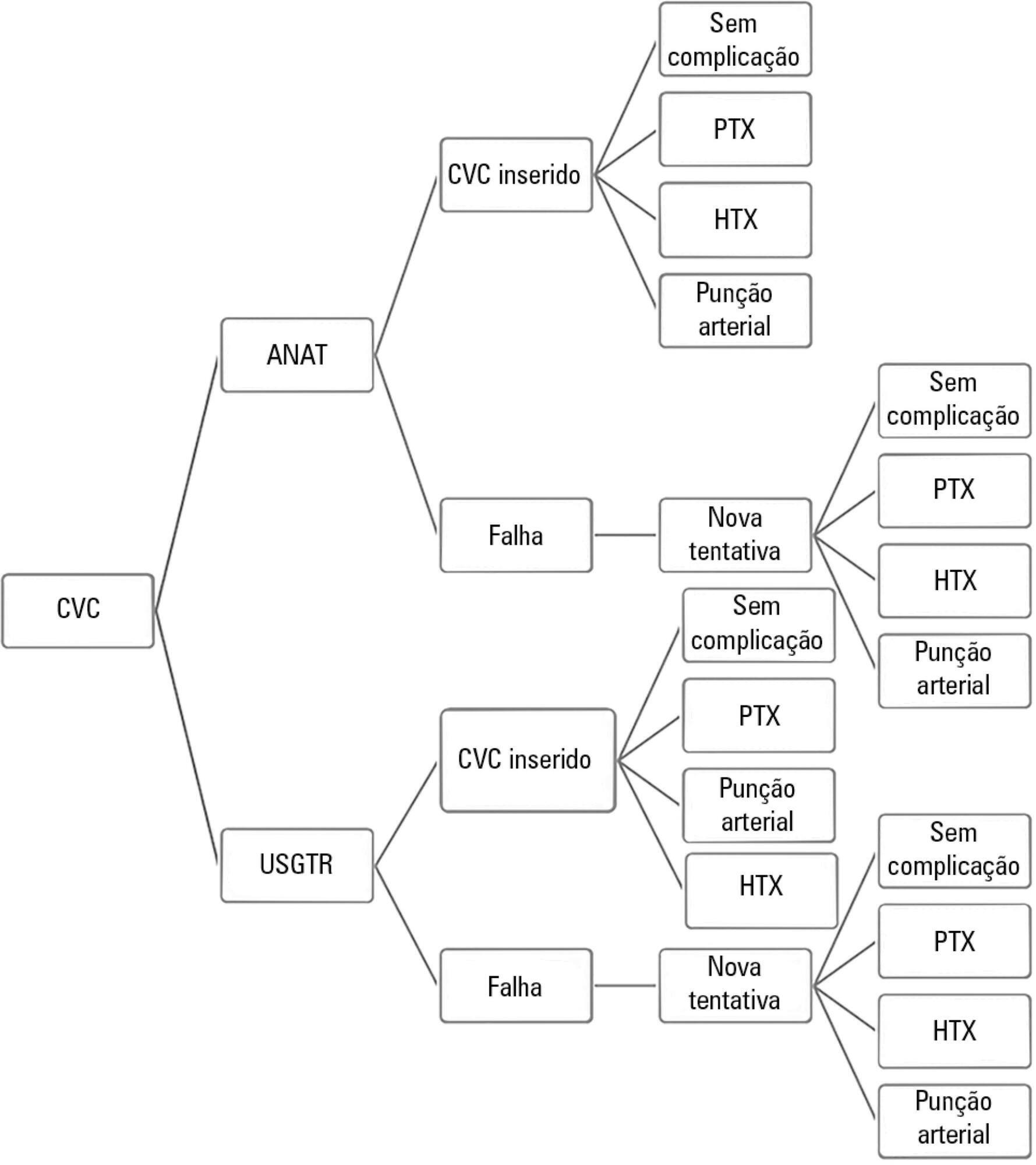
To evaluate the cost-effectiveness, from the funding body's point of view, of real-time ultrasound-guided central venous catheter insertion compared to the traditional method, which is based on the external anatomical landmark technique.
A theoretical simulation based on international literature data was applied to the Brazilian context, i.e., the Unified Health System (Sistema Único de Saúde - SUS). A decision tree was constructed that showed the two central venous catheter insertion techniques: real-time ultrasonography versus external anatomical landmarks. The probabilities of failure and complications were extracted from a search on the PubMed and Embase databases, and values associated with the procedure and with complications were taken from market research and the Department of Information Technology of the Unified Health System (DATASUS). Each central venous catheter insertion alternative had a cost that could be calculated by following each of the possible paths on the decision tree. The incremental cost-effectiveness ratio was calculated by dividing the mean incremental cost of real-time ultrasound compared to the external anatomical landmark technique by the mean incremental benefit, in terms of avoided complications.
When considering the incorporation of real-time ultrasound and the concomitant lower cost due to the reduced number of complications, the decision tree revealed a final mean cost for the external anatomical landmark technique of 262.27 Brazilian reals (R$) and for real-time ultrasound of R$187.94. The final incremental cost of the real-time ultrasound-guided technique was -R$74.33 per central venous catheter. The incremental cost-effectiveness ratio was -R$2,494.34 due to the pneumothorax avoided.
Real-time ultrasound-guided central venous catheter insertion was associated with decreased failure and complication rates and hypothetically reduced costs from the view of the funding body, which in this case was the SUS.
Abstract
Rev Bras Ter Intensiva. 2016;28(1):70-77
DOI 10.5935/0103-507X.20160015
Identify prognostic factors related to mortality and non-recovery of renal function.
A prospective single-center study was conducted at the intensive care medicine department of a university hospital between 2012 and 2015. Patients with acute kidney injury receiving continuous renal replacement therapy were included in the study. Clinical and analytical parameters were collected, and the reasons for initiation and discontinuation of renal replacement therapy were examined.
A total of 41 patients were included in the study, of whom 43.9% had sepsis. The median Simplified Acute Physiology Score II (SAPSII) was 56 and the mortality was 53.7%, with a predicted mortality of 59.8%. The etiology of acute kidney injury was often multifactorial (56.1%). Survivors had lower cumulative fluid balance (median = 3,600mL, interquartile range [IQR] = 1,175 - 8,025) than non-survivors (median = 12,000mL, IQR = 6,625 - 17,875; p = 0.004). Patients who recovered renal function (median = 51.0, IQR = 45.8 - 56.2) had lower SAPS II than those who do not recover renal function (median = 73, IQR = 54 - 85; p = 0.005) as well as lower fluid balance (median = 3,850, IQR = 1,425 - 8,025 versus median = 11,500, IQR = 6,625 - 16,275; p = 0.004).
SAPS II at admission and cumulative fluid balance during renal support therapy were risk factors for mortality and non-recovery of renal function among critically ill patients with acute kidney injury needing renal replacement therapy.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):341-347
DOI 10.5935/0103-507X.20160058
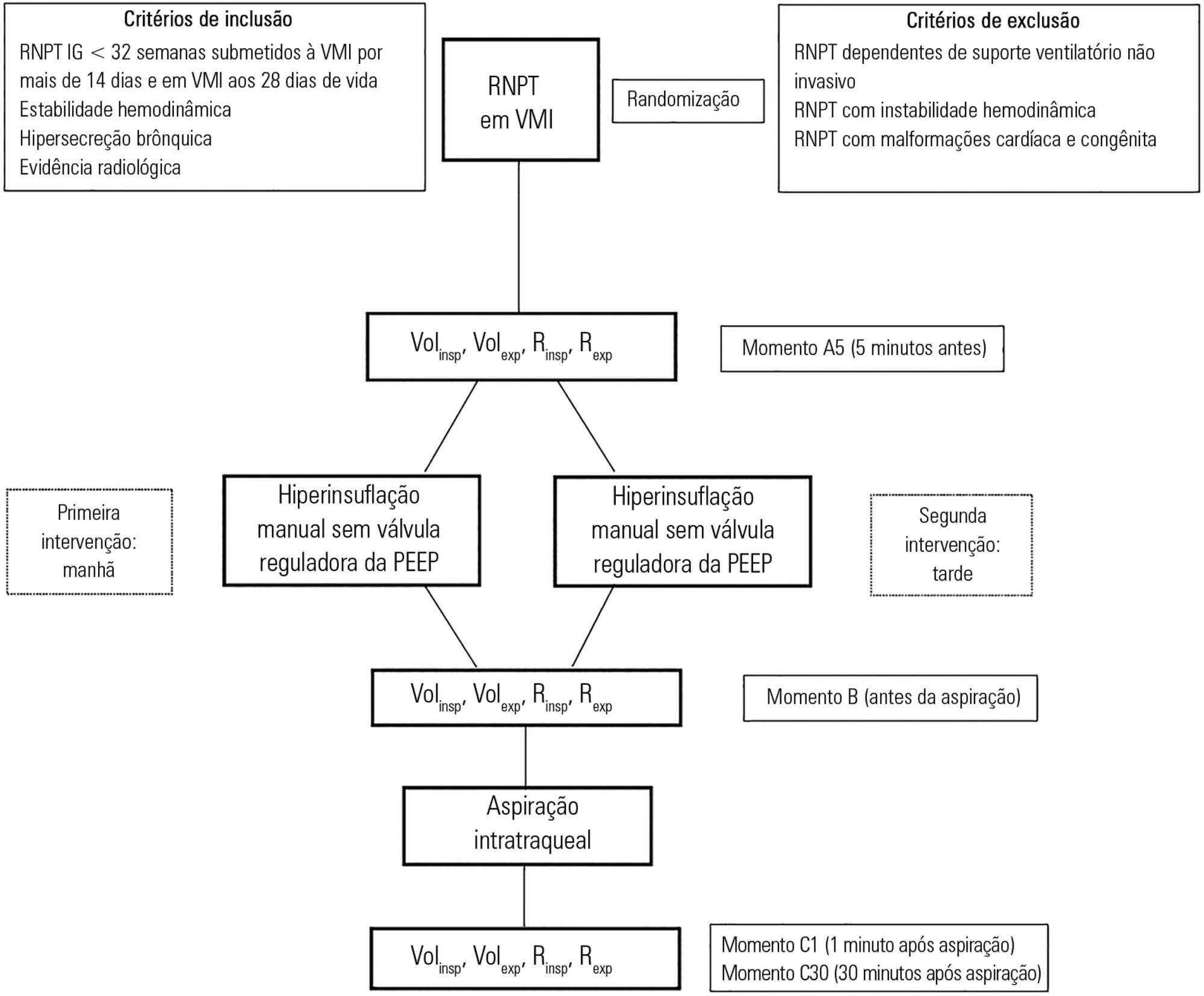
To assess the effects of manual hyperinflation, performed with a manual resuscitator with and without the positive end-expiratory pressure valve, on the respiratory function of preterm newborns under mechanical ventilation.
Cross-sectional study of hemodynamically stable preterm newborns with gestational age of less than 32 weeks, under mechanical ventilation and dependent on it at 28 days of life. Manual hyperinflation was applied randomly, alternating the use or not of the positive end-expiratory pressure valve, followed by tracheal aspiration for ending the maneuver. For nominal data, the two-tailed Wilcoxon test was applied at the 5% significance level and 80% power.
Twenty-eight preterm newborns, with an average birth weight of 1,005.71 ± 372.16g, an average gestational age of 28.90 ± 1.79 weeks, an average corrected age of 33.26 ± 1.78 weeks, and an average mechanical ventilation time of 29.5 (15 - 53) days, were studied. Increases in inspiratory and expiratory volumes occurred between time-points A5 (before the maneuver) and C1 (immediately after tracheal aspiration) in both the maneuver with the valve (p = 0.001 and p = 0.009) and without the valve (p = 0.026 and p = 0.001), respectively. There was also an increase in expiratory resistance between time-points A5 and C1 (p = 0.044).
Lung volumes increased when performing the maneuver with and without the valve, with a significant difference in the first minute after aspiration. There was a significant difference in expiratory resistance between the time-points A5 (before the maneuver) and C1 (immediately after tracheal aspiration) in the first minute after aspiration within each maneuver.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):270-277
DOI 10.5935/0103-507X.20160053
To estimate the prevalence of burnout in intensivist doctors working in adult, pediatric and neonatal intensive care units in five Brazilian capitals.
Descriptive epidemiological study with a random sample stratified by conglomerate with 180 intensivist doctors from five capitals representing the Brazilian geographic regions: Porto Alegre (RS), Sao Paulo (SP), Salvador (BA), Goiania (GO) and Belem (PA). A self-administered questionnaire examining sociodemographic data and the level of burnout was evaluated through the Maslach Burnout Inventory.
A total of 180 doctors were evaluated, of which 54.4% were female. The average age was 39 ± 8.1 years, 63.4% had specialization as the highest degree, 55.7% had up to 10 years of work experience in an intensive care unit, and 46.1% had the title intensive care specialist. Most (50.3%) had weekly workloads between 49 and 72 hours, and the most frequent employee type was salaried. High levels of emotional exhaustion, depersonalization and inefficacy were found (50.6%, 26.1% and 15.0%, respectively). The prevalence of burnout was 61.7% when considering a high level in at least one dimension and 5% with a high level in three dimensions simultaneously.
A high prevalence of burnout syndrome among intensivist doctors was observed. Strategies for the promotion and protection of health in these workers must be discussed and implemented in hospitals.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):301-309
DOI 10.5935/0103-507X.20160054
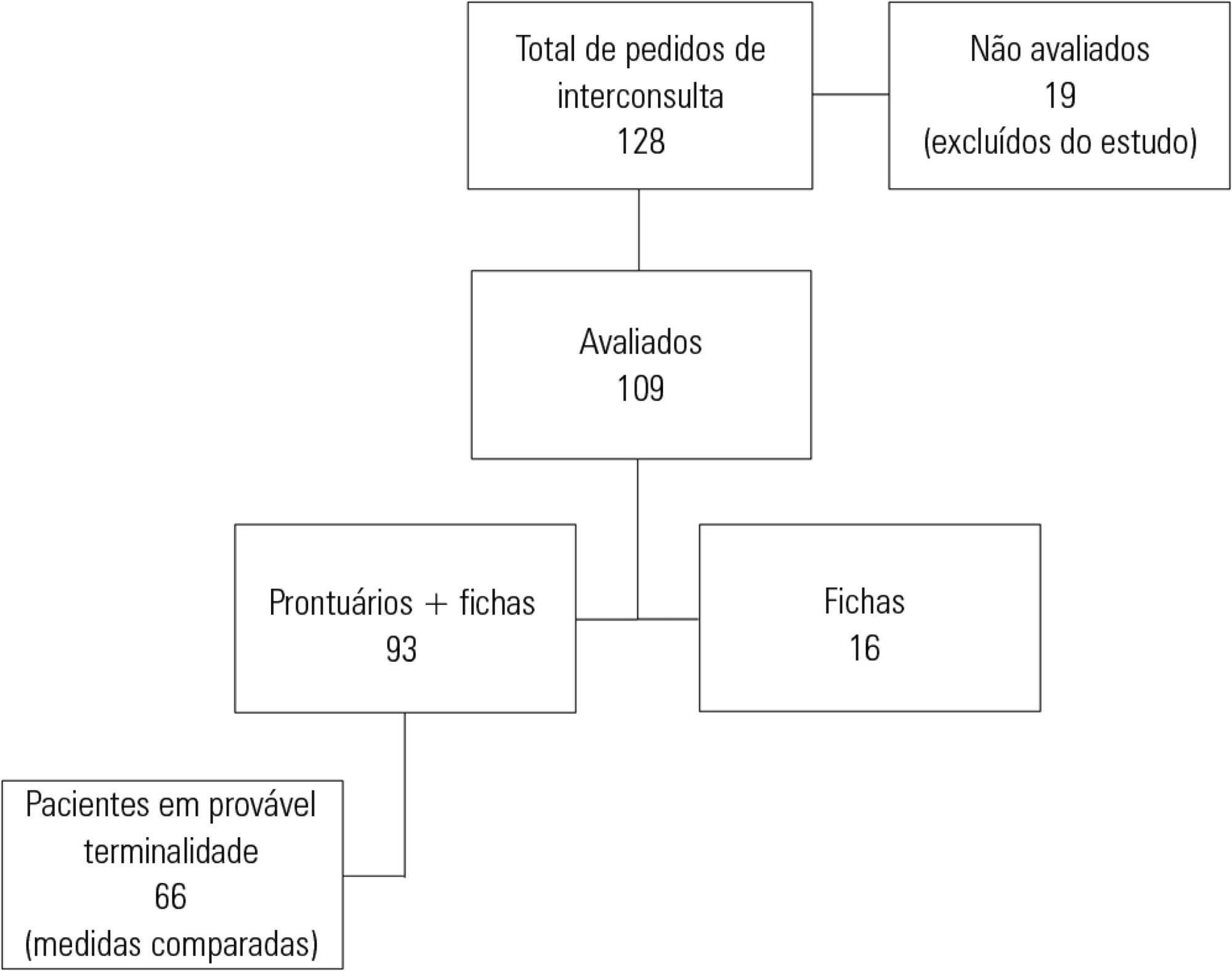
To describe the characteristics of patients with HIV/AIDS and to compare the therapeutic interventions and end-of-life care before and after evaluation by the palliative care team.
This retrospective cohort study included all patients with HIV/AIDS admitted to the intensive care unit of the Instituto de Infectologia Emílio Ribas who were evaluated by a palliative care team between January 2006 and December 2012.
Of the 109 patients evaluated, 89% acquired opportunistic infections, 70% had CD4 counts lower than 100 cells/mm3, and only 19% adhered to treatment. The overall mortality rate was 88%. Among patients predicted with a terminally ill (68%), the use of highly active antiretroviral therapy decreased from 50.0% to 23.1% (p = 0.02), the use of antibiotics decreased from 100% to 63.6% (p < 0.001), the use of vasoactive drugs decreased from 62.1% to 37.8% (p = 0.009), the use of renal replacement therapy decreased from 34.8% to 23.0% (p < 0.0001), and the number of blood product transfusions decreased from 74.2% to 19.7% (p < 0.0001). Meetings with the family were held in 48 cases, and 23% of the terminally ill patients were discharged from the intensive care unit.
Palliative care was required in patients with severe illnesses and high mortality. The number of potentially inappropriate interventions in terminally ill patients monitored by the palliative care team significantly decreased, and 26% of the patients were discharged from the intensive care unit.
Abstract
Rev Bras Ter Intensiva. 2016;28(4):380-386
DOI 10.5935/0103-507X.20160071
This study aimed to assess whether currently used dosages of vancomycin for treatment of serious gram-positive bacterial infections in intensive care unit patients provided initial therapeutic vancomycin trough levels and to examine possible factors associated with the presence of adequate initial vancomycin trough levels in these patients.
A prospective descriptive study with convenience sampling was performed. Nursing note and medical record data were collected from September 2013 to July 2014 for patients who met inclusion criteria. Eighty-three patients were included. Initial vancomycin trough levels were obtained immediately before vancomycin fourth dose. Acute kidney injury was defined as an increase of at least 0.3mg/dL in serum creatinine within 48 hours.
Considering vancomycin trough levels recommended for serious gram-positive infection treatment (15 - 20µg/mL), patients were categorized as presenting with low, adequate, and high vancomycin trough levels (35 [42.2%], 18 [21.7%], and 30 [36.1%] patients, respectively). Acute kidney injury patients had significantly greater vancomycin trough levels (p = 0.0055, with significance for a trend, p = 0.0023).
Surprisingly, more than 40% of the patients did not reach an effective initial vancomycin trough level. Studies on pharmacokinetic and dosage regimens of vancomycin in intensive care unit patients are necessary to circumvent this high proportion of failures to obtain adequate initial vancomycin trough levels. Vancomycin use without trough serum level monitoring in critically ill patients should be discouraged.
Abstract
Rev Bras Ter Intensiva. 2016;28(3):323-329
DOI 10.5935/0103-507X.20160055
To identify and stratify the main stressors for the relatives of patients admitted to the adult intensive care unit of a teaching hospital.
Cross-sectional descriptive study conducted with relatives of patients admitted to an intensive care unit from April to October 2014. The following materials were used: a questionnaire containing identification information and demographic data of the relatives, clinical data of the patients, and 25 stressors adapted from the Intensive Care Unit Environmental Stressor Scale. The degree of stress caused by each factor was determined on a scale of values from 1 to 4. The stressors were ranked based on the average score obtained.
The main cause of admission to the intensive care unit was clinical in 36 (52.2%) cases. The main stressors were the patient being in a state of coma (3.15 ± 1.23), the patient being unable to speak (3.15 ± 1.20), and the reason for admission (3.00 ± 1.27). After removing the 27 (39.1%) coma patients from the analysis, the main stressors for the relatives were the reason for admission (2.75 ± 1.354), seeing the patient in the intensive care unit (2.51 ± 1.227), and the patient being unable to speak (2.50 ± 1.269).
Difficulties in communication and in the relationship with the patient admitted to the intensive care unit were identified as the main stressors by their relatives, with the state of coma being predominant. By contrast, the environment, work routines, and relationship between the relatives and intensive care unit team had the least impact as stressors.